Nonalcoholic fatty liver disease isn't just about being overweight. It’s a silent condition that quietly damages your liver-often without symptoms-until it’s too late. Once called NAFLD, it’s now known as MASLD (metabolic dysfunction-associated steatotic liver disease), a name that better reflects what’s really going on: your body’s metabolism is out of sync, and your liver is paying the price. This isn’t rare. About 1 in 4 people worldwide have it. In the U.S., that’s over 100 million people. And it’s not just adults-kids are getting it too, especially if they’re overweight.
What’s Actually Happening in Your Liver?
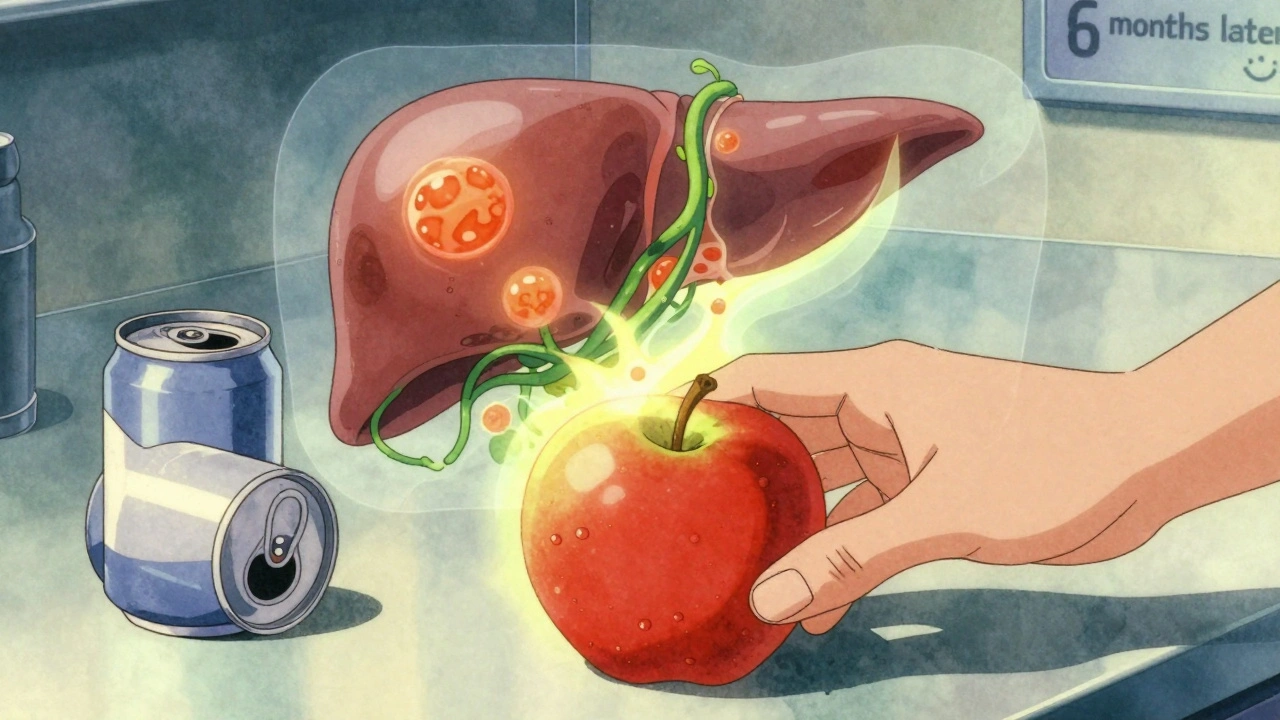
Your liver is supposed to process fats, sugars, and toxins. But when you consistently eat more than your body can handle-especially refined carbs, sugary drinks, and unhealthy fats-your liver starts storing excess fat. That’s steatosis. At first, it’s harmless. But over time, that fat triggers inflammation. That’s when it turns into MASH (metabolic dysfunction-associated steatohepatitis), the more serious form. Inflammation leads to scarring-fibrosis. And if that keeps going, you get cirrhosis, where your liver becomes stiff, lumpy, and can’t function properly. Some people even develop liver cancer.
