Narrow Therapeutic Index: What It Means and Why It Matters for Safe Medication Use
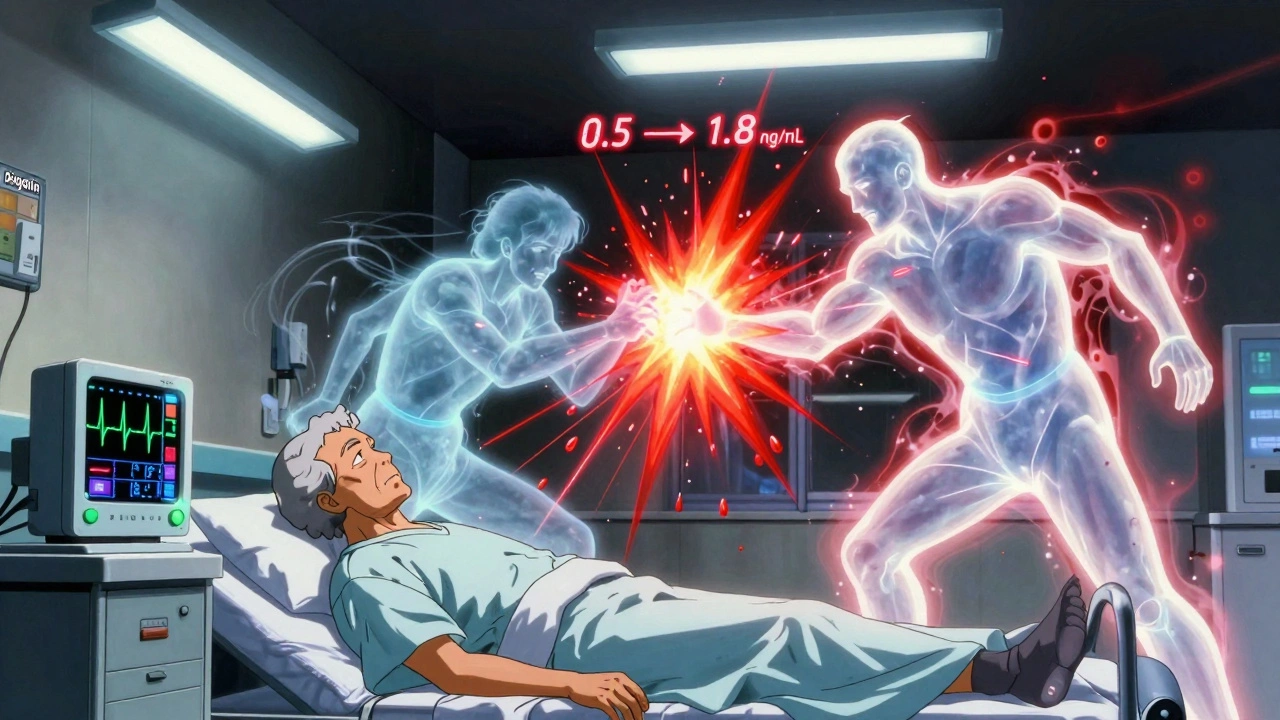
When a drug has a narrow therapeutic index, a small range between the effective dose and the toxic dose. Also known as low therapeutic index, it means even a tiny mistake in dosing can turn a life-saving medicine into a dangerous one. This isn’t about bad drugs—it’s about precision. Some of the most common and critical medications fall into this category: lithium for bipolar disorder, warfarin for blood clots, digoxin for heart rhythm, and phenytoin for seizures. These aren’t optional treatments—they’re essential. But they demand attention.
Why does this matter? Because your body doesn’t handle them like regular pills. A little too much lithium, and you get tremors, confusion, or kidney damage. A slight dip in warfarin, and you risk a stroke. Too much phenytoin, and your nervous system shuts down. These aren’t rare side effects—they’re predictable risks when monitoring isn’t tight. That’s why doctors and pharmacists track blood levels, check for interactions, and adjust doses slowly. It’s not guesswork. It’s science. And it’s why drugs with a narrow therapeutic index often come with warnings that feel overcautious—because they’re not.
These drugs don’t play well with others. Diuretics can spike lithium levels. NSAIDs can do the same. Even something as simple as changing your salt intake or starting a new antibiotic can throw off the balance. That’s why so many posts here focus on drug interactions, medication reviews, and patient education. You’ll find guides on how to safely start allopurinol, why ginkgo biloba can bleed when mixed with blood thinners, and how NSAIDs and diuretics dangerously raise lithium toxicity risk. You’ll see how pharmacists report generic drug problems when bioequivalence isn’t perfect, and why older adults are especially vulnerable because their bodies process drugs differently.
This isn’t just about pills. It’s about systems. It’s about school nurses double-checking pediatric doses, insurers pushing for generics without understanding the risks, and pharmacies ensuring every batch of medication meets strict sourcing standards. It’s about knowing when a generic isn’t interchangeable—not because it’s fake, but because the fillers or release rates change how your body absorbs it. That’s why excipients matter. That’s why the Five Rights aren’t just a checklist—they’re a lifeline.
If you’re taking one of these drugs, or care for someone who is, you need to know the signs. Dizziness, nausea, confusion, irregular heartbeat, unusual bruising—these aren’t just side effects. They’re warning signals. And you don’t have to wait for your doctor to notice them. You can ask for blood tests. You can ask for easy-open bottles if you’re on multiple meds. You can ask if your pharmacist has flagged any interactions. You’re not just a patient—you’re part of the safety team.