When you're taking blood pressure medication, what you eat can be just as important as the pill in your hand. Many people don’t realize that common foods like bananas, spinach, and sweet potatoes can interfere with their meds-sometimes in dangerous ways. If you're on an ACE inhibitor, ARB, or potassium-sparing diuretic, eating too much potassium could raise your blood potassium levels to unsafe levels. But cutting out these foods entirely isn't the answer either. Potassium helps lower blood pressure naturally. The key is balance. And that balance depends on your medication, your kidneys, and your diet.
Why Potassium Matters for Blood Pressure
Potassium isn’t just another mineral. It’s a natural counterbalance to sodium. When you eat more potassium, your body gets better at flushing out excess salt through urine. That reduces pressure on your blood vessels. Studies show that increasing potassium intake can lower systolic blood pressure by over 5 mm Hg in people with high blood pressure. That’s about the same drop you’d see with a low-dose pill.
The American Heart Association recommends 3,500 to 5,000 mg of potassium per day. But most Americans get less than half that-around 2,400 mg. That’s not just a gap. It’s a public health issue. Low potassium intake contributes to about 15% of hypertension cases. And the foods that deliver the most potassium-fruits, vegetables, beans, fish, and dairy-are also the ones that help prevent heart disease overall.
Which Blood Pressure Medications Interact with Potassium?
Not all blood pressure meds affect potassium the same way. The big three that do are:
- ACE inhibitors (like lisinopril, enalapril)
- ARBs (like losartan, valsartan)
- Potassium-sparing diuretics (like spironolactone, eplerenone)
These drugs work by blocking hormones that cause your body to hold onto sodium and water. But they also reduce how much potassium your kidneys excrete. That’s good for blood pressure-but risky if you’re also loading up on potassium-rich foods.
According to the 2022 National Ambulatory Medical Care Survey, about 40% of people taking blood pressure meds are on one of these three types. That means nearly 1 in 2 hypertensive patients could be at risk for high potassium if they don’t adjust their diet.
What Happens When Potassium Gets Too High?
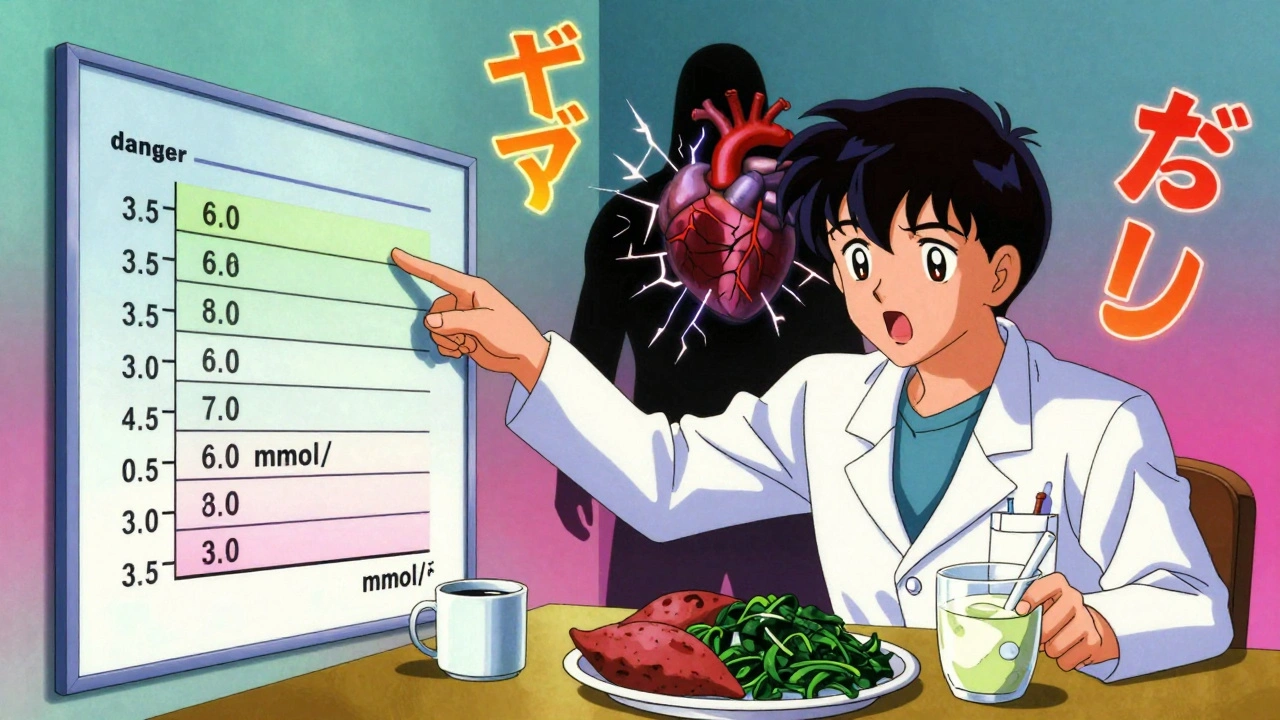
Normal potassium levels are between 3.5 and 5.0 mmol/L. Once you hit 5.0, you’re in the danger zone. Above 6.0, you’re at risk for life-threatening heart rhythms.