The scary part? Most people don’t feel anything until the damage is advanced. You might have fatigue, or a dull ache under your right ribs, but 80% of people have no symptoms at all. Blood tests might show elevated liver enzymes (ALT above 30 U/L in women, 40 U/L in men), but even that’s not always enough. Many are told their results are ‘just a little off’-and nothing’s done.
Who’s at Risk?
You don’t have to be obese to get MASLD, but being overweight is the biggest red flag. About 70% of people with type 2 diabetes have it. Nine out of ten people with MASLD have insulin resistance. High blood pressure, high triglycerides, and belly fat are all part of the same problem. In fact, MASLD is the liver’s version of metabolic syndrome.
Some groups are hit harder. Hispanics have the highest rates-nearly 45%-while non-Hispanic Blacks have lower rates, around 20%. But the fastest-growing group is children. One in ten kids in the U.S. now has fatty liver. Among obese kids, that jumps to 70%. That’s not normal aging-it’s a warning sign of a broken food system.
Even people who seem healthy can have it. A 2023 study found that 20% of people with MASLD didn’t fit the classic metabolic syndrome profile. They weren’t overweight, didn’t have diabetes, but still had fat and inflammation in their liver. That’s why just waiting for symptoms is dangerous.
Why It’s Different From Alcohol-Related Liver Damage
People used to think fatty liver only happened with heavy drinking. That’s not true anymore. MASLD has nothing to do with alcohol. It’s caused by insulin resistance, excess sugar, and fat buildup from poor diet and inactivity. The liver doesn’t care if the fat came from beer or from soda. The damage looks similar, but the cause is completely different.
And here’s something surprising: MASLD can lead to cirrhosis just as fast as alcohol-related liver disease. Studies show 15-25% of people with MASH develop cirrhosis within 10 years. That’s faster than most people realize. And unlike alcohol-related damage, where quitting drinking can reverse things, MASLD often slips under the radar because there’s no obvious culprit to stop.

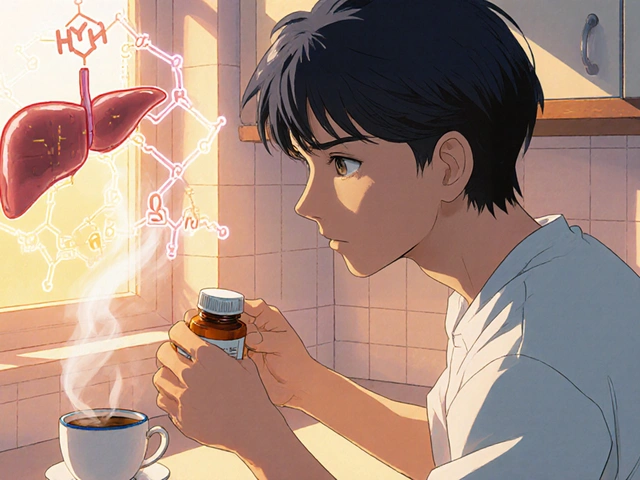
The Hard Truth: No Magic Pill Yet
As of late 2024, there’s still no FDA-approved drug for most people with MASLD. Yes, resmetirom got approved in March 2024 for MASH with fibrosis-but it’s only for advanced cases, and it’s expensive. Most patients won’t qualify. The real treatment? It’s not in a bottle. It’s in your kitchen and on your shoes.
Studies show that if you lose 5-7% of your body weight, you can reverse the fat in your liver in most cases. Lose 10%, and you have a 45% chance of clearing the inflammation too. That’s not a miracle-it’s science. The liver is one of the few organs that can heal itself-if you give it the chance.
