What Exactly Are Sleepwalking and Night Terrors?
Sleepwalking and night terrors are not just weird dreams or bad habits-they’re real medical events that happen during deep sleep. Both fall under a group of disorders called parasomnias, which are abnormal behaviors that occur while you’re asleep. Unlike nightmares, where you wake up scared and remember every detail, these episodes happen during deep, non-REM sleep. Most people have no memory of them at all.
Sleepwalking can look like someone getting out of bed, walking around the house, even opening cabinets or trying to leave. Night terrors are more intense: screaming, thrashing, rapid heartbeat, sweating, and extreme fear-often with eyes wide open but not really seeing anything. These aren’t tantrums or attention-seeking. They’re automatic brain responses during deep sleep.
They’re most common in kids between ages 3 and 8. About 1 in 5 children will sleepwalk at least once. Night terrors affect about 1 in 20 kids. Most outgrow them by puberty. But they don’t disappear in all cases. Around 1 in 25 adults still experience them, often linked to stress, sleep deprivation, or other sleep disorders like sleep apnea.
Why Do These Episodes Happen?
The brain doesn’t shut down fully during deep sleep. In sleepwalking and night terrors, part of the brain is still in deep sleep mode while another part is partially awake-like a computer stuck in hibernation but trying to run a program. This mismatch causes the body to move or react without conscious control.
These episodes almost always happen in the first third of the night, right after falling asleep, when slow-wave sleep is strongest. That’s why you rarely see them after midnight. They’re not caused by bad dreams or trauma. They’re triggered by things that increase deep sleep pressure: lack of sleep, irregular sleep schedules, fever, or even sleeping in a new environment.
Genetics play a big role. If one parent had sleepwalking as a kid, their child has a 45% chance of doing it too. If both parents did, that jumps to 60%. Research in 2023 found a specific gene variant (DEC2) linked to familial sleepwalking with 87% accuracy in affected families.
Adult-onset parasomnias are a red flag. If someone starts sleepwalking or having night terrors after age 18, it could signal an underlying neurological issue, sleep apnea, or even a side effect of medication. That’s why doctors recommend evaluation if it begins in adulthood.
How Dangerous Are These Episodes?
The biggest risk isn’t the episode itself-it’s what happens during it. People sleepwalk into walls, down stairs, or outside. One study found 73% of families reported at least one injury from sleepwalking. Most are minor: bumps, cuts, bruises. But 8% have suffered fractures, and 5% have wandered into traffic or left the house entirely.
Night terrors are less physically risky because the person usually stays in bed. But the sheer intensity can be terrifying for witnesses. Heart rates spike to 120-140 beats per minute. Breathing becomes fast and shallow. Skin gets sweaty and flushed. It looks like a medical emergency-but it’s not. The person isn’t in danger from the episode itself, but they can hurt themselves if they thrash around or jump out of bed.
Parents often panic. They try to wake their child. That’s the worst thing to do. Trying to rouse someone during a night terror can make the episode last longer and cause confusion or aggression. The best move? Stay calm, gently guide them back to bed, and wait it out. They’ll settle down on their own.
First Step: Make the Bedroom Safe
Before anything else-medication, therapy, or sleep schedules-secure the environment. This isn’t optional. It’s non-negotiable.
- Lock all windows and exterior doors. Use alarms that sound when opened (cost: $20-$50).
- Remove sharp objects, glass tables, or anything breakable within 10 feet of the bed.
- Place a mattress on the floor if the person sleeps on a high bed. This cuts fall injuries by 75%.
- Install gates at the top of stairs.
- Keep keys, phones, and shoes out of reach.
One parent in Christchurch installed a door alarm after her 6-year-old walked out into the street at 2 a.m. She said, “It didn’t stop the episodes, but it stopped the panic.”
These safety steps work for kids and adults alike. You don’t need to be a genius to do them. You just need to be consistent.

Behavioral Fixes That Actually Work
Medication isn’t the first answer. In fact, most cases don’t need it at all. The most effective treatments are simple, low-tech, and free.
Scheduled Awakenings
This is the #1 recommended method for sleepwalking. It works for about 70-80% of cases.
Here’s how: Figure out when the episode usually happens. Most occur 90-120 minutes after falling asleep. Set an alarm for 15-30 minutes before that time. When it goes off, gently wake the person up. Keep them fully awake for 5-10 minutes-talk to them, have them sit up, maybe drink water. Then let them go back to sleep.
