When a generic drug hits the market, it’s not set in stone. Even after FDA approval, manufacturers can make changes - to equipment, ingredients, or production lines. But not every change is allowed without review. Some changes trigger a full re-evaluation by the FDA. If you’re a pharmacist, a patient, or someone working in generic drug manufacturing, understanding what triggers re-evaluation is critical. It affects drug availability, cost, and even safety.
Why Manufacturing Changes Matter for Generic Drugs
Generic drugs aren’t copies in the way you might think. They’re not just repackaged versions of brand-name drugs. They must match the Reference Listed Drug (RLD) in strength, dosage form, route of administration, and, most importantly, bioequivalence. That means your body absorbs the generic drug the same way it absorbs the original. But manufacturing isn’t perfect. Equipment wears out. Suppliers change. Factories move. Sometimes, a company wants to improve efficiency - switch to a new tablet press, use a different solvent, or scale up production. These aren’t just logistical tweaks. They can affect how the drug performs in your body. The FDA doesn’t want you to get a different drug just because the factory changed its machine. That’s why any manufacturing change has to be evaluated. Not all changes are equal. Some are minor. Others? They need full review.The Three Tiers of FDA Review for Manufacturing Changes
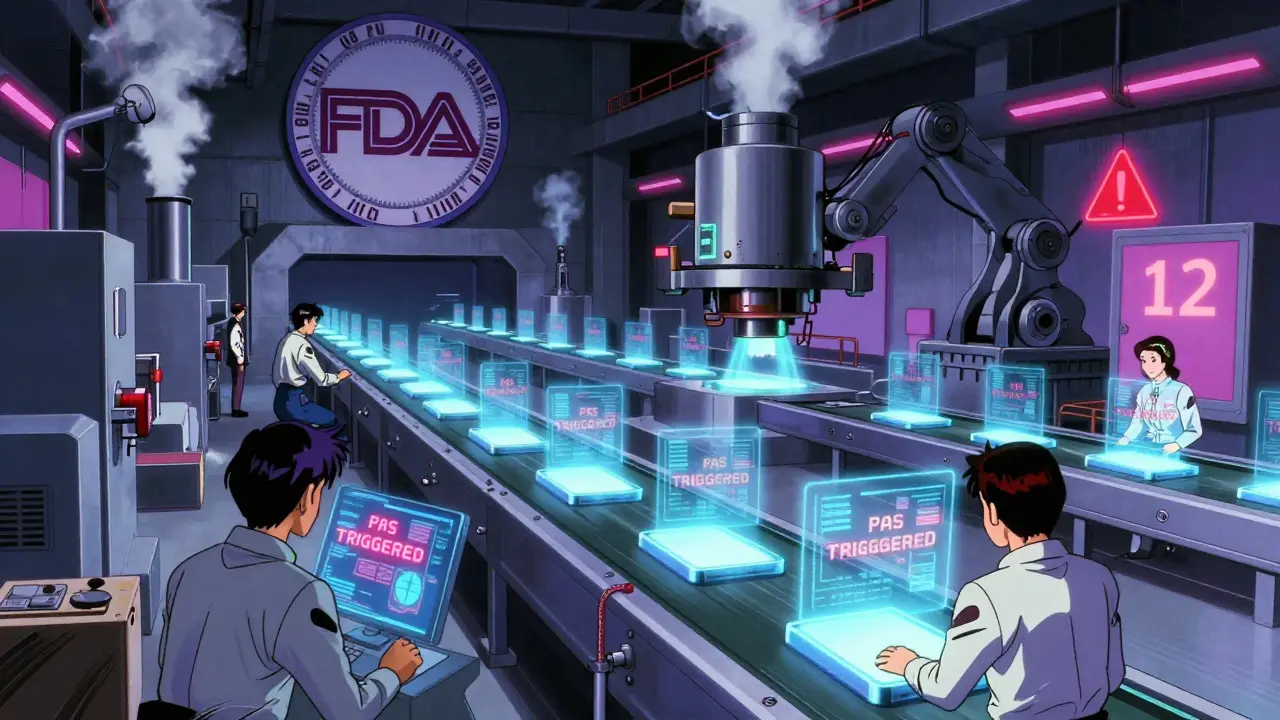
The FDA doesn’t treat every change the same. It uses a risk-based system to sort them into three categories:- Prior Approval Supplements (PAS) - The strictest. You can’t make the change until the FDA says yes. This applies to major changes that could affect safety, effectiveness, or quality.