Hyperkalemia-high potassium-doesn’t always cause obvious symptoms. But when it does, you might feel:
- Muscle weakness or cramps
- Palpitations or irregular heartbeat
- Numbness or tingling in hands or feet
- Nausea or fatigue
One study of 872 hypertension patients found that 19% experienced symptoms like these after increasing their potassium intake without medical advice. Seven percent ended up in the emergency room. That’s not rare. It’s predictable-and preventable.
People with kidney problems are especially vulnerable. If your eGFR (a measure of kidney function) is below 60 mL/min, your body can’t clear potassium efficiently. One study showed that 28% of these patients develop hyperkalemia even with moderate dietary potassium.
High-Potassium Foods: What to Watch Out For
You don’t need to avoid these foods entirely-but you do need to know how much you’re eating, especially if you're on one of the risky meds.
| Food | Amount | Potassium (mg) |
|---|---|---|
| Sweet potato | 1 medium | 542 |
| Spinach | 1 cup, cooked | 839 |
| Banana | 1 medium | 422 |
| Avocado | 1 whole | 975 |
| Salmon | 3 oz cooked | 534 |
| White beans | 1 cup cooked | 829 |
| Coconut water | 1 cup | 600 |
| Orange juice | 1 cup | 496 |
Some people think one banana a day is harmless. But if you’re on spironolactone and also eat spinach at lunch, an avocado for a snack, and drink coconut water after your workout-you could easily hit 2,500 mg of potassium in a single day. That’s more than half your daily limit. And if your kidneys aren’t clearing it fast enough, that’s a recipe for trouble.
When Potassium Is Safe (and Even Helpful)
Here’s the good news: for most people with normal kidney function, eating potassium-rich foods while on ACE inhibitors or ARBs is safe. A 2016 study followed hypertensive patients for four weeks while they increased their dietary potassium. Their serum potassium levels stayed steady-between 4.1 and 4.3 mmol/L. No spikes. No emergencies.
The difference? These patients got their potassium from food, not supplements. Whole foods contain fiber, water, and other nutrients that slow absorption. Potassium chloride pills or salt substitutes? Those deliver a rapid, concentrated punch. One study found that salt substitutes raised potassium levels by 0.3-0.5 mmol/L on average in people taking ACE inhibitors. That might not sound like much-but in someone with borderline kidney function, it’s enough to push them over the edge.
Dr. Paul Whelton, lead author of the AHA hypertension guidelines, says potassium’s effect is strongest in people eating high-sodium diets. If you’re eating processed food, fast food, or canned soups, your body needs more potassium to balance the salt. In those cases, adding more fruits and veggies isn’t risky-it’s essential.
What You Should Do: A Practical Guide
If you’re on a blood pressure medication that affects potassium, here’s what to do:
- Get your potassium level checked. Ask your doctor for a simple blood test. Don’t assume it’s fine. Many people don’t know their levels until something goes wrong.
- Don’t stop eating potassium-rich foods. Instead, learn portion control. One sweet potato is fine. Two in one day? Maybe not.
- Avoid potassium salt substitutes. They’re marketed as healthy, but they’re the #1 cause of medication-related hyperkalemia. Skip them.
- Track your intake. Use apps like Cronometer or the National Kidney Foundation’s Potassium Counts app. They show you exactly how much potassium is in your meals.
- Time your meds. Some doctors recommend taking ACE inhibitors at least 2 hours before or after a high-potassium meal to reduce absorption spikes.
- Know your symptoms. If you feel weak, your heart skips, or your fingers tingle-call your doctor. Don’t wait.
Patients who followed these steps saw results. One analysis from PatientsLikeMe showed that 63% of hypertensive patients who adjusted their diet under medical supervision lowered their systolic blood pressure by 5 mm Hg or more in just eight weeks.

What Your Doctor Should Be Doing
Doctors are supposed to talk to you about this. But a 2023 survey found that while 72% of patients get general dietary advice, only 38% get specific guidance on potassium-medication interactions.
Ask your doctor:
- “Is my current medication one that raises potassium?”
- “What’s my last potassium level?”
- “Should I get it checked every 3-6 months?”