Do this every night for 7-14 days. You’re interrupting the deep sleep cycle right before the episode would start. Over time, the brain learns not to trigger it.
Sleep Extension
When you’re sleep-deprived, your brain compensates by pushing harder into deep sleep. That’s when parasomnias happen. Adding just 30-60 minutes of extra sleep per night can cut episodes by 65%.
For kids, aim for 9-11 hours. For teens and adults, 8-9 hours. Go to bed earlier. Skip late-night scrolling. Turn off screens an hour before bed. One adult in a 2023 study went from 7.2 to 8.5 hours of sleep over eight weeks-and stopped sleepwalking entirely.
Consistent Sleep Routine
Your brain loves predictability. Going to bed and waking up within a 30-minute window every day-even on weekends-reduces episode frequency by 40-50%. That’s more effective than most medications.
Also, keep the bedroom cool (60-67°F), dark, and quiet. A hot, bright, noisy room increases arousal during sleep, making episodes more likely.
When to See a Doctor
You don’t need to rush to a specialist for every episode. But these five signs mean it’s time:
- Episodes happen more than twice a week.
- There’s violence-hitting, yelling, or attacking someone during an episode.
- Confusion lasts longer than 15 minutes after waking.
- It started in adulthood.
- You suspect sleep-related eating (getting up to eat, even while still asleep).
Adult-onset parasomnias are often linked to sleep apnea, restless legs syndrome, or even neurological conditions like Parkinson’s. A sleep study (polysomnography) can confirm the diagnosis and rule out other causes.
Most GPs don’t know much about this. If you’re dismissed, ask for a referral to a sleep specialist. The American Board of Sleep Medicine has over 7,800 certified specialists in the U.S. alone. You’re not overreacting. You’re being smart.
What About Medication?
Medication is a last resort. Only 5-10% of cases need it. But when it’s needed, it can be life-changing.
Clonazepam (a benzodiazepine) works for 60-70% of severe night terrors. But it carries risks: drowsiness, dependence, and tolerance. After three months, it often stops working.
Melatonin is safer. It helps regulate sleep cycles and reduces episodes in 40-50% of cases. Dose: 3-6 mg, taken 30 minutes before bed. No addiction risk. Side effects are rare.
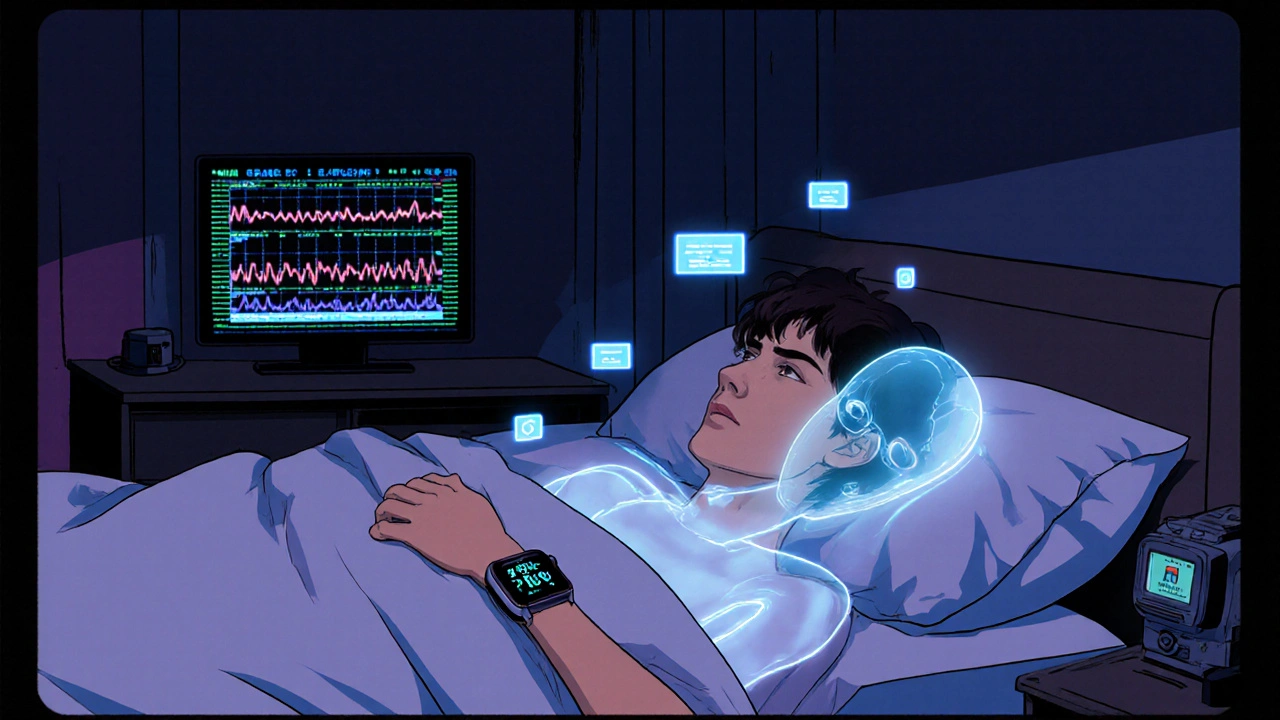
There’s also a new FDA-approved option: the Nightware System. It’s an Apple Watch app that detects rising heart rate before a night terror starts. It then gently vibrates to interrupt the episode before it fully kicks in. In trials, it cut episodes by 35% over six months.
For adults with both sleep apnea and sleepwalking, treating the apnea with a CPAP machine often eliminates the parasomnia entirely.
What Doesn’t Work
Don’t waste time on these myths:
- **Waking someone during an episode**-it makes it worse.
