Medication Heartburn Risk Calculator
See how your medications might be causing heartburn and get personalized tips to reduce risk.
Which Medications Are You Taking?
15-30% risk of heartburn
12% risk of pill-induced esophagitis
10-20% risk of heartburn
25-30% risk of heartburn
20-30% risk of heartburn
5-10% risk of esophageal injury
15-20% risk of esophageal irritation
Personalized Tips
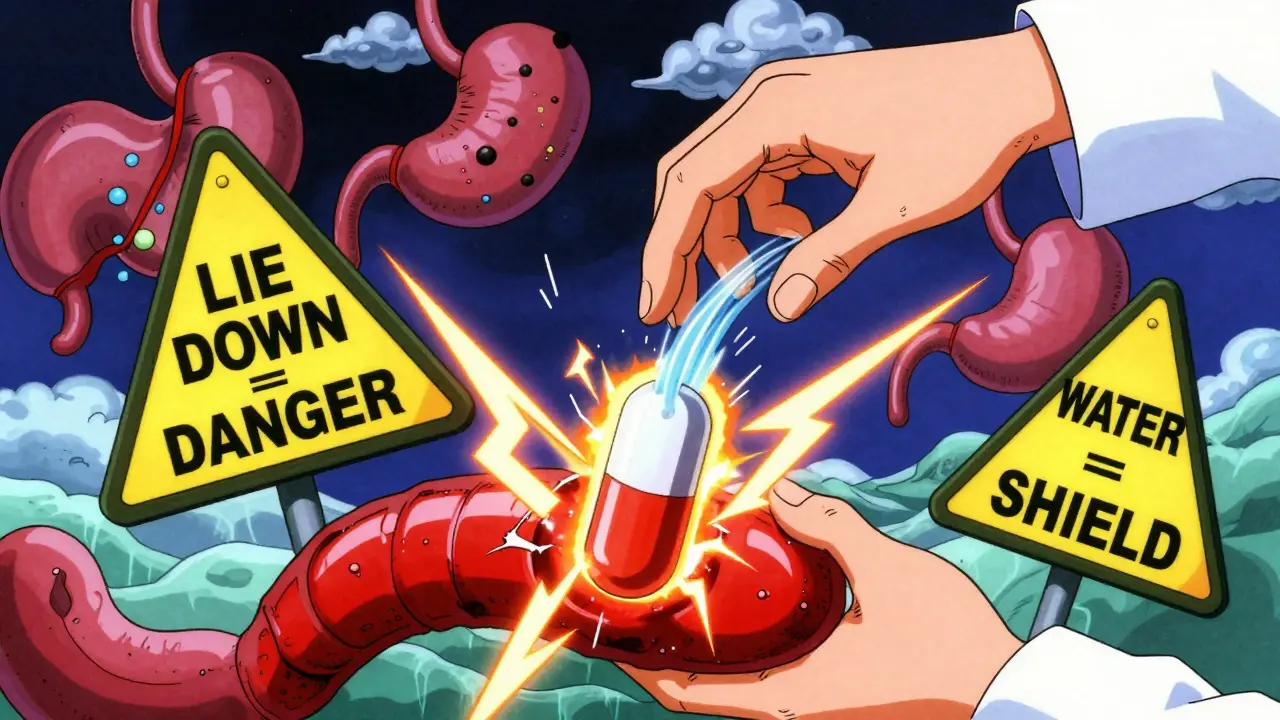
- Take all medications with a full glass of water
- Stay upright for at least 30 minutes after taking medications
- Take NSAIDs with food
Many people take medications every day without thinking about how they might be hurting their stomach. But if you’ve ever felt that burning sensation behind your breastbone after popping a pill, or had your stomach churn for hours afterward, you’re not alone. About 1 in 5 people on common prescriptions like ibuprofen, antibiotics, or diabetes meds experience heartburn or an upset stomach because of their drugs-not because of what they ate, but because of the medicine itself.
