Generic Drugs: What They Are, Why They Matter, and What You Need to Know
When you pick up a prescription, you might see a generic drug, a medication that contains the same active ingredient as a brand-name drug but is sold under its chemical name. Also known as non-brand medications, they’re often cheaper because they don’t carry the cost of marketing or original research. But here’s the thing: just because they’re the same active ingredient doesn’t mean they’re the same for everyone.
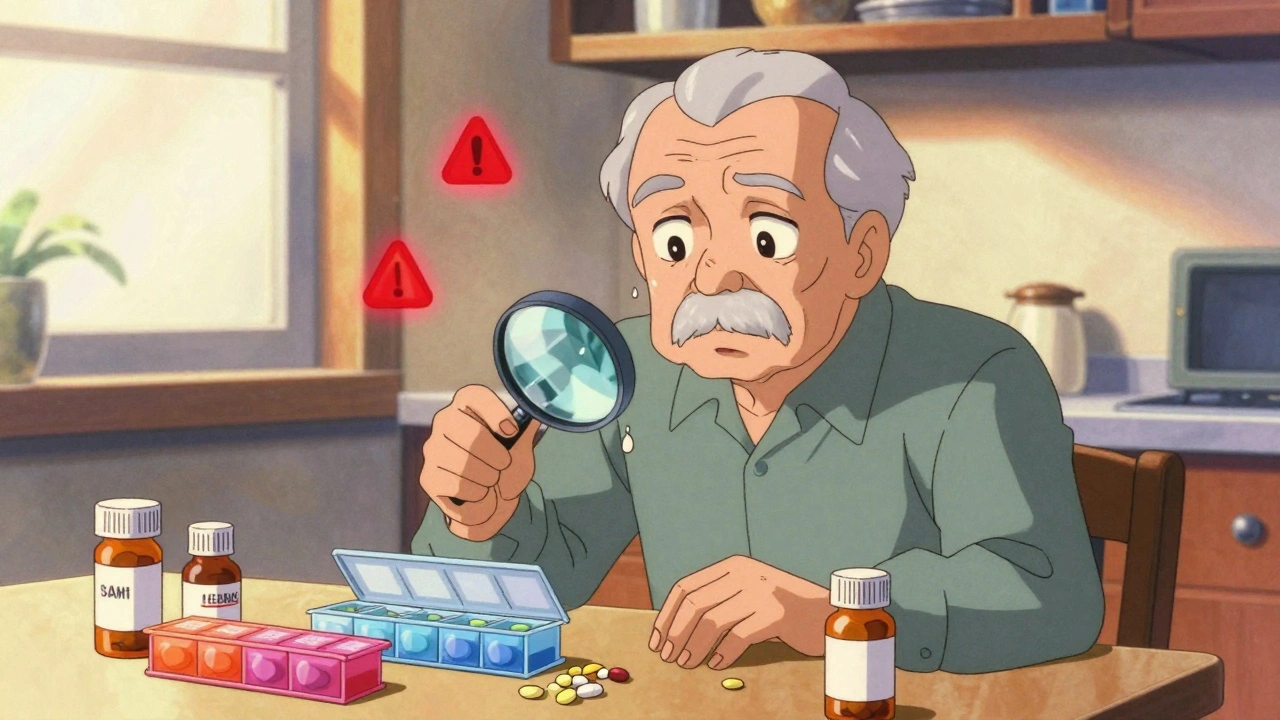
Behind the scenes, excipients, inactive ingredients like fillers, dyes, and binders that help form the pill can make a real difference. One person might take a generic version of a blood pressure pill and feel fine. Another might get headaches, nausea, or strange reactions—not because the drug doesn’t work, but because the filler is different. These aren’t rare cases. Pharmacists see it all the time, and many patients never connect their symptoms to the switch from brand to generic. That’s why understanding what’s in the pill, not just what it does, matters.
Then there’s regulatory exclusivity, the legal delays that let drugmakers block generics even after patents expire. The FDA grants extra years of market control for orphan drugs, new chemical entities, and biologics. That means a life-saving medication might stay expensive for years longer than you’d expect. Meanwhile, insurers use bulk buying and tendering to drive down prices—but those savings don’t always reach you at the pharmacy counter. You might pay more than the cash price just because your insurance plan’s formulary favors one generic over another.
And it doesn’t stop there. drug interactions, when a generic medicine reacts badly with another drug, supplement, or food can be just as dangerous as with brand names. Ginkgo biloba with blood thinners? Lithium mixed with common painkillers? These aren’t hypothetical risks. Real people end up in the ER because no one checked what else they were taking. Even something as simple as switching from one generic manufacturer to another can change how your body absorbs the medicine—especially if you’re on tight-dose meds like thyroid pills or seizure drugs.
There’s a myth that generics are just "copycats." But they’re not. They’re regulated, tested, and approved. But approval doesn’t mean perfection. It means they meet minimum standards. And those standards leave room for variation—especially in the parts no one talks about. If you’ve ever felt off after a refill, even though your doctor said everything was fine, you’re not imagining it. You’re experiencing the hidden side of generic drugs.
Below, you’ll find real stories and facts from pharmacists, patients, and researchers about what actually happens when you take a generic. From why school nurses need to track every pill to how naloxone co-prescribing ties into opioid safety, these posts cut through the noise. No fluff. No marketing. Just what you need to know to stay safe, save money, and ask the right questions.