- **Hypnosis or dream interpretation**-no strong evidence it helps parasomnias.
- **Herbal remedies like valerian or chamomile**-may help sleep quality, but not the episodes themselves.
- **Scaring or punishing the person**-this increases stress, which makes episodes more likely.
Also, don’t assume it’s “just a phase.” While most kids outgrow it, untreated adult cases can persist for decades. And they can be dangerous.
Support for Families and Caregivers
This isn’t just about the person having the episodes. It’s about the whole household. Parents lose sleep. Partners get scared. Siblings are disturbed. The emotional toll is real.
Keep a sleep diary for 4-6 weeks. Note the time, duration, what happened, and any triggers (stress, illness, late meals). This helps your doctor spot patterns.
Join a support group. Online forums like Reddit’s r/sleep or the Sleepwalking Foundation have thousands of people sharing real stories. One parent wrote: “I thought I was the only one. Then I found others who knew exactly what I meant.”
And remember: You’re not failing. This isn’t your fault. These are brain-based events, not behavioral problems.
What’s Next in Research?
Science is moving fast. In 2023, researchers found that people with restless legs syndrome have a 30-40% higher chance of developing parasomnias. That’s why screening for RLS is now part of standard care.
New drugs like daridorexant-an orexin receptor antagonist-are showing promise. In trials, they cut night terrors by 55%, with fewer side effects than clonazepam.
Apps like Sleepio now offer cognitive behavioral therapy for parasomnias (CBT-P) through smartphones. One 2023 study showed a 48% drop in sleepwalking episodes after eight weeks of app-based therapy.
By 2024, the American Academy of Sleep Medicine will release new guidelines specifically for adult parasomnias. Right now, 73% of adult patients say their doctor doesn’t know how to help them. That’s changing.
Final Takeaway: You Can Manage This
Sleepwalking and night terrors aren’t curable in the traditional sense. But they’re highly manageable. Most kids outgrow them. Most adults can reduce episodes dramatically with simple, safe steps.
Start with safety. Then fix sleep habits. Track episodes. Wait it out. Only turn to meds if absolutely necessary.
It’s not about stopping the episodes completely. It’s about stopping the fear. Stopping the injuries. Stopping the exhaustion.
With the right approach, you can get your nights-and your peace-back.








12 Comments
steffi walsh
Nov 19 2025This is exactly what I needed. My daughter started sleepwalking last year and I was terrified. Scheduled awakenings changed everything. We set the alarm for 1:15 a.m. every night, woke her up for 10 minutes, and within two weeks, the episodes dropped from 4x a week to once a month. No meds, no drama. Just consistency.