Why Your Pills Are Causing Heartburn
It’s not magic. It’s chemistry. Many medications directly irritate the lining of your esophagus or stomach, or they mess with the muscle that keeps stomach acid where it belongs-the lower esophageal sphincter (LES). When that muscle relaxes too much, acid flows back up. That’s heartburn.Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin are the biggest offenders. They block a protective enzyme in your stomach called COX-1. Without it, your stomach lining gets thin and vulnerable. Studies show 20-30% of people who take ibuprofen regularly get heartburn. For aspirin, it’s 15-25%. That’s not rare. That’s common.
Then there are antibiotics. Doxycycline, a tetracycline, is notorious. If you swallow it with just a sip of water and lie down right after, it can stick to your esophagus like glue. That causes chemical burns. Up to 12% of people who don’t follow the rules get pill-induced esophagitis-sometimes with ulcers. And it happens fast. Symptoms often show up within 2-4 hours.
Other culprits? Calcium channel blockers like amlodipine (used for high blood pressure) relax the LES, letting acid rise. Theophylline for asthma weakens that same muscle by 30-50%. Even metformin, the most common diabetes drug, triggers nausea and heartburn in 20-30% of new users. And bisphosphonates like alendronate? If you don’t take them right, they can cause serious, even life-threatening, esophageal damage.
Which Medications Are Most Likely to Cause Problems?
Not all pills are equal when it comes to stomach trouble. Here’s what the data says about the worst offenders and how they compare:
| Medication Class | Common Examples | Heartburn/Upset Stomach Rate | Key Risk Factor |
|---|---|---|---|
| NSAIDs | Ibuprofen, Aspirin, Naproxen | 15-30% | Stomach lining damage from COX-1 inhibition |
| Tetracycline Antibiotics | Doxycycline | 12% | Pill stuck in esophagus (pill-induced esophagitis) |
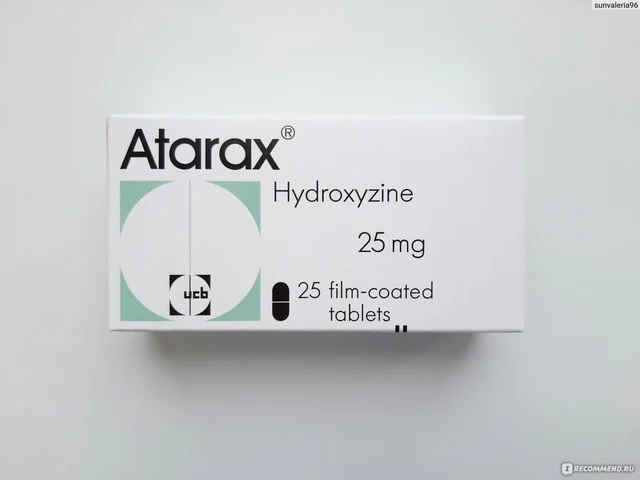
| Calcium Channel Blockers | Amlodipine, Nifedipine | 10-20% | Relaxes lower esophageal sphincter |
| Asthma Medications | Theophylline | 25-30% | Weakens LES pressure significantly |
| Diabetes Medication | Metformin | 20-30% | GI irritation-often improves after 2-4 weeks |
| Bisphosphonates | Alendronate (Fosamax) | 5-10% | Severe esophageal injury if not taken upright |
| Potassium Chloride | K-Dur | 15-20% | Direct irritation of esophagus |
Notice something? The worst risks aren’t always the most common. NSAIDs affect more people overall, but bisphosphonates and doxycycline can cause far more serious damage if taken wrong. That’s why how you take your pill matters just as much as which one you take.
How to Take Pills Without Hurting Your Stomach
You don’t have to stop your meds to stop the heartburn. There are simple, proven steps that cut risk dramatically.
- Take everything with a full glass of water (8 oz). This isn’t just advice-it’s medical protocol. For doxycycline and bisphosphonates, drinking a full glass reduces esophagitis risk by 60-70%. Water flushes the pill down before it has time to sit and burn.