- Changes Being Effected (CBE) - You can make the change right away, but you must notify the FDA within 30 days (CBE-30) or immediately (CBE-0). These are moderate changes with lower risk.
- Annual Reports (AR) - The lowest risk. You just report the change in your yearly summary. No approval needed.
| Change Type | Typical FDA Category | Why It Matters |
|---|---|---|
| Switching to a new supplier for active ingredient | PAS | Could alter purity or dissolution profile |
| Changing tablet press from 10 to 12 stations | PAS | Alters compression force, may affect dissolution |
| Updating packaging from blister to bottle | CBE-30 | Doesn’t affect drug performance |
| Adjusting in-process testing limits within approved range | AR | Same quality, tighter monitoring |
| Transferring production to a new facility | PAS | High risk - new environment, new personnel, new equipment |
| Adding a new analytical method for purity testing | PAS | Must prove it’s as good as or better than the old one |
For example, if a company wants to switch from batch manufacturing to continuous manufacturing - a newer, more efficient method - that’s a PAS. It’s not just a tweak. It’s a fundamental shift in how the drug is made. The FDA will demand full comparative data: dissolution profiles, stability data, bioequivalence studies. This can take 10 to 14 months to approve.
What Specifically Triggers a Full Re-Evaluation?
Not every change is obvious. Here are the most common triggers for a PAS submission - the kind that forces the FDA to re-evaluate the entire drug:- Change in active pharmaceutical ingredient (API) source - Even if the chemical formula is identical, a new supplier might have different impurities. The FDA requires full testing to prove equivalence.
- Facility transfer - Moving production from one plant to another? That’s a major red flag. Different humidity, equipment, operators - all can affect the product. The FDA will inspect the new site before approving.
- Scale-up or scale-down - Making 10,000 tablets a day? Now you’re making 100,000. That change can alter mixing, drying, and compression. You need validation data showing the larger batch still meets specs.
- Change in formulation - Even swapping one excipient (like a filler) for another can affect how the drug dissolves. If it dissolves slower, your body absorbs less. That’s a safety issue.
- Change in manufacturing process - Switching from wet granulation to direct compression? That’s a process change. The FDA requires analytical and clinical data to prove no difference in performance.
- New impurities or higher impurity levels - If a new impurity appears, even at 0.1%, the FDA demands toxicology studies. For complex generics like peptides, impurities must be below 0.5% with full justification.
Between 2018 and 2022, PAS submissions for manufacturing changes rose by 27.3%. Why? Two big reasons: supply chain disruptions and companies trying to modernize. But the cost is high. A single PAS submission can cost $287,500. For a low-margin generic drug, that’s a tough investment.
How Manufacturers Navigate the System
Most companies don’t just submit paperwork and wait. They use strategies to avoid delays:- Pre-submission meetings - Talking to the FDA before submitting can cut approval time. Teva Pharmaceuticals reduced approval time for amlodipine from 14 months to 8 months by holding three pre-submission meetings.
- Quality by Design (QbD) - This approach builds flexibility into the original ANDA. By understanding how each variable affects the product, manufacturers can make changes later without triggering a PAS. Companies using QbD report 40% fewer major changes.
- Process Analytical Technology (PAT) - Real-time monitoring of production lets companies catch issues early. Firms using PAT had 32.6% fewer PAS submissions over five years.
But not everyone has the resources. Small manufacturers with fewer than five ANDAs report review times 43% longer than big companies. And 65% say they get inconsistent feedback from the FDA - one reviewer says ‘yes,’ another says ‘more data needed.’