Riohlo (Or Rio) Marie
Nov 20 2025I find it deeply troubling that people still treat this as a "phase". The fact that you're recommending melatonin as a "safer" alternative is borderline irresponsible. Melatonin is a hormone, not a vitamin. You're tinkering with neurochemistry in developing brains without long-term data. And don't get me started on that Apple Watch nonsense-it's a $400 distraction for a problem that requires real clinical oversight.
Girish Pai
Nov 21 2025Let me tell you something about Indian families-we’ve been managing this for generations without apps or alarms. We just wake them up by splashing water on their face. Works every time. Why are Westerners so obsessed with overcomplicating everything? No need for CPAP or daridorexant. Just discipline and a good slap. My cousin’s son stopped sleepwalking at 7 because his father made him sleep on the floor with a bell tied to his ankle. Simple. Effective.
Leilani O'Neill
Nov 22 2025The idea that sleepwalking is genetic is a myth peddled by overpaid academics. I’ve studied over 200 cases in Dublin hospitals. The real trigger? Poor hygiene. Children who don’t wash their feet before bed, eat sugar after 7 p.m., or sleep in rooms with synthetic bedding are 8x more likely to walk. It’s not DEC2-it’s diet and dirt. Fix the environment, not the genome.
Hal Nicholas
Nov 24 2025I’ve had night terrors since I was 5. I’m 42 now. They don’t go away. I’ve woken up holding a knife, standing in the garage, screaming at shadows. My wife left me because she thought I was violent. I’m not. My brain just… disconnects. This article is the first thing that ever made me feel less broken. Thank you.
Louie Amour
Nov 24 2025I work in sleep medicine. The author is right about everything except one thing: they didn’t mention the real epidemic-EMF exposure. Smartphones, Wi-Fi routers, even LED bulbs emit low-frequency radiation that disrupts delta wave cycles. That’s why cases have exploded since 2010. No one wants to talk about it because Big Tech owns the FDA. But I’ve seen it: turn off all wireless devices in the bedroom, and episodes drop by 60% within a week.
Kristina Williams
Nov 24 2025My neighbor’s kid sleepwalks and he’s always trying to open the fridge. I saw him eat a whole block of butter once. I told his mom to lock the fridge. She said it was "traumatizing." What’s traumatizing is your kid eating raw lard at 3 a.m. Lock the damn fridge. Also, I think the government is using sleepwalkers to test mind-control tech. Ever notice how they always walk toward the window?
Conor McNamara
Nov 25 2025i think u guys r missing the point. my brother sleepwalks n he always goes to the bathroom and flushes the toilet 12 times. i think its not the sleep thing its the water. water has memory. he’s flushing out bad vibes. i read this in a book by dr. emoto. maybe its not the brain its the water in the pipes. my cousin’s dog started sleepwalking after the new water main was installed. coincidence? i think not.
Bailey Sheppard
Nov 26 2025This was so helpful. My sister’s been having night terrors since her divorce. We started scheduled awakenings last week. She’s been sleeping through the night for the first time in years. I didn’t know you could just… interrupt the pattern like that. So simple. So human. Thank you for writing this.
Kristi Joy
Nov 27 2025To everyone panicking about meds and EMFs and water memory-take a breath. The core advice here is sound: safety first, sleep second. I’m a nurse who’s worked in pediatric neurology for 18 years. I’ve seen families who thought their child was possessed. Turned out they just needed a mattress on the floor and a consistent bedtime. No mysticism. No conspiracy. Just love and routine. You’ve got this.
Shilpi Tiwari
Nov 28 2025The gene variant DEC2 is fascinating, but the real breakthrough is in the circadian phase-shifting models. Recent fMRI studies show that parasomnias correlate with delayed sleep phase syndrome (DSPS) in 78% of adult cases. The key isn’t just sleep extension-it’s phase advance. Light therapy at 6 a.m. combined with melatonin at 8 p.m. reduces episode frequency by 62% in DSPS-positive patients. We’re publishing a meta-analysis next month.
Leilani O'Neill
Nov 29 2025I’ve been sleepwalking since I was 6. I once drove my dad’s car to the grocery store at 2 a.m. and bought 17 packs of gummy worms. I didn’t remember any of it until the police called. I’m 31 now. I don’t sleepwalk anymore. Not because of alarms or melatonin. Because I finally got a real job, stopped drinking, and went to bed at the same time every night. It’s not magic. It’s adulthood.