- “Do I need to avoid any specific foods?”
The European Society of Cardiology recommends potassium testing every 3-6 months for patients on RAAS inhibitors. If your doctor isn’t doing that, ask why.
Special Cases: Kidney Disease and Older Adults
If you have chronic kidney disease (CKD), you’re at higher risk. Even small increases in potassium can be dangerous. A 2021 review found that 11.3% of elderly patients on ACE inhibitors developed hyperkalemia when eating high-potassium diets.
For these patients, potassium supplements are not an option. In fact, studies show a 1.8-fold increase in death risk when potassium levels go above 5.0 mmol/L in stage 3-4 CKD. But that doesn’t mean eating vegetables is off-limits. It means you need a dietitian’s help. A registered dietitian can help you pick lower-potassium alternatives-like apples instead of bananas, cabbage instead of spinach-that still give you nutrients without the risk.
There’s new hope, too. In 2023, the FDA approved patiromer (Veltassa), a medication that binds potassium in the gut and lets it pass out of the body. It’s not a substitute for diet changes-but it allows patients with kidney disease to keep eating heart-healthy foods while staying safe.
Final Thoughts: It’s About Balance, Not Fear
Potassium isn’t your enemy. It’s your ally-unless you’re on certain meds and your kidneys can’t keep up. The goal isn’t to eliminate healthy foods. It’s to understand how your body responds to them.
Most people can safely eat a banana, a serving of salmon, and a side of spinach every day. But if you’re on spironolactone, have diabetes, or your kidneys aren’t working well, you need to be smarter about it.
Don’t wait for a warning sign. Get your potassium checked. Talk to your doctor. Use a food tracker. Make small, smart changes. The result? Lower blood pressure, fewer meds, and a much lower risk of a heart rhythm emergency.
Can I still eat bananas if I take lisinopril?
Yes, but limit yourself to one medium banana per day, and avoid other high-potassium foods like sweet potatoes, spinach, and coconut water on the same day. If your potassium level is above 4.8 mmol/L, your doctor may advise you to switch to lower-potassium fruits like apples, berries, or grapes.
Are potassium supplements safe with blood pressure meds?
No. Potassium supplements are not safe with ACE inhibitors, ARBs, or potassium-sparing diuretics. They can cause dangerous spikes in blood potassium levels. Always get potassium from food, not pills-unless your doctor specifically prescribes a supplement and monitors your levels closely.
How often should I get my potassium level checked?
If you’re on an ACE inhibitor, ARB, or potassium-sparing diuretic, get your potassium checked at least once a year. If you have kidney disease, diabetes, or are over 65, check every 3-6 months. Your doctor should also test you 2-4 weeks after starting or changing your medication.
Do salt substitutes help lower blood pressure?
Yes, salt substitutes that replace sodium with potassium can lower systolic blood pressure by nearly 6 mm Hg. But if you’re on blood pressure meds that affect potassium, they’re dangerous. They can push your potassium level into the danger zone. Avoid them unless your doctor approves them and you’re being monitored.
What are the best low-potassium alternatives to high-potassium foods?
Swap sweet potatoes for white potatoes (peeled), spinach for lettuce or cabbage, bananas for apples or blueberries, and coconut water for regular water or unsweetened tea. Choose white rice over brown rice, and chicken over salmon if you’re watching potassium. Portion control matters-even low-potassium foods can add up.
Can I stop my blood pressure medication if I eat more potassium?
No. Diet can help lower blood pressure, but it doesn’t replace medication for most people. Stopping your meds without medical supervision can cause dangerous spikes in blood pressure. Always work with your doctor to adjust your treatment plan-never on your own.




10 Comments
Elliot Barrett
Dec 11 2025Wow, another article telling me I can't eat my favorite foods. Thanks, I guess.
Maria Elisha
Dec 12 2025So... I'm supposed to stop eating bananas? I'm 28 and healthy. This feels like medical fearmongering.
William Umstattd
Dec 12 2025Let me be clear: if you're on an ACE inhibitor and you're casually consuming avocado toast, coconut water, and sweet potatoes daily, you're not 'eating healthy'-you're playing Russian roulette with your heart. The data is unambiguous. This isn't opinion, it's physiology. If your doctor hasn't checked your potassium in the last six months, you're being negligent. Stop romanticizing 'natural foods' when they're actively putting you at risk.
People think 'whole foods' are inherently safe. They're not. A single cup of cooked spinach has more potassium than three bananas. Combine that with lisinopril and you've got a perfect storm. And no, your 'I eat clean' Instagram bio doesn't override your lab values.
