Alzheimer’s disease isn’t just forgetting where you put your keys. It’s losing the ability to recognize your own children, forgetting how to tie your shoes, or no longer remembering the name of the person you’ve lived with for 50 years. It’s the most common cause of dementia, affecting 60-80% of all dementia cases worldwide. By 2025, over 7 million Americans aged 65 and older are living with it-and that number is expected to nearly double by 2060. This isn’t a normal part of aging. It’s a brutal, progressive brain disease with no cure… but new treatments are changing the game.
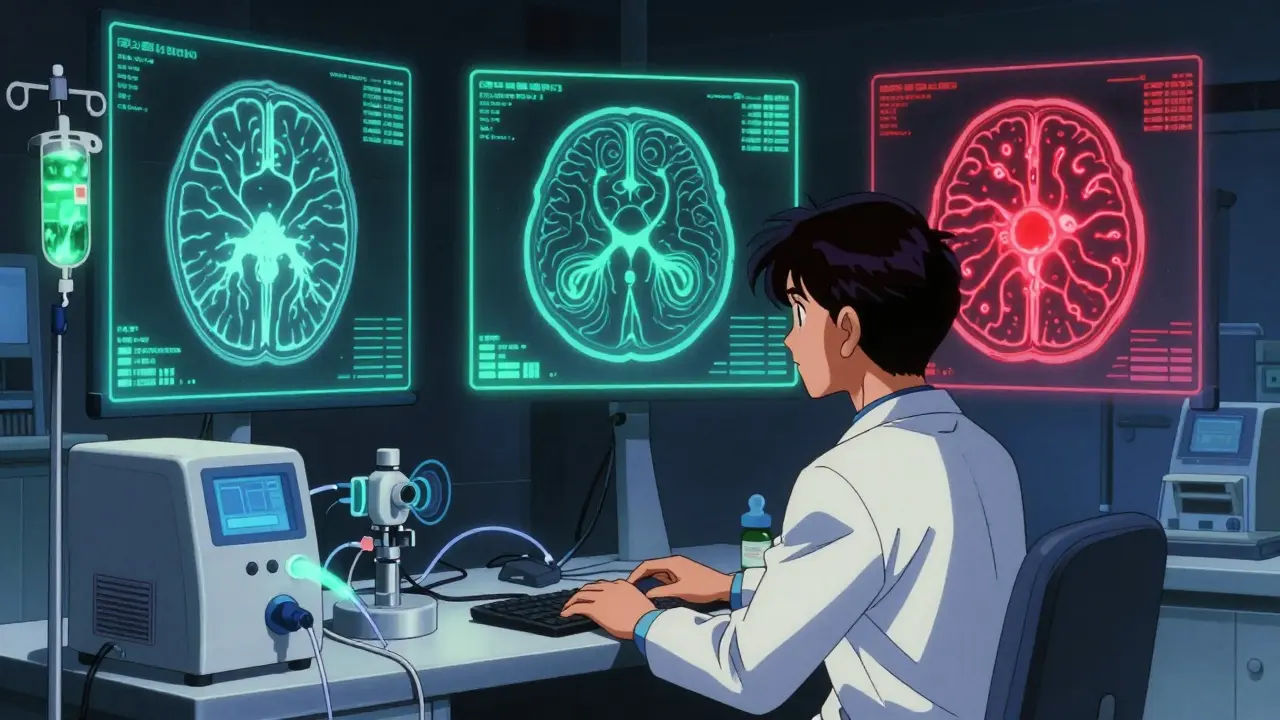
What Happens in the Brain?
Alzheimer’s doesn’t start with memory loss. It starts in silence. Years before symptoms show, two abnormal proteins begin to build up in the brain: beta-amyloid and tau. Beta-amyloid forms sticky clumps called plaques between nerve cells. Tau, normally a support structure inside cells, twists into tangled threads called neurofibrillary tangles. These tangles choke off the cell’s transport system, starving it of nutrients. Over time, brain cells die-especially in the hippocampus, the area responsible for forming new memories. By the time someone is diagnosed, they’ve already lost 20-30% of their brain volume in key regions.These changes aren’t guesswork. Doctors now use biomarkers to see them. A spinal fluid test can detect low levels of amyloid-beta 42 and high levels of phosphorylated tau-with 85-90% accuracy. Amyloid PET scans show those plaques directly, with 92% specificity. Tau PET scans are newer but still reliable at 78% sensitivity. Still, only 35% of U.S. hospitals offer these scans. For most people, diagnosis still relies on memory tests, brain imaging like MRI, and ruling out other causes like thyroid problems or vitamin deficiencies.
The Seven Stages of Progression
Alzheimer’s doesn’t hit all at once. It creeps in, then climbs. Experts break it into seven stages:- Stage 1 (No impairment): No symptoms. Brain changes are happening, but the person functions normally.