But here’s the catch: most people don’t lose that weight. Or they lose it and gain it back. That’s why programs that focus on sustainable habits work better than diets. A 12-week program from the Cleveland Clinic showed 65% of people stuck with the changes after a year. They didn’t count calories-they changed how they ate and moved.
How to Prevent or Reverse It
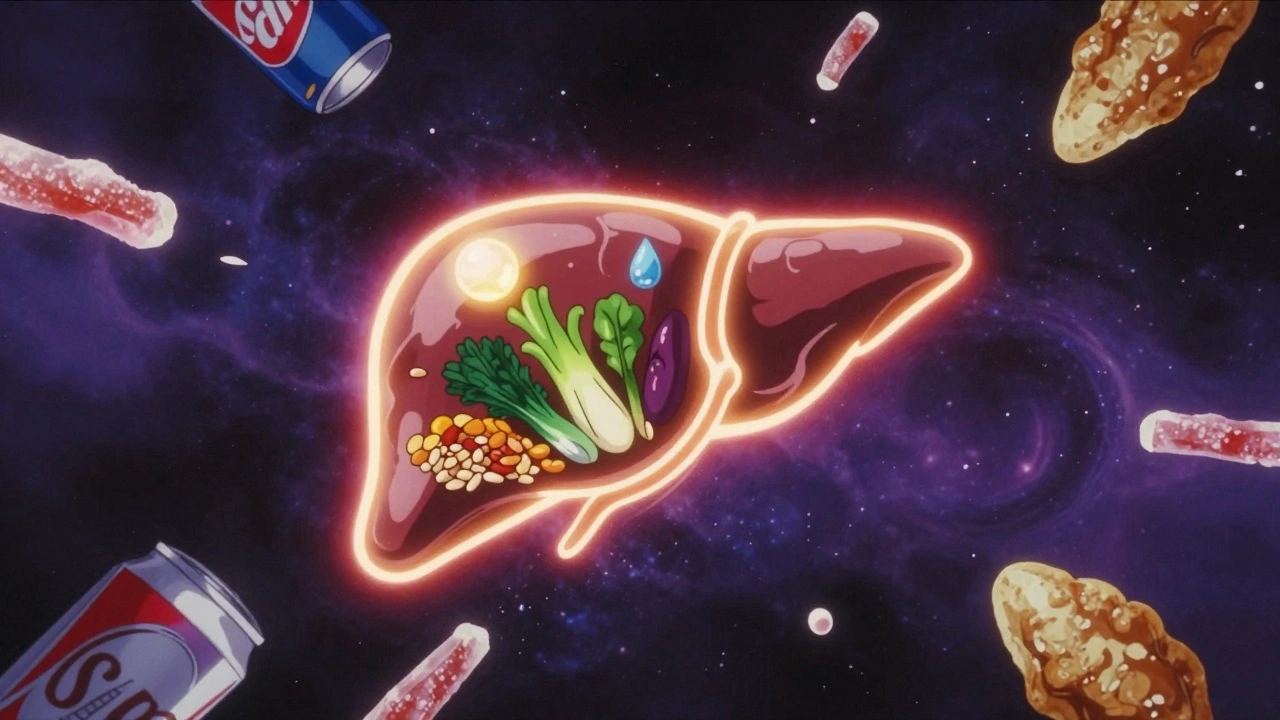
There are four pillars to beating MASLD-and you don’t need a gym membership or a nutritionist to start.
- Drop the sugar. Sugary drinks are the #1 dietary driver. One soda a day can increase liver fat by 27% over 12 weeks. Replace soda with water, unsweetened tea, or sparkling water with lemon. Cut back on fruit juice-even ‘natural’ juice spikes blood sugar like soda.
- Eat real food. Focus on vegetables, beans, lentils, whole grains (oats, quinoa, brown rice), lean proteins (chicken, fish, tofu), and healthy fats (olive oil, nuts, avocado). The Mediterranean diet has been proven to reduce liver fat by 30% in six months. It’s not a fad-it’s how people ate for thousands of years before processed food.