How New FDA Programs Are Changing the Game
In September 2023, the FDA launched the ANDA Prioritization Pilot Program. It’s a game-changer. If your generic drug is made entirely in the U.S. - from the active ingredient to the final pill - your review time drops from 30 months to as low as 8 months. This isn’t just about speed. It’s about incentives. The FDA wants more generic drugs made domestically. Why? Because supply chain problems - like the 2020 shortage of antibiotics from India - hurt patients. By 2026, over a third of new generics could qualify for this faster track. Then in February 2024, the FDA announced PreCheck - a two-phase review for high-priority manufacturing sites. Instead of waiting 18 months for a facility transfer, you could get approval in 9 months. These programs are pushing manufacturers to invest in U.S. production. And that’s good news. It means fewer shortages and more predictable supply.
What This Means for Patients
You might not think about manufacturing changes. But here’s the reality: if a generic drug’s manufacturer changes its process and the FDA doesn’t approve it fast enough, the drug can disappear from shelves. That’s happened before - with antibiotics, blood pressure meds, and insulin. On the flip side, when companies upgrade their equipment, they often make better drugs. Cleaner production. Fewer impurities. More consistent dosing. That’s what patients deserve. The FDA’s system isn’t perfect. It’s slow. It’s expensive. It’s confusing. But it’s designed to protect you. Every time a generic drug changes hands - from factory to pharmacy - the system checks: Is this still the same drug?What’s Next?
The next phase of regulation - GDUFA IV, due in 2025 - could bring standardization. Right now, one FDA office might classify a change as CBE-30, while another calls it a PAS. That inconsistency drives up costs and delays. Industry experts hope GDUFA IV will create clear, uniform rules. That would mean less guesswork, fewer delays, and more innovation. For now, the message is clear: manufacturing changes are inevitable. But whether they trigger re-evaluation? That depends on how big the change is - and how well the manufacturer understands its own process.Do all manufacturing changes require FDA approval?
No. Only major changes that could affect safety, effectiveness, or quality require full approval. Minor changes - like switching packaging or adjusting testing limits within approved ranges - can be reported through Annual Reports or Changes Being Effected notices. The FDA uses a risk-based system to classify changes into three categories: Prior Approval Supplements (PAS), Changes Being Effected (CBE), and Annual Reports (AR).
How long does FDA re-evaluation take for a manufacturing change?
It varies by change type. A Prior Approval Supplement (PAS) typically takes 10 months on average, but complex changes - like facility transfers or new manufacturing processes - can take 14 months or longer. CBE-30 supplements are reviewed within 30 days, and CBE-0 within 15 days. Under the FDA’s new ANDA Prioritization Pilot Program, U.S.-manufactured generics can be approved in as little as 8 months.
Why do some generic drug manufacturers avoid making improvements?
Because the cost and time involved in getting FDA approval for a major change can outweigh the benefits. A single PAS submission can cost over $287,500, and approval can take over a year. For low-margin generics, this financial risk discourages innovation. Some companies choose to keep outdated equipment rather than risk delays or rejection.
Can a manufacturing change make a generic drug less effective?
Yes - if it’s not properly evaluated. A change in equipment, ingredient source, or process can alter how the drug dissolves or is absorbed. That’s why the FDA requires comparative studies, stability data, and sometimes bioequivalence testing. Without this, a change could lead to under- or over-dosing, which affects safety.
What is the ANDA Prioritization Pilot Program?
Launched in September 2023, this FDA program speeds up approval for generic drugs that are fully manufactured in the U.S., including the active ingredient. Instead of the standard 30-month review, qualifying applications can be approved in as little as 8 months. The goal is to reduce supply chain risks and encourage domestic investment in generic drug production.
Do small manufacturers face longer approval times than big ones?