- Stay upright for at least 30-60 minutes after taking your pill. Lying down right after is a recipe for trouble. Whether you’re taking a blood pressure pill or a bone drug, stay standing or sitting. Walk around if you can. This prevents 80-90% of pill-induced esophagitis cases.
- Take NSAIDs with food. Eating before or with ibuprofen or aspirin reduces stomach irritation by 40-50%. A sandwich, a bowl of oatmeal, even a banana helps. Don’t take them on an empty stomach.
- Don’t crush or open capsules unless told to. Delayed-release or enteric-coated pills are designed to dissolve in the intestine, not the stomach or esophagus. Crushing them defeats the purpose.
- Avoid alcohol and caffeine around medication time. Both relax the LES and increase acid. Add them to NSAIDs or antibiotics, and you’re stacking the deck against your stomach.
And here’s something many people don’t know: if you’re on metformin, your stomach issues might go away on their own. About 60-70% of new users see symptoms fade within 2-4 weeks. That’s not a sign to quit-it’s a sign to wait it out.
When to Use Antacids or Acid Reducers
Over-the-counter help can work-but only if you use it right.
Antacids like Tums or Rolaids can help if taken 30 minutes before your NSAID. They neutralize acid right away. Studies show this cuts heartburn by 30-40%. But they’re short-term. They don’t fix the root problem.
Proton pump inhibitors (PPIs) like omeprazole are stronger. For people on long-term NSAIDs who have a history of ulcers or are over 60, doctors often prescribe a PPI at the same time. This cuts ulcer risk by 70-80%. That’s huge. But don’t start PPIs without talking to your doctor. Long-term use has its own risks, including nutrient deficiencies and increased infection risk.
Don’t use PPIs just because you feel a little heartburn after a pill. Use them when the risk is high-and only under medical guidance.
Red Flags: When to Call Your Doctor Immediately
Most medication-related heartburn is annoying, not dangerous. But some signs mean something serious is happening.
- Chest pain that feels like pressure or tightness. Not all heartburn is harmless. If it feels like a heart attack, get checked.
- Difficulty swallowing. If food feels stuck or you feel pain going down, your esophagus may be damaged.
- Blood in vomit or stool. Black, tarry stools or bright red blood are signs of bleeding. This can happen in 1-2% of long-term NSAID users.
- Unexplained weight loss or persistent nausea. These can signal deeper GI damage or even Barrett’s esophagus, a condition that raises cancer risk.
If you have any of these, don’t wait. Call your doctor. Don’t assume it’s just from your pill. It might be, but it might be something worse.

New Solutions and What’s Coming
The good news? Pharma companies are listening.
In 2022, the FDA approved a new delayed-release version of doxycycline that’s less likely to stick in your esophagus. It reduces exposure by 40-50%. New coated NSAIDs are in trials and show 30-35% fewer stomach issues.
Hospitals and clinics are starting to use smart systems that flag when a patient is on multiple high-risk drugs. One 2024 study showed these systems catch dangerous combinations with 85-90% accuracy.
Future options? Genetic testing to find people who metabolize NSAIDs poorly (about 1 in 5 Caucasians have this gene). Or pills that go through the skin instead of the gut-transdermal patches and sublingual forms are already in early testing.
But right now, the best solution isn’t new tech. It’s simple: take your pills the right way, stay upright, drink water, and talk to your doctor before stopping anything.
Don’t Quit Your Meds-Fix the Problem
One of the biggest mistakes people make? Stopping their medication because of heartburn. Around 7% of patients quit life-saving drugs like blood pressure pills or diabetes meds over stomach issues. That’s dangerous.
High blood pressure without meds? Risk of stroke goes up. Diabetes uncontrolled? Nerve damage, kidney failure, vision loss follow. A little heartburn isn’t worth that.
Instead of quitting, ask your doctor: "Is there a different form of this drug? Can I take it with food? Should I use a PPI?" There’s almost always a way to keep the benefit and reduce the side effect.
