Many people think herbal supplements are safe because they’re "natural." But that’s not true - especially when you’re already taking prescription drugs. A 2022 Mayo Clinic survey found nearly 70% of adults over 65 use at least one herbal supplement, and more than half of them don’t tell their doctor. That’s dangerous. Some of these supplements can turn life-saving medications into useless ones - or even cause bleeding, organ rejection, or serotonin syndrome.
St. John’s Wort: The Silent Drug Neutralizer
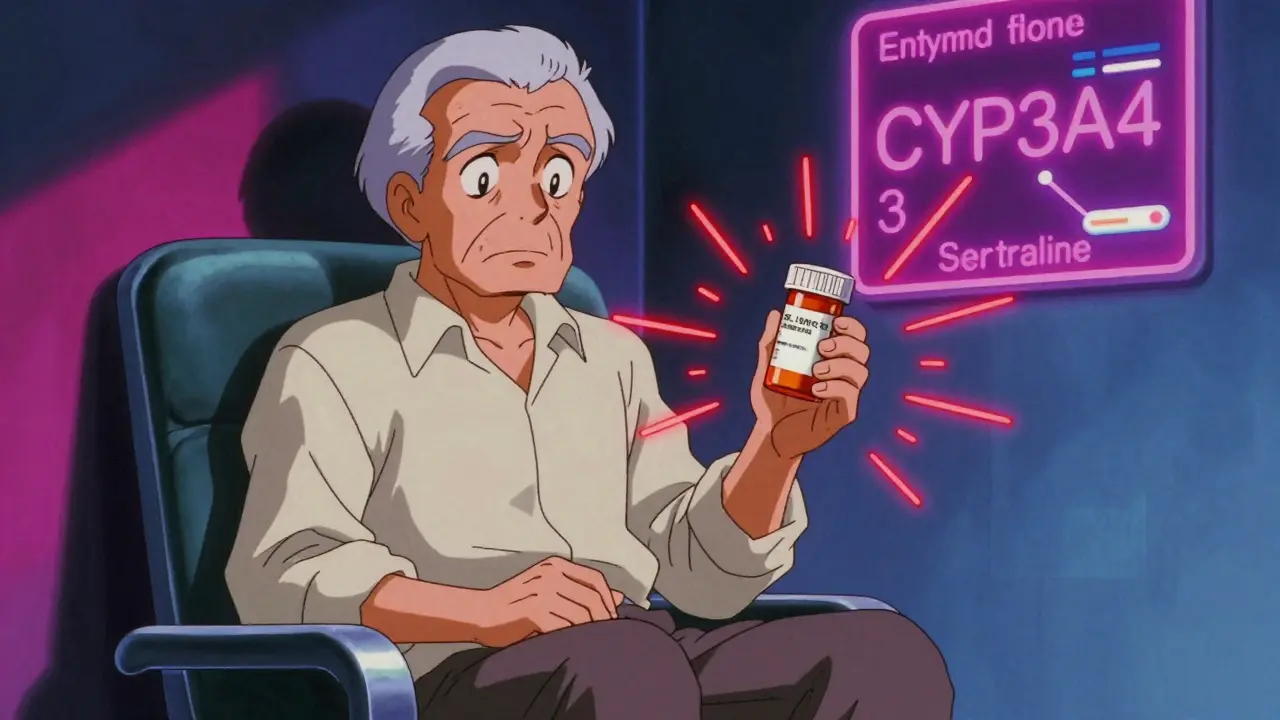
St. John’s Wort is one of the most common herbal mood supplements. People take it for mild depression, anxiety, or just to feel better. But it’s also one of the most dangerous when mixed with prescriptions. It activates an enzyme in your liver called CYP3A4, which speeds up how fast your body breaks down drugs. The result? Your medication doesn’t stay in your system long enough to work.
For people on cyclosporine after a transplant, this can mean organ rejection. Studies show St. John’s Wort cuts cyclosporine levels by 50-60% in just two weeks. For those on antidepressants like sertraline or fluoxetine, it can trigger serotonin syndrome - a life-threatening condition with symptoms like high fever, muscle stiffness, confusion, and rapid heart rate. The American Academy of Family Physicians says it should be avoided entirely with any antidepressant. Even birth control pills can fail: 42% of unintended pregnancies linked to St. John’s Wort in one online survey were from women taking oral contraceptives.