Yes. A 2023 survey found that small manufacturers with fewer than five ANDAs experienced review times 43% longer than large manufacturers with over 20 ANDAs. This is partly because big companies have dedicated regulatory teams and more experience navigating FDA expectations. Small firms often struggle with inconsistent feedback and unclear guidance.
What role does Quality by Design (QbD) play in reducing re-evaluations?
QbD helps manufacturers understand how every variable in production affects the final product. By mapping out this ‘design space’ during initial approval, companies can make future changes - like adjusting temperature or pressure - without triggering a full FDA review. Companies using QbD report up to 40% fewer major manufacturing changes after approval.

11 Comments
Brandon Osborne
Feb 9 2026This is why I can't trust generics anymore. My blood pressure med switched manufacturers last year and I started getting dizzy. I called my pharmacy-they said 'it's the same drug.' Same drug? My body says otherwise. The FDA's system is a joke. They let companies change everything and call it 'bioequivalent' while patients suffer. Someone needs to blow the whistle on this.
Lyle Whyatt
Feb 10 2026Look, I work in pharma logistics, and let me tell you-this whole PAS/CBE/AR system is actually way more nuanced than most people realize. It's not just about 'big changes' versus 'small changes.' It's about the *quality of the data* behind the change. A company can submit a PAS for a simple packaging switch if they're paranoid (or under litigation risk). Conversely, some massive facility transfers get approved faster if the company has a flawless audit history. The FDA doesn't just look at the change-they look at the *track record*. And yes, small manufacturers get crushed because they don't have regulatory teams that can spin a 40-page justification like Pfizer can. It's systemic bias disguised as science.
Also, PAT and QbD aren't just buzzwords-they're lifesavers. One plant I worked with reduced PAS submissions by 60% after implementing QbD. They mapped dissolution profiles across 12 process variables. Now they can tweak humidity or pressure without a single letter to the FDA. The system works-if you know how to play it.
And don't get me started on the ANDA pilot. U.S.-made generics? Finally. We've been outsourcing critical APIs to India and China while pretending it's 'cost-effective.' When the supply chain snaps, it's not the FDA's fault-it's ours. We let cheap labor win over national security. Time to fix it.
Tatiana Barbosa
Feb 12 2026Y’all need to stop acting like the FDA is the villain here. This system exists because people died from inconsistent generics. Remember that 2018 valsartan recall? Carcinogenic impurity. 100k+ patients exposed. That’s why PAS exists. Not to ‘delay’ companies-to stop deadlier drugs from hitting shelves. I’m a pharmacist. I’ve had patients come in crying because their med stopped working. Not because it was ‘different’-because the new batch had 12% lower bioavailability. That’s not a glitch. That’s a failure. And the FDA? They caught it before more people got hurt. Yes, it’s slow. Yes, it’s expensive. But it’s the only thing standing between us and a generic drug Wild West.
Also-QbD? Game changer. If your company isn’t using it, you’re not trying. It’s not magic. It’s engineering. And if you think switching tablet presses is ‘no big deal,’ you’ve never seen a batch of pills that crumble like dust because the compression force was off by 5 psi. That’s not theory. That’s real life. And patients notice.
Susan Kwan
Feb 13 2026So let me get this straight-the FDA takes 14 months to approve a change that could save a company $2M/year… but lets Chinese factories pump out pills with 0.8% impurity because ‘it’s within limits’? Right. Sure. And I’m supposed to be grateful for ‘safety’? Please. This isn’t regulation. It’s a bureaucratic extortion racket. The real scandal? The same FDA reviewers who reject a PAS for a U.S. plant will greenlight the exact same change from a facility in Mumbai with zero inspection. Double standard. Classic.
Random Guy
Feb 13 2026bro the fda is just trying to make sure we dont get a drug that turns us into zombies or something lmao
Tom Forwood
Feb 15 2026As someone who’s been on generic insulin for 8 years-I’ve had 3 different versions. One made me hypoglycemic. Another made my blood sugar spike. I didn’t know why until I read this. Turns out, the manufacturer switched excipients and didn’t do full bioequivalence testing. The FDA approved it under CBE-30. I almost died. I now track the manufacturer, lot number, and even the pharmacy’s supplier. It’s insane that patients have to be detectives just to stay alive. The system should be transparent. Not just ‘trust us.’ We deserve to know what’s in our meds.