Medication-induced heartburn isn’t something you just have to live with. It’s a solvable problem. And with the right steps, you can take your pills safely-without the burn.
Can I take ibuprofen with food to avoid heartburn?
Yes. Taking ibuprofen with food reduces stomach irritation by 40-50%. A small meal or even a snack like crackers or yogurt helps protect your stomach lining. Avoid taking it on an empty stomach, especially if you’re using it regularly.
Why does doxycycline cause esophagitis?
Doxycycline is acidic and can stick to the esophagus if not washed down properly. When it sits there, it causes chemical burns. Taking it with a full glass of water and staying upright for 60 minutes prevents this in nearly all cases. Never lie down right after taking it.
Is metformin heartburn permanent?
No. For most people, metformin-related nausea and heartburn fade within 2-4 weeks as the body adjusts. Taking it with meals helps. If symptoms last longer than a month, talk to your doctor about switching to an extended-release version.
Can I use antacids every day with my medication?
Occasional use is fine, but daily antacids aren’t a long-term fix. They don’t reduce acid production-they just neutralize it briefly. For chronic heartburn from meds, proton pump inhibitors (PPIs) are more effective. But only use PPIs under a doctor’s supervision due to potential side effects with long-term use.
Should I stop my blood pressure pill if it gives me heartburn?
No. Calcium channel blockers like amlodipine can cause heartburn, but stopping them suddenly can raise your blood pressure dangerously. Talk to your doctor instead. They may switch you to a beta blocker, which causes heartburn in only 5-10% of users, or add a PPI to protect your stomach.
What’s the safest way to take bisphosphonates like Fosamax?
Take it first thing in the morning on an empty stomach with a full glass of plain water. Stay upright for at least 60 minutes. Don’t eat, drink, or take other meds during that time. Wait 30 minutes before eating. Skipping these steps increases risk of serious esophageal injury by up to 10 times.
What to Do Next
Start by listing every medication you take daily. Then ask yourself: "When I take this, do I feel heartburn or stomach upset?" If yes, note the timing-right after? An hour later?
Next, check the instructions. Are you taking it with enough water? Are you lying down too soon? Are you taking NSAIDs on an empty stomach?
Finally, schedule a quick chat with your doctor or pharmacist. Don’t wait for symptoms to get worse. Say: "I’ve been having heartburn since I started [medication]. Are there ways to reduce this without stopping the drug?"
Most of the time, the answer will be yes. And you won’t have to choose between staying healthy and feeling better.







11 Comments
Praseetha Pn
Jan 17 2026Okay but have you ever heard that Big Pharma *wants* you to have heartburn? It’s not an accident-they make the pills to irritate your gut so you’ll buy their PPIs on top. That’s why they don’t fix the damn coating on doxycycline until 2022. They were making bank off your burning esophagus for decades. And don’t even get me started on how they hide the metformin nausea data in tiny footnotes. Wake up, sheeple.
rachel bellet
Jan 19 2026There’s a fundamental flaw in your risk stratification. You’re conflating incidence with clinical significance. While NSAIDs have a 30% GI upset rate, the absolute risk of ulceration is <0.5% in healthy adults under 60. Meanwhile, bisphosphonates carry a 0.1% risk of esophageal perforation-but that’s still 10x higher than placebo. Your data is statistically noisy but clinically misleading. Also, ‘full glass of water’ is undefined. 8 oz? 12 oz? FDA guidelines specify 240 mL minimum. Precision matters.
Selina Warren
Jan 20 2026Y’all are overcomplicating this. Your body is screaming at you. If your pill gives you heartburn, it’s not ‘just’ a side effect-it’s your system saying ‘this doesn’t belong here.’ I used to take ibuprofen like candy until I started drinking a whole glass of water, standing up, and eating a banana first. Boom. No more burn. No magic. Just respect your gut. You wouldn’t shove a rock down your throat and wonder why it hurt. Why treat your stomach like a trash can?