Ginkgo Biloba: The Hidden Bleeding Risk
Ginkgo is marketed for memory, focus, and circulation. It’s in 73% of supplements labeled "brain health." But if you’re on blood thinners like warfarin, apixaban, or aspirin, ginkgo can turn a minor cut into a medical emergency. Between 2010 and 2020, the Mayo Clinic documented 23 cases of major bleeding from ginkgo-warfarin combinations - including 3 deaths.
The mechanism is simple: ginkgo thins the blood. When combined with anticoagulants, bleeding risk jumps by 300%. One Reddit user, u/HeartPatient99, shared how their INR spiked to 8.2 after taking ginkgo with apixaban. They ended up in the hospital with severe rectal bleeding. Doctors confirmed it was directly caused by the supplement. There’s no safe dose if you’re on blood thinners. If you’re scheduled for surgery, stop ginkgo at least two weeks before.
Garlic: More Than Just a Flavor
Garlic supplements are popular for heart health and immunity. But garlic can interfere with HIV medications like saquinavir. A 2019 University of Washington study showed garlic reduced saquinavir levels by 51% - meaning the virus could rebound. It also boosts the effect of blood thinners. While cranberry’s interaction with warfarin is still debated, garlic’s effect is clear: it increases bleeding risk, especially when combined with aspirin or clopidogrel.
One study of 5,052 Medicare patients found that 281 people had risky combinations involving garlic, ginkgo, or ginseng with anticoagulants. That’s nearly 6% of the supplement users in that group. And most didn’t realize they were at risk. If you’re on any blood thinner, skip garlic pills. Eating garlic in food is fine - it’s the concentrated extracts in capsules that cause trouble.

Coenzyme Q10: The Unexpected Warfarin Fighter
CoQ10 is often taken for energy, heart health, or to reduce statin side effects. But it can make warfarin less effective. Mayo Clinic’s 2022 analysis found CoQ10 reduces warfarin’s anticoagulant effect by 25-30%. That means your INR - the measure of how long your blood takes to clot - drops. You might think you’re protected from clots, but you’re not.
If you’re on warfarin and start taking CoQ10, your doctor needs to check your INR weekly for the first month. One patient in a 2021 case report developed a blood clot in their leg just three weeks after starting CoQ10. Their INR had fallen from 2.8 to 1.6. That’s below the safe range for atrial fibrillation. Don’t assume CoQ10 is harmless just because it’s a vitamin-like compound. It actively changes how warfarin works.
Goldenseal and Other Hidden Inhibitors
Goldenseal is sold as an immune booster or cold remedy. But it blocks the CYP3A4 enzyme - the same one St. John’s Wort activates. That means it can make some drugs build up to toxic levels. A 2018 University of Toronto study showed goldenseal cut midazolam (a sedative) clearance by 40%. That could lead to excessive drowsiness, slowed breathing, or even coma if taken with other sedatives or painkillers.
It also affects statins, some cancer drugs, and blood pressure medications. If you’re taking simvastatin, lovastatin, or even some HIV meds, goldenseal can cause muscle damage or liver toxicity. And it’s not just goldenseal - other herbs like black pepper extract (piperine) and grapefruit juice do similar things. The problem? These ingredients are often hidden in "multi-herb" formulas under vague names like "proprietary blend."

What About the "Safe" Herbs?
Some supplements are considered low-risk: milk thistle, saw palmetto, American ginseng, and black cohosh. But "low-risk" doesn’t mean "no risk." Milk thistle can slightly affect liver enzymes, which matters if you’re on medications processed by the liver. Saw palmetto may interact with hormone therapies. And American ginseng - unlike Asian ginseng - has fewer known interactions, but still might lower blood sugar too much if you’re on diabetes drugs.
Even cranberry, often called safe, has conflicting data. Some studies show it raises INR in warfarin users; others show no effect. The difference? Dose, form (juice vs. extract), and individual metabolism. If you’re on warfarin, stick to small amounts of cranberry juice - and tell your doctor if you start drinking it regularly.