Also-PAT is legit. My cousin works at a small U.S. generic plant. They installed real-time NIR sensors. Now they catch powder blending issues before the batch even leaves the mixer. No recalls. No delays. Just better medicine. This isn’t sci-fi. It’s here. And it’s cheap. Why aren’t all manufacturers doing this?
John McDonald
Feb 15 2026Big pharma loves to cry about costs, but the real issue is market competition. If a company spends $300k to upgrade equipment and get FDA approval, they raise prices… but then a competitor with outdated gear just copies them and sells cheaper. So why invest? It’s a race to the bottom. The FDA’s system assumes companies care about quality. But in generics, profit margin is 5%. No one’s going to spend $287k to make a better drug when they can make a ‘good enough’ one and win on price. The only way to fix this? Subsidize innovation. Or mandate that every generic change includes a ‘quality premium’ that lets companies recoup costs. Otherwise, we’ll keep getting drugs made on 1990s machinery. And that’s not safety-it’s negligence.
Jacob den Hollander
Feb 16 2026Just wanted to say thank you for this post. I’m a pharmacy tech and I’ve seen firsthand how confusing this all is for patients. They come in, confused because their ‘same’ med now gives them headaches. We have zero access to the FDA’s change logs. We don’t even know if the manufacturer switched suppliers. We just say ‘it’s the same.’ But it’s not. And that’s scary. I’ve started keeping a little notebook-manufacturer, lot, date, patient reaction. It’s not official, but it’s helping. Maybe one day the FDA will make this data public. Until then, patients are flying blind. And we’re just the messengers.
P.S. The ANDA pilot? YES. My uncle’s company just got approved for a U.S.-made metformin batch in 7 months. They’re hiring 12 new workers. That’s what policy should look like.
John Watts
Feb 17 2026Everyone’s talking about PAS and CBE like it’s rocket science. Here’s the simple version: if the change could make your pill dissolve slower, faster, or differently in your stomach-it’s a PAS. If it’s just packaging? CBE. If it’s tweaking a test that doesn’t affect the pill? AR. The FDA isn’t trying to be evil. They’re trying to make sure your blood pressure med doesn’t turn into a sugar pill. The real problem? Companies don’t test changes properly. They cut corners. And the FDA catches them… after people get hurt. So yeah, the system’s slow. But it’s the only thing stopping a lot of people from dying.
Also-QbD isn’t just for big companies. Even small shops can use it. It’s just math and data. You don’t need a PhD. You need a spreadsheet and a willingness to learn. If you’re scared of the FDA, learn how to talk to them. They’re not monsters. They’re just overworked. And they want you to succeed.
Randy Harkins
Feb 17 2026Thank you for this! 🙌 I’ve been on a generic anticoagulant for 3 years. Two different batches. One gave me nosebleeds. The other made me feel like I was underwater. I thought it was me… until I read this. Now I know: it’s the manufacturing. The FDA should require a ‘change notice’ on the pill bottle. Like ‘Manufacturing Process Updated: May 2024’. Patients deserve transparency. Not just ‘trust us.’ We’re not dumb. We just want to know what’s in our bodies. 🌟
Tori Thenazi
Feb 18 2026Okay, but what if… the FDA is being manipulated? What if the ‘PAS’ system is just a way for big pharma to block small competitors? I read somewhere that the FDA gets funding from the same companies they regulate. And what about the 2022 whistleblower report? They found FDA reviewers who approved PAS submissions after being offered ‘consulting gigs’ at the manufacturer. Coincidence? I think not. And don’t tell me ‘it’s for safety’-because if it was, why are there still 300+ drug shortages every year? Something’s rotten here. And it’s not just the manufacturers.