- Stage 2 (Very mild decline): Minor memory lapses-forgetting names, misplacing things. Often dismissed as stress or aging.
- Stage 3 (Mild decline): Friends and family notice. Trouble remembering recent conversations, planning events, or finding the right words. This is often when people first seek help.
- Stage 4 (Moderate decline): Clear cognitive issues. Forgetting personal history, struggling with finances, needing help with complex tasks like cooking or driving. Diagnosis usually happens here.
- Stage 5 (Moderately severe decline): Major gaps in memory. May not remember where they live or what year it is. Needs help with dressing, bathing, choosing clothes.
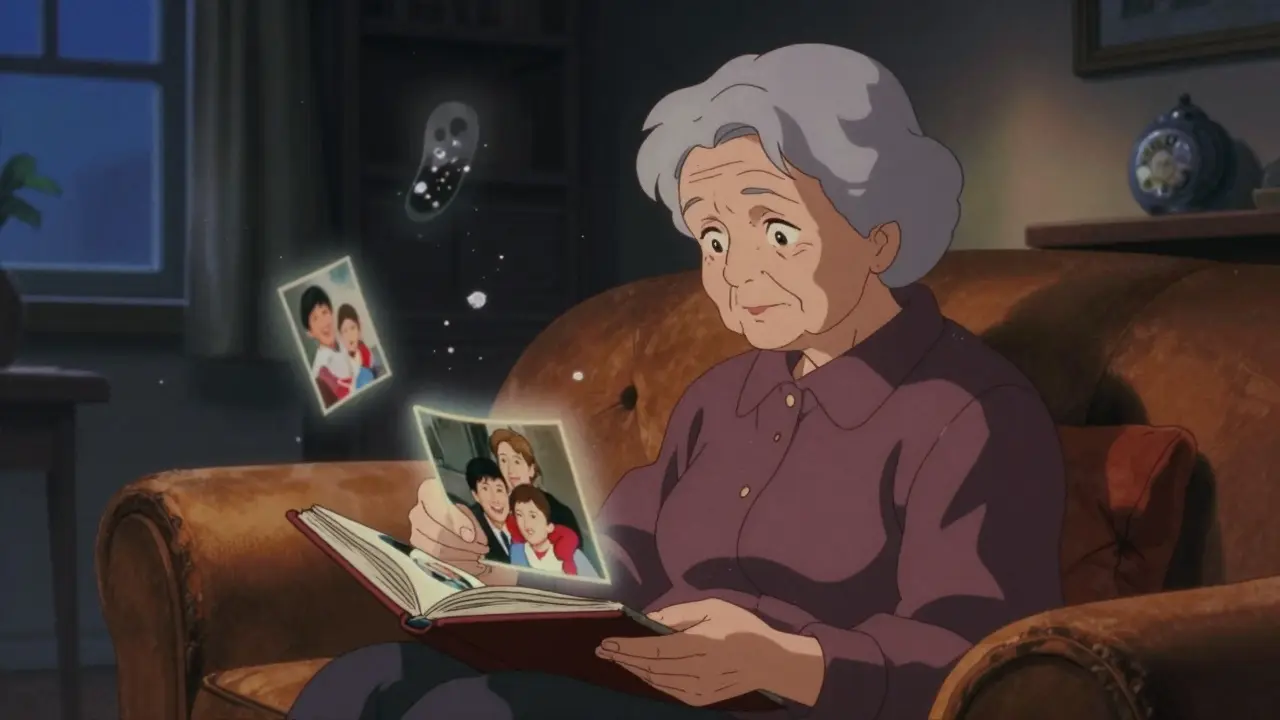
- Stage 6 (Severe decline): Personality changes. May confuse family members, wander, lose bladder/bowel control. Needs full-time help with daily tasks.
- Stage 7 (Very severe decline): Loses ability to speak, walk, or swallow. Completely dependent. Often bedridden. This is the final stage.
On average, people live 4 to 8 years after diagnosis. But some live up to 20. Progression speed varies wildly based on age, overall health, genetics, and access to care.
Current Medications: What Works and What Doesn’t
For decades, treatment options were limited to two types of drugs that only masked symptoms-never slowed the disease.- Cholinesterase inhibitors (donepezil, rivastigmine, galantamine): These boost acetylcholine, a brain chemical involved in memory. They help 40-50% of patients stabilize symptoms for 3-6 months. Side effects? Nausea, vomiting, diarrhea, and sleep problems. Many patients quit because the downsides outweigh the benefits.
- Memantine (Namenda): Works on glutamate, another brain chemical. Used in moderate to severe stages. Slows decline by 20-30%. Often combined with cholinesterase inhibitors.
These drugs don’t stop Alzheimer’s. They just slow the slide-sometimes for a few months. For many families, the emotional toll of watching a loved one decline while taking pills that barely help is exhausting.