- Move every day. You don’t need to run a marathon. Aim for 150 minutes a week of brisk walking-that’s 30 minutes, five days a week. Or take 10,000 steps a day. Studies show even light activity reduces liver fat. If you’re tired (and many with MASLD are), start with 10 minutes and build up.
- Track your progress. Weigh yourself once a week. Get your liver enzymes checked every 3-6 months. If you can get a FibroScan (a non-invasive liver stiffness test), do it. It’s not perfect, but it’s better than waiting for symptoms.
People who stick with these changes see results. One Reddit user lost 8% of their body weight in a year, did 30 minutes of walking daily, and saw their FibroScan score drop from 9.8 to 5.2 kPa-meaning their liver was no longer scarred. That’s not luck. That’s consistency.
What Doesn’t Work
Detox teas, liver cleanses, and miracle supplements? They don’t help. The liver doesn’t need ‘cleansing’-it cleans itself. Taking vitamin E or milk thistle might sound logical, but there’s no solid proof they reverse MASH. Some supplements can even harm your liver.
Extreme diets like keto or fasting? They can help some people lose weight fast, but they’re hard to keep up. And if you go back to old habits, the fat comes back. The goal isn’t to lose weight fast-it’s to keep it off.
And don’t wait for your doctor to bring it up. Most doctors don’t screen for MASLD unless you’re clearly obese or diabetic. If you have any of the risk factors-belly fat, high blood pressure, prediabetes-ask for a liver enzyme test. It’s a simple blood draw. If your ALT is high, ask about next steps.
The Bigger Picture
MASLD isn’t just a liver problem. It’s a sign your whole metabolism is struggling. People with MASLD have a higher risk of heart disease, stroke, and type 2 diabetes. Treating the liver isn’t enough-you need to treat the whole system.
Workplaces are starting to notice. Companies like IBM have reduced NAFLD rates by 37% in their employees by offering nutrition coaching, step challenges, and healthy meal options. That’s not just good for health-it’s good for business.
But the real problem is systemic. Ultra-processed foods are cheap, everywhere, and engineered to make you eat more. Sugar is hidden in bread, sauces, yogurt, even ‘healthy’ snacks. Until we change the food environment, MASLD will keep rising. That’s why prevention starts with you-but it can’t end there.
What’s Next?
By 2030, half of U.S. adults could be obese. By 2040, MASLD could affect 35% of the global population. That’s over 2 billion people. The cost? Over $100 billion a year in the U.S. alone. And liver transplants for MASLD have quadrupled since 2000.
The good news? It’s preventable. In early stages, 90% of cases can be reversed. But only if you act before the scarring starts. The window isn’t open forever. Once fibrosis sets in, it’s harder to undo.
You don’t need to be perfect. You just need to start. Swap one sugary drink for water. Take a walk after dinner. Add one extra vegetable to your plate. Small steps add up. Your liver doesn’t need a revolution-it needs consistency.
Can you reverse nonalcoholic fatty liver disease?
Yes, especially in the early stages. If you lose 5-7% of your body weight through diet and exercise, you can reverse the fat buildup in your liver. Losing 10% can even clear inflammation and stop scarring. The liver is one of the few organs that can heal itself-if you stop feeding it the things that damage it.
Does MASLD only affect overweight people?
No. While obesity is the biggest risk factor, about 20% of people with MASLD are not overweight. They may have insulin resistance, high blood sugar, or high triglycerides without visible belly fat. This is why doctors now look at metabolic health-not just weight-when screening for liver disease.
Is alcohol allowed if you have MASLD?
Most experts recommend avoiding alcohol completely. Even small amounts can worsen liver inflammation and speed up scarring. While some European guidelines allow minimal intake, the American Association for the Study of Liver Diseases says abstinence is safest. Your liver is already under stress-don’t add another burden.
What foods should I avoid with fatty liver?