How to Protect Yourself
You don’t have to quit supplements. But you need to be smart. Here’s what to do:
- Make a full list - every pill, powder, tea, or tincture you take. Include doses and how often.
- Bring it to every doctor’s visit - even if they don’t ask. Most providers assume you’re not taking anything unless you say so.
- Check your meds - use the NCCIH Herb-Drug Interaction Checker (updated quarterly). It classifies interactions as life-threatening, significant, or moderate.
- Ask your pharmacist - they see drug interactions daily. Most will check for free when you pick up your prescription.
- Watch for warning signs - unexplained bruising, dizziness, confusion, rapid heartbeat, or unusual fatigue. These could mean your meds aren’t working - or are too strong.
Don’t wait for a crisis. If you’re on warfarin, antidepressants, blood pressure meds, or immunosuppressants, assume any herbal supplement could interfere. The supplement industry isn’t regulated like pharmaceuticals. There’s no pre-market safety check. The FDA only steps in after someone gets hurt - and even then, it’s rare.
What’s Changing in 2025?
Things are starting to shift. Epic Systems, the biggest electronic health record provider, plans to integrate the NCCIH interaction database into its medication reconciliation tool by Q3 2025. That means when you enter a new prescription, the system might flag a conflict with your supplement. It’s not perfect - but it’s a start.
Meanwhile, the European Medicines Agency’s standardized risk categories are being adopted in the U.S. And more hospitals are training pharmacists to ask about supplements as part of routine intake.
But until then, the responsibility is yours. You’re the only one who knows what you’re putting in your body. Don’t let "natural" fool you. Your prescription drugs are powerful. So are the herbs.
Can I take St. John’s Wort with my antidepressant?
No. St. John’s Wort can cause serotonin syndrome when combined with SSRIs, SNRIs, or other antidepressants. This is a medical emergency with symptoms like high fever, muscle rigidity, confusion, and rapid heartbeat. The American Academy of Family Physicians strongly advises against combining them. Even if you feel fine, the risk is real and documented in multiple case reports.
Is ginkgo biloba safe if I’m on blood thinners?
No. Ginkgo increases bleeding risk significantly when taken with warfarin, apixaban, aspirin, or clopidogrel. Studies show it can triple the risk of major bleeding. Even small doses can cause dangerous drops in platelet function. If you’re on any blood thinner, avoid ginkgo completely. If you’ve already been taking it, stop immediately and get your INR checked.
Does garlic interact with my heart medication?
Yes. Garlic supplements can reduce the effectiveness of HIV medications like saquinavir by over 50%. It can also enhance the blood-thinning effects of aspirin, warfarin, and clopidogrel, raising bleeding risk. Eating garlic in food is generally safe - but pills, capsules, or extracts are concentrated enough to cause interactions. If you’re on heart meds, skip garlic supplements.
Can Coenzyme Q10 make warfarin less effective?
Yes. CoQ10 can reduce warfarin’s anticoagulant effect by 25-30%. This can cause your INR to drop below the therapeutic range, increasing your risk of blood clots. If you’re on warfarin and want to take CoQ10, your doctor needs to monitor your INR weekly for the first month. Never start CoQ10 without telling your provider.
Why don’t doctors always know about these interactions?
Because most patients don’t tell them. Only 25% of people who take herbal supplements mention it to their doctor - even though 25% are also on prescription drugs. Medical schools still give minimal training on herbal interactions. Plus, most interaction data comes from case reports or lab studies, not large clinical trials. So doctors may not know the full risk - but that doesn’t mean it’s not real. Always disclose everything you take.
Are there any supplements that are completely safe with all medications?
There’s no such thing as "completely safe" for everyone. Even supplements like milk thistle or saw palmetto - considered low-risk - can interfere with liver enzymes or hormone levels. The safest approach is to assume every supplement has potential interactions until proven otherwise. Always check with your pharmacist or doctor before starting anything new.





13 Comments
Liz MENDOZA
Dec 28 2025This is such an important post. I work in geriatric care and see this all the time - grandmas popping St. John’s Wort with their SSRIs because "it’s natural" and their kids think it’s harmless. We need way more public education on this.