The New Era: Disease-Modifying Therapies
In 2025, everything changed. For the first time, drugs exist that can actually slow the disease’s progression by targeting the root cause: amyloid plaques.- Lecanemab (Leqembi): Approved by the FDA in January 2025 after a major trial showed it slowed cognitive decline by 27% over 18 months. Given as a biweekly IV infusion. But it comes with risks: 12.5% of patients develop ARIA-brain swelling or bleeding visible on MRI. That means monthly brain scans are required.
- Donanemab: In trials, it slowed decline by 35%. Even more effective than lecanemab. But its ARIA risk is higher-24%. It’s not yet FDA-approved as of early 2025, but could be soon.
- ALZ-801: An oral pill for people with two copies of the APOE-e4 gene (the strongest genetic risk factor). In a 2025 trial, it cut cognitive decline by 81% in this group. This could be a game-changer for high-risk patients.
These aren’t cures. But they’re the first real hope of changing the disease’s course. The catch? They’re expensive-$26,500 per year. And they require a complex care setup: a neurologist, an MRI center, and a team trained to monitor for side effects. Only 15% of eligible patients currently get them.
Non-Drug Approaches That Actually Help
Medications aren’t the whole story. Lifestyle changes and therapies can make a real difference-even alongside new drugs.The FINGER study (Finland) showed that combining diet, exercise, cognitive training, and managing blood pressure and cholesterol cut cognitive decline by 25% over two years. That’s as powerful as some drugs.
Cognitive Stimulation Therapy (CST)-group activities like memory games, music, and discussions-improved cognition scores by 1.5 points on a standard scale in a 2024 meta-analysis of over 1,800 patients. It’s low-cost, low-risk, and boosts mood.
And here’s the most hopeful part: 40% of dementia cases may be preventable by managing nine modifiable risk factors-high blood pressure, obesity, hearing loss, smoking, depression, physical inactivity, diabetes, excessive alcohol, and low education. Treating hearing loss alone can reduce dementia risk by up to 20%.

Why So Many People Don’t Get Help
Even with better tools, access is broken.- Diagnostic delay: It takes 18 months on average from first symptoms to diagnosis. People brush it off as aging. Doctors don’t always test.
- Cost and insurance: Amyloid PET scans cost up to $5,000. Medicare often denies coverage. Out-of-pocket costs for families average over $1,000.
- Infrastructure gap: Only 78% of treatment centers are in urban areas. Rural patients can’t get infusions or MRIs.
- Provider training: Only 32% of primary care doctors know the latest diagnostic guidelines.
- Family caregiver burden: 85% of caregivers report high stress. 40% show signs of depression. 60% cut work hours, losing an average of $18,200 per year in income.
And clinical trials? Only 8% of participants in amyloid drug trials are non-white-despite dementia affecting Black and Hispanic populations at higher rates. That means the drugs may not work the same for everyone.
What’s Coming Next
The future isn’t just one drug. It’s precision medicine.- Blood tests: A new test called PrecivityAD2 can detect Alzheimer’s biomarkers in a simple blood draw-with 97% accuracy compared to PET scans. It costs under $500. This could make diagnosis as easy as a cholesterol test.
- Combination therapies: Over 27 clinical trials are now testing amyloid drugs + tau drugs + anti-inflammatories. The goal? Hit the disease from multiple angles.
- Prevention trials: Studies are now testing drugs in people with no symptoms but high genetic risk or biomarker evidence. Early intervention could stop Alzheimer’s before it starts.
By 2030, doctors may use a patient’s genetic profile, blood biomarkers, and brain scans to pick the exact treatment that works best for them. That’s the promise.
Where Do We Go From Here?
Alzheimer’s isn’t just a medical problem. It’s a societal one. Families are breaking under the weight of care. The system is failing to deliver new treatments. And prevention is still ignored.If you or someone you love is showing signs-forgetting recent events, repeating questions, getting lost in familiar places-don’t wait. See a doctor. Ask for a cognitive screening. Push for biomarker testing if it’s available. Talk about care plans early. Join a support group. The Alzheimer’s Association’s 24/7 helpline handled 1.2 million calls in 2024. You’re not alone.
We’re not at the finish line. But we’re no longer running in the dark. We have tools. We have data. We have hope. The question now isn’t whether we can treat Alzheimer’s. It’s whether we’ll make sure everyone who needs help can get it.
Can Alzheimer’s be cured?
No, there is no cure yet. But new disease-modifying drugs like lecanemab and donanemab can slow the progression of symptoms significantly-by up to 35% in some cases. These treatments don’t reverse damage, but they can help people maintain independence longer. Research into cures is ongoing, with over 120 clinical trials targeting different aspects of the disease.