Avoid sugary drinks (soda, juice, sweetened coffee), refined carbs (white bread, pastries, pasta), fried foods, and processed snacks (chips, cookies, candy). Watch out for hidden sugars in sauces, yogurt, and ‘low-fat’ products. Focus instead on whole foods: vegetables, legumes, whole grains, lean proteins, nuts, and healthy fats like olive oil.
How long does it take to see improvement?
You can see a drop in liver fat within 6 months of consistent lifestyle changes. Studies using MRI scans show a 30% reduction in liver fat after six months of losing 7% of body weight and exercising 150 minutes a week. But it takes time to build habits-don’t expect overnight results. Focus on progress, not perfection.
Should I get tested for MASLD?
If you have any of these: belly fat, high blood pressure, prediabetes or type 2 diabetes, high triglycerides, or a family history of liver disease, ask your doctor for a liver enzyme test (ALT, AST). If those are elevated, ask about a FibroScan or ultrasound. Early detection is the best way to prevent serious damage.






15 Comments
Chad Handy
Dec 3 2025The liver is an incredible organ, but we treat it like a trash can and then act shocked when it breaks down. I’ve seen friends with normal BMIs but who drink diet soda like water and eat ‘healthy’ granola bars loaded with corn syrup - their ALT levels were through the roof. No one talks about how sugar, not fat, is the real villain here. It’s not about willpower. It’s about a food system designed to exploit our biology. The fact that we still call it ‘fatty liver’ instead of ‘sugar toxicity syndrome’ shows how deeply we misunderstand this.
I work in public health. We run screenings at community centers. Last month, a 14-year-old girl came in - not overweight, but her FibroScan showed stage 2 fibrosis. Her mom said they ate ‘clean’ - organic chicken, gluten-free pasta, almond milk lattes. Turns out, she had three fruit smoothies a day and a bottle of kombucha with 20g of sugar each. The liver doesn’t care if it’s organic or artisanal. It just sees glucose.
We need to stop blaming individuals and start fixing the environment. Schools still sell flavored milk. Hospitals serve sugary cereals for breakfast. Employers give out candy jars at the front desk. This isn’t an individual failure. It’s a societal collapse of nutritional literacy. And until we treat it like the public health crisis it is, we’re just rearranging deck chairs on the Titanic.
Jenny Rogers
Dec 5 2025It is, indeed, a matter of profound moral and physiological significance that the medical establishment has, for decades, failed to adequately communicate the metabolic underpinnings of this condition. The nomenclature shift from NAFLD to MASLD is not merely semantic - it is epistemological. One cannot treat a disease whose etiology is obscured by euphemistic language. The term ‘fatty liver’ implies a passive accumulation, whereas ‘metabolic dysfunction-associated steatotic liver disease’ accurately reflects a systemic derangement of insulin signaling, lipid metabolism, and mitochondrial efficiency.
Moreover, the assertion that weight loss of 5–7% can reverse steatosis is not only empirically supported but also ethically imperative. To suggest that dietary modification is insufficient is to endorse nihilism in preventive medicine. The liver, as the central hub of xenobiotic metabolism, does not operate in isolation. It is a mirror of the organism’s metabolic integrity. To neglect this is to neglect the very architecture of human physiology.
One must also interrogate the commercialization of ‘liver cleanses’ - a grotesque commodification of biological ignorance. Milk thistle, while historically revered, lacks robust Phase III clinical validation. To prescribe it as a panacea is to confuse tradition with evidence. The only true ‘detox’ is the cessation of metabolic insult - a radical act of self-responsibility that our culture has systematically disincentivized.
Rebecca Braatz
Dec 6 2025YOU CAN DO THIS. I know it feels impossible. I was there - 220 lbs, fatigue all day, liver enzymes off the charts. I didn’t go keto. I didn’t buy expensive supplements. I just started walking after dinner. 15 minutes. Then 20. Then I swapped my afternoon soda for sparkling water with lime. One change at a time. Three months in, my doctor said, ‘I can’t believe this is the same person.’