Robert Davis
Jan 21 2026Interesting. I’ve been taking metformin for 3 years. Never had an issue. Maybe I’m just lucky? Or maybe I’m one of those people who metabolizes it differently. I’ve noticed that people who complain about side effects are often the same ones who read every drug label and then assume the worst. Maybe the anxiety is part of the problem.
Jake Moore
Jan 23 2026For anyone on bisphosphonates: I’m a pharmacist and I’ve seen people take Fosamax with coffee or juice and then lie down to scroll TikTok. That’s how you end up in the ER. The protocol is non-negotiable: plain water, upright for 60 min, nothing else for 30 min after. Even a sip of tea breaks the rule. I’ve had patients who swore they ‘did it right’-turns out they drank 4 oz of water and sat on the couch. Don’t be that person. Your bones need this. Your esophagus needs this.
Joni O
Jan 24 2026OMG I JUST REALIZED I’VE BEEN TAKING MY AMLODIPINE WITH A SIP OF WATER AND THEN LAYING BACK ON THE COUCH 😭 I’M SO SORRY MY ESOPHAGUS. I’M GOING TO START DOING IT RIGHT TOMORROW. THANK YOU FOR THIS POST. I FEEL SO MUCH LESS ALONE NOW. I THOUGHT I WAS JUST WEIRD FOR GETTING HEARTBURN FROM BP MEDS.
Max Sinclair
Jan 25 2026Great breakdown. I appreciate how you distinguished between common irritation and serious injury. Many people don’t realize that 10-20% heartburn from amlodipine doesn’t mean you need to stop it-it means you need to adjust your habits. I’ve had patients switch to a beta blocker, take a PPI for 6 weeks, and then taper off. The key is communication with your provider. Don’t self-diagnose, don’t self-discontinue. Just ask: ‘What’s the next best option?’
Nishant Sonuley
Jan 26 2026Let’s be real here. The whole ‘take with food’ advice for NSAIDs? That’s what your grandma told you in 1987. But here’s the kicker: modern enteric-coated aspirin doesn’t need it. And yet, we keep repeating the myth because it’s easier than updating guidelines. Meanwhile, people are taking ibuprofen with pizza and thinking they’re protected, when the real issue is the dose and duration. I’ve seen 800mg ibuprofen twice daily for 3 months cause ulcers in someone who ate steak with every dose. Food isn’t a shield-it’s a distraction. The real fix? Use the lowest effective dose for the shortest time. And if you’re on it daily, you should be on a PPI anyway. Period.
Emma #########
Jan 27 2026Thank you for writing this. I’ve been too scared to tell my doctor I’ve been skipping my metformin because of the nausea. I thought I was weak for not being able to handle it. But now I know it’s common and temporary. I’m going to try taking it with dinner instead of breakfast. And I’m not giving up. I deserve to be healthy without feeling like my stomach is on fire.
Andrew McLarren
Jan 28 2026While the recommendations presented are generally sound, I must emphasize the necessity of individualized risk assessment. The statistical prevalence of gastrointestinal adverse effects, while informative, does not account for comorbidities, concomitant medications, or physiological variables such as gastric pH, motility, or esophageal clearance kinetics. Furthermore, the assertion that ‘water flushes the pill down’ is an oversimplification of esophageal transit dynamics, which are governed by peristaltic wave propagation and bolus rheology. A more rigorous approach would incorporate pharmacokinetic modeling in lieu of heuristic advice.
Andrew Short
Jan 29 2026You’re all being naive. This isn’t about ‘taking pills correctly.’ It’s about pharmaceutical negligence. They know these drugs damage the GI tract. They know the real solution is reformulation. But why fix it when you can sell $300/month PPIs on top? The FDA approved that delayed-release doxycycline in 2022? Took them 40 years. And now they’re pushing ‘smart systems’ to flag dangerous combos-when they could’ve just made safer pills from the start. This isn’t patient care. It’s profit-driven harm. Stop blaming the user. Blame the system.