Are the new Alzheimer’s drugs worth the cost and risk?
It depends. For people in the early stages with confirmed amyloid buildup, the benefit can be meaningful-gaining months or even years of clearer thinking. But the drugs cost $26,500 a year, require monthly MRIs, and carry a 12-24% risk of brain swelling or bleeding. For many families, the emotional and financial burden outweighs the clinical benefit. Doctors now recommend these drugs only for carefully selected patients after full counseling.
Can lifestyle changes really prevent Alzheimer’s?
Yes. Studies show that managing high blood pressure, staying physically active, eating a heart-healthy diet, treating hearing loss, and staying socially engaged can reduce dementia risk by up to 40%. The FINGER study proved that combining these factors cuts cognitive decline by 25% over two years. Prevention isn’t guaranteed, but it’s the most powerful tool we have right now.
How do you know if it’s Alzheimer’s or just normal aging?
Normal aging means occasionally forgetting a name or where you parked. Alzheimer’s means forgetting the name of your spouse, getting lost in your own neighborhood, or being unable to follow a simple conversation. If memory loss is worsening, interfering with daily life, or accompanied by mood changes, confusion, or poor judgment, it’s not normal. A doctor can run tests to tell the difference.
What should caregivers do first?
Start by getting a formal diagnosis and understanding the stage of the disease. Then connect with the Alzheimer’s Association for resources: support groups, care planning tools, and legal/financial advice. Learn how to communicate with someone who has dementia-use simple sentences, avoid arguing, and focus on emotions, not facts. Finally, take care of yourself. Caregiver burnout is real. You can’t help someone else if you’re collapsing.






9 Comments
sharon soila
Dec 16 2025Alzheimer’s isn’t just a medical condition-it’s a human experience. Every forgetful moment, every confused glance, every time a loved one doesn’t recognize you-it’s a quiet grief that never ends. But we’re not powerless. The new drugs, the lifestyle changes, the early screenings-they’re not magic, but they’re light in the dark. Keep showing up. Keep asking questions. Keep fighting for care. You’re not alone in this.
nina nakamura
Dec 18 2025The new drugs are a scam theyre expensive and risky and the trials were rigged
Hamza Laassili
Dec 18 2025I mean, come on! We're spending billions on pills while our vets are sleeping on the streets! This is what happens when you let corporate greed run medicine! And don't even get me started on how they're only testing on white folks! Where's the justice?!?!?!
Alvin Montanez
Dec 20 2025It’s deeply concerning that we continue to treat Alzheimer’s as a problem of individual biology rather than a systemic failure of public health infrastructure. The fact that 85% of caregivers report high stress levels while only 32% of primary care physicians are trained in the latest diagnostic criteria speaks to a society that prioritizes profit over compassion. We have the science-we have the tools-but we lack the moral will to distribute them equitably. The real epidemic isn’t amyloid plaques-it’s indifference.
Lara Tobin
Dec 21 2025i just lost my mom to this... i still cry when i see her favorite mug in the cupboard. but seeing lecanemab in the news? it gave me a tiny bit of hope. not for her, but for the next person. you’re not alone. 💔
Jamie Clark
Dec 22 2025Let’s be brutally honest: the entire medical establishment has been lying to us for decades. They told us it was just aging. They told us nothing could be done. Now that drugs exist, suddenly it’s a ‘breakthrough’? No. It’s a delayed reckoning. And the fact that only 15% of eligible patients get access? That’s not a failure of medicine-that’s a moral crime. We’ve known the science for 20 years. We chose not to act. Now we’re playing catch-up with billion-dollar price tags.
Keasha Trawick
Dec 22 2025Okay, so picture this: your brain is a city. Amyloid plaques? Toxic skyscrapers blocking the highways. Tau tangles? The power grid’s been hacked and every streetlight’s out. And now, lecanemab is a demolition crew with a permit-slow, expensive, and sometimes they accidentally blow up your neighbor’s house (ARIA). But hey-they’re tearing down the damn buildings! Meanwhile, FINGER’s just out there handing out kale smoothies and yoga mats like it’s a TED Talk. Both matter. One fixes the infrastructure. The other keeps the lights on while the repairmen show up.
Jennifer Taylor
Dec 24 2025Did you know the government is secretly using Alzheimer’s patients to test mind-control tech? I heard it from a nurse who saw the MRI logs-those brain scans aren’t just for amyloid, they’re mapping neural pathways for surveillance. And don’t get me started on the vaccines-they’re linked to the 5G towers! I’ve been researching this for 7 years. My cousin’s neighbor’s cousin was diagnosed after getting the flu shot. Coincidence? I think not. 🤫👁️
Lauren Scrima
Dec 25 2025Wow. A 35% slowdown... for $26,500... and you need a PhD to even qualify. Thanks, capitalism. 🙃