You don’t need to be perfect. You just need to start. One less sugary drink. One extra veggie. One walk. That’s it. Your liver doesn’t need a revolution. It needs you to stop poisoning it. And guess what? Once you start feeling better - more energy, clearer mind - you won’t want to go back. This isn’t a diet. It’s a return to your body’s natural rhythm. You’ve got this. I believe in you.
Jordan Wall
Dec 7 2025It’s fascinating how the metabolic syndrome paradigm has become the dominant heuristic, yet the epistemic foundations remain underdetermined. The reliance on ALT as a biomarker is particularly problematic - it’s neither sensitive nor specific, and its reference ranges are arbitrary, often calibrated for Caucasian male populations, thereby obscuring ethnic variance. Furthermore, the FibroScan’s validity in pediatric cohorts remains contested, with inter-operator variability exceeding 15% in recent meta-analyses.
Also, the conflation of ‘processed foods’ as monolithic villains is reductive. The real issue lies in the glycaemic load of ultra-refined carbohydrates - particularly fructose-induced de novo lipogenesis - which operates independently of caloric intake. Yet, the public discourse reduces this to ‘eat less sugar,’ which is a policy failure disguised as nutrition advice. The solution isn’t individual compliance - it’s structural: sugar taxes, advertising bans, and reformulation mandates. Until then, we’re just doing harm reduction with kale smoothies.
Karl Barrett
Dec 8 2025There’s something deeply poetic about the liver’s ability to regenerate. It’s the only organ that can rebuild itself after near-total destruction - if given the chance. But we don’t give it a chance. We treat it like a machine that can handle endless abuse because it never screams. But it does scream - in silent enzymes, in rising ALT, in invisible fibrosis.
I think we’ve lost touch with the idea that health isn’t a destination. It’s a daily practice of listening. Not to fads, not to influencers, but to the quiet signals your body sends. The fatigue. The bloating. The brain fog after lunch. We call it ‘normal’ because we’ve normalized suffering. But it’s not normal. It’s a warning.
The real tragedy isn’t the disease. It’s that we wait until it’s advanced before we act. We’re trained to fix things when they break, not to prevent them from breaking in the first place. Maybe that’s the deeper illness - our collective refusal to value prevention.
Elizabeth Crutchfield
Dec 8 2025i had this and didnt even know it. my dr just said my alt was high and i was like ‘oh cool’ and went back to eating my pop tarts. then i started feeling wiped all the time and got a fibroscan. turns out i had stage 2. i cried. not because i was fat, but because i realized i’d been ignoring my body for years. now i drink water, walk after dinner, and say no to juice. not perfect, but better. thanks for this post. it made me stop pretending.
Ben Choy
Dec 8 2025I’ve been following this for a year now. Lost 12% of my body weight without counting calories. Just ate more beans, walked 8k steps daily, and stopped drinking anything with sugar. My FibroScan dropped from 11.4 to 6.1. I didn’t even realize how tired I was until I wasn’t tired anymore.
Also - if you think you’re ‘healthy’ because you run marathons but drink smoothies all day? You’re not. Your liver doesn’t care how fit you are. It cares about what you feed it. I used to think I was doing everything right. Turns out, I was just really good at hiding damage.
Emmanuel Peter
Dec 9 2025Let’s be real - 90% of people who read this will scroll past it. They’ll say ‘I’ll change tomorrow’ and keep buying the same crap. This isn’t about knowledge. It’s about denial. People don’t want to hear that their favorite snacks are slowly killing them. They want a pill. A cleanse. A miracle. But there isn’t one. The truth is ugly: you’re the problem. And most of you will never admit it.
Meanwhile, the food industry is laughing all the way to the bank. They know exactly what they’re doing. They engineer products to trigger dopamine spikes. They hide sugar in ‘healthy’ foods. They fund ‘research’ to muddy the waters. This isn’t a medical crisis. It’s a corporate one. And you’re the customer.