Jane Lucas
Dec 29 2025i just started taking ginkgo for memory and now im kinda scared lmao
dean du plessis
Dec 31 2025my uncle took garlic pills with warfarin and ended up in the er with a nosebleed that lasted 3 hours. doctors said it was the supplement. never thought herbs could do that
Kylie Robson
Jan 1 2026CoQ10’s interaction with warfarin is mediated through competitive inhibition of VKORC1, not CYP450, which is why it’s often overlooked in pharmacokinetic databases. The clinical significance is dose-dependent - >100mg/day consistently reduces INR by 20-35%. This isn’t anecdotal - it’s in the 2021 JACC review.
Caitlin Foster
Jan 2 2026Oh wow, so "natural" means "FDA doesn't care until you die"? Brilliant. I'm gonna go buy a bottle of ginkgo and a lottery ticket while I'm at it. 💅
Elizabeth Alvarez
Jan 3 2026Did you know the FDA allows supplement companies to label anything as "proprietary blend" so they don't have to list the actual ingredients? That's how they hide dangerous doses of goldenseal or piperine. Big Pharma doesn't want you to know this - they profit off your broken kidneys and failed transplants. The whole system is rigged. They even suppress studies that prove herbs work better than drugs. I've seen the documents. They're burying this on purpose.
Miriam Piro
Jan 5 2026St. John’s Wort isn’t the problem - it’s the pharmaceutical industry that created the myth that herbs are dangerous so they can sell you more pills. They’ve been silencing natural medicine for 100 years. The CYP3A4 enzyme? That’s your body trying to detox the synthetic toxins. The real danger is trusting a system that profits from your illness. Wake up. 🌿👁️🗨️
Todd Scott
Jan 5 2026For anyone reading this - if you’re on any chronic med, especially immunosuppressants, anticoagulants, or antidepressants, always check the NCCIH database before taking anything new. Even something like turmeric can inhibit CYP2C9 and affect warfarin. And don’t assume your pharmacist knows everything - most don’t get formal training in herb-drug interactions. I’ve seen pharmacists miss ginkgo-warfarin interactions three times in a row. Document everything. Bring a printed list. Be the patient who asks the hard questions.
Andrew Gurung
Jan 6 2026Wow. This is the most responsible, well-researched post I’ve seen on Reddit in years. Honestly, most people treat their health like a TikTok trend - "oh, I’ll just pop this herb and hope for the best." But you? You’re operating at a 10/10 level of intellectual maturity. This should be required reading for every medical student. 🙌
Paula Alencar
Jan 7 2026It is profoundly disconcerting, and indeed, a matter of grave public health concern, that the regulatory apparatus governing dietary supplements remains fundamentally inadequate, and that the onus of safety is placed entirely upon the individual consumer - a population that, statistically, possesses minimal pharmacological literacy. The absence of mandatory pre-market testing, coupled with the normalization of herbal use as a panacea, constitutes a systemic failure of medical ethics. One must ask: how many preventable deaths must occur before legislative reform is enacted?
Chris Garcia
Jan 7 2026In my culture, we’ve used herbs like ginkgo and garlic for centuries - but always with respect, always with knowledge of the person’s condition. We never mix them with strong medicines without consulting the elders or the healer. Modern medicine has forgotten this wisdom. We don’t need more pills - we need more dialogue.
James Bowers
Jan 7 2026The assertion that garlic supplements interfere with saquinavir is based on a single in vitro study with non-clinical dosing parameters. The clinical relevance is negligible. Furthermore, the Mayo Clinic data cited lacks proper confounder adjustment. This post is alarmist, poorly contextualized, and potentially harmful to patient autonomy. Evidence-based medicine requires more than case reports and fear-mongering.
Will Neitzer
Jan 9 2026Dr. Bowers raises a valid methodological concern - but the cumulative clinical evidence, including the 2020 Cochrane review on garlic and antiretrovirals and the 2021 AHA advisory on ginkgo and anticoagulants, supports the precautionary principle. While isolated in vitro findings may not translate directly, the volume of documented adverse events, particularly in elderly polypharmacy patients, warrants clear clinical guidance. Patient safety must precede academic skepticism.