The American Heart Association recommends 3,500–5,000 mg. Most people get 2,400. But that's not the point. The point is: if you're on a RAAS inhibitor, your body doesn't excrete potassium efficiently. You're not 'deficient'-you're in a pharmacological bottleneck. Eating more potassium doesn't fix that. It exacerbates it.
And don't get me started on salt substitutes. They're literally potassium chloride in disguise. Marketers call them 'heart-healthy.' Doctors call them 'cardiac triggers.' The FDA has issued warnings. Yet people buy them like they're organic kale chips.
There's a reason nephrologists hate these articles. They give false reassurance. You don't need to eliminate potassium. You need to measure it. Track it. Know your eGFR. If your kidneys are below 60 mL/min, your diet needs a clinical review-not a TikTok influencer's advice.
One banana a day? Fine. Two? Maybe. Three? You're not a nutritionist-you're a patient. Act like it.
This isn't about fear. It's about accountability. Your body doesn't care how 'clean' your diet is. It only cares about your serum levels. Check them. Or don't. But don't pretend ignorance is a strategy.
Lisa Whitesel
Dec 13 2025People die from hyperkalemia. Not because they ate a banana. Because they ate ten bananas and thought their 'natural lifestyle' made them invincible. Wake up.
Sabrina Thurn
Dec 13 2025As a clinical pharmacist, I see this every week. Patients on spironolactone who start juicing kale, spinach, and beetroot because 'it's good for blood pressure.' Then they show up with a potassium of 6.2 and a flattened T-wave on EKG. The irony? They were trying to avoid meds. Instead, they ended up in the ER needing calcium gluconate and dialysis.
The key isn't restriction-it's awareness. Potassium from whole foods is slower-absorbing, which is why the 2016 study showed stability. But when you combine high-potassium foods with potassium-sparing meds? You're stacking the deck. You need to know your numbers, not your Instagram diet trends.
Also, if you're over 65 or have diabetes, your kidneys don't work like they did in 2010. Your body's ability to clear potassium declines with age. That's not fear-it's biology.
Bottom line: don't avoid potassium. Just don't ignore your meds' interaction with it. Talk to your provider. Get tested. Use Cronometer. You're not being paranoid-you're being smart.
Andrea Beilstein
Dec 14 2025It's fascinating how we've turned nutrition into a moral hierarchy. Eat spinach? Virtuous. Eat salt substitute? Sinful. But the real issue isn't the food-it's the system. Why do we let pharmaceuticals dictate what we can eat? Why is the default response to a drug side effect not to adjust the drug, but to restrict the diet? We've outsourced our physiology to pills and then blamed the food for the consequences.
Maybe we need better drugs. Maybe we need more frequent monitoring. Maybe we need doctors who actually explain this stuff instead of handing out pamphlets. But telling people to stop eating sweet potatoes because they're on lisinopril? That's not medicine. That's avoidance.
Balance isn't about fear. It's about agency. And right now, we're teaching people to fear their food instead of trusting their bodies-with the help of a system that profits from both pills and panic.
Tejas Bubane
Dec 15 2025Let's be real most people on these meds don't even know what an ACE inhibitor is they just take the pill and eat whatever they want then panic when they get dizzy and blame the banana
Also why is everyone obsessed with potassium when sodium is the real villain here
Also coconut water is not a health drink it's just sugar water with electrolytes
And if you're eating 2 sweet potatoes a day you're not eating healthy you're eating like a bodybuilder on a steroid cycle
Stop pretending this is complicated it's not your body is not a chemistry set it's a biological machine that works fine if you don't overdo it
Ajit Kumar Singh
Dec 15 2025India has been eating high potassium diets for centuries and our elders live to 90+ on rice dal and spinach curry
Western medicine is so obsessed with numbers it forgets the body is an ecosystem not a lab experiment
Also why are we assuming all kidneys are the same? My grandfather took losartan for 20 years and never had a problem he ate bananas every day and walked 10km daily
Maybe the problem isn't potassium maybe it's processed food and stress and sitting all day
And why do Americans think every food must be measured like a chemistry equation
Food is culture not a spreadsheet
Larry Lieberman
Dec 17 2025Just got my potassium checked yesterday-4.9. Was about to eat an avocado for lunch. Now I'm eating a pear. 🍐
Also, I use Cronometer. It's wild how fast it adds up. One cup of spinach + banana + salmon = 2,100 mg. That's half my daily limit. I didn't even realize.
Thanks for the heads up. No more coconut water for me. 💧
Angela R. Cartes
Dec 17 2025Okay but like... I'm on lisinopril and I eat a banana every morning with my oatmeal. I'm 42, no kidney issues, active, no symptoms. My last potassium was 4.5. Why am I being told to stop? 😐
Also, I'm not going to stop eating avocado. I'm not a robot.