Ashley Elliott
Dec 10 2025I appreciate how this post avoids fear-mongering. So many health articles make you feel guilty. This one just says: here’s what’s happening, here’s what helps, here’s how to start. No judgment. Just facts. I’ve shared this with my mom - she’s 68, prediabetic, and didn’t know she was at risk. She’s now swapping soda for tea and taking evening walks. Small steps. But real ones. Thank you.
Augusta Barlow
Dec 10 2025Who really benefits from the MASLD diagnosis? Big Pharma, obviously. They’ve been trying to get a drug approved for years. Now they have resmetirom - expensive, limited use, but profitable. Meanwhile, the real solution - eating real food - doesn’t require patents. It doesn’t need clinical trials. It doesn’t need a CEO on a panel. That’s why they keep calling it a ‘disease’ - to make you think you need a doctor to fix it. But your liver doesn’t need a pill. It needs you to stop eating junk. The whole system is rigged to keep you dependent. Don’t fall for it.
Also - did you know the FDA approved resmetirom after a 12-week trial with 400 patients? That’s not a cure. That’s a marketing campaign. And they’re already pushing it as a ‘breakthrough’ while ignoring the 90% of cases that could’ve been reversed with a walk and some broccoli. This isn’t science. It’s capitalism.
Ollie Newland
Dec 12 2025One thing no one talks about: sleep. I had MASLD, lost weight, cut sugar - but my FibroScan stayed stuck at 8.5. Then I started sleeping 7+ hours. Fixed my circadian rhythm. Cut screen time before bed. Within 4 months, dropped to 5.8. Turns out, poor sleep increases visceral fat and insulin resistance - even if you eat clean. Your liver repairs itself at night. If you’re scrolling TikTok until 2 a.m., you’re sabotaging the healing. Just saying.
Benjamin Sedler
Dec 14 2025So let me get this straight - you’re telling me the entire medical establishment has been wrong for 20 years, and now we’re supposed to believe that walking and eating broccoli is the solution? That’s it? No pills? No surgery? No biotech breakthrough? That’s the most boring thing I’ve ever heard. I thought we were living in the future. Turns out, the cure for liver disease is… being a responsible adult? How anticlimactic.
Also, if MASLD is so common, why aren’t we seeing more liver transplants? Because the stats are inflated. People with elevated ALT have stress, or hepatitis, or are just dehydrated. They’re overdiagnosing this. It’s the new ‘pre-diabetes.’ A money-making label for people who don’t want to accept that modern life is just… hard.
Alex Piddington
Dec 14 2025I’ve worked with over 200 patients with MASLD. The most successful cases weren’t the ones who lost the most weight - they were the ones who built sustainable habits. One woman replaced her daily donut with a boiled egg. Another swapped soda for sparkling water with lemon. They didn’t change their entire lives. They changed one thing. And kept doing it. That’s the secret. Not discipline. Not willpower. Just consistency.
And yes - alcohol should be avoided. Even one drink a week can slow recovery. Your liver is already working overtime. Don’t ask it to detox alcohol too. It’s not asking for a reward. It’s asking for mercy.
Gillian Watson
Dec 15 2025I’m British and I’ve seen this in my family. My dad had it. He didn’t drink. He just ate takeaway every night. Changed to cooking rice and beans with veggies - lost 15kg in 8 months. No fancy diet. Just real food. The liver doesn’t need a revolution. It needs less nonsense.
Shofner Lehto
Dec 16 2025My brother had MASLD. He was 32, not overweight, but ate a ton of ‘healthy’ granola and fruit juice. He thought he was eating clean. Turned out his liver was fried. He started walking, stopped juice, ate more eggs and greens. In 6 months, his enzymes normalized. He’s now a fitness coach. His story changed my life. If he could do it, anyone can. Just start small. Don’t wait for motivation. Just move.