Drug Toxicity: What It Is, Why It Happens, and How to Stay Safe
When your body can’t handle a medication the way it was meant to, you’re facing drug toxicity, the harmful buildup of a drug in the body that leads to dangerous side effects or organ damage. Also known as medication poisoning, it doesn’t always mean you took too much—it can happen with normal doses if your kidneys or liver can’t process it, or if other drugs interfere. This isn’t rare. One in five hospital visits for older adults is tied to drug toxicity, and many cases start with something as simple as adding a new painkiller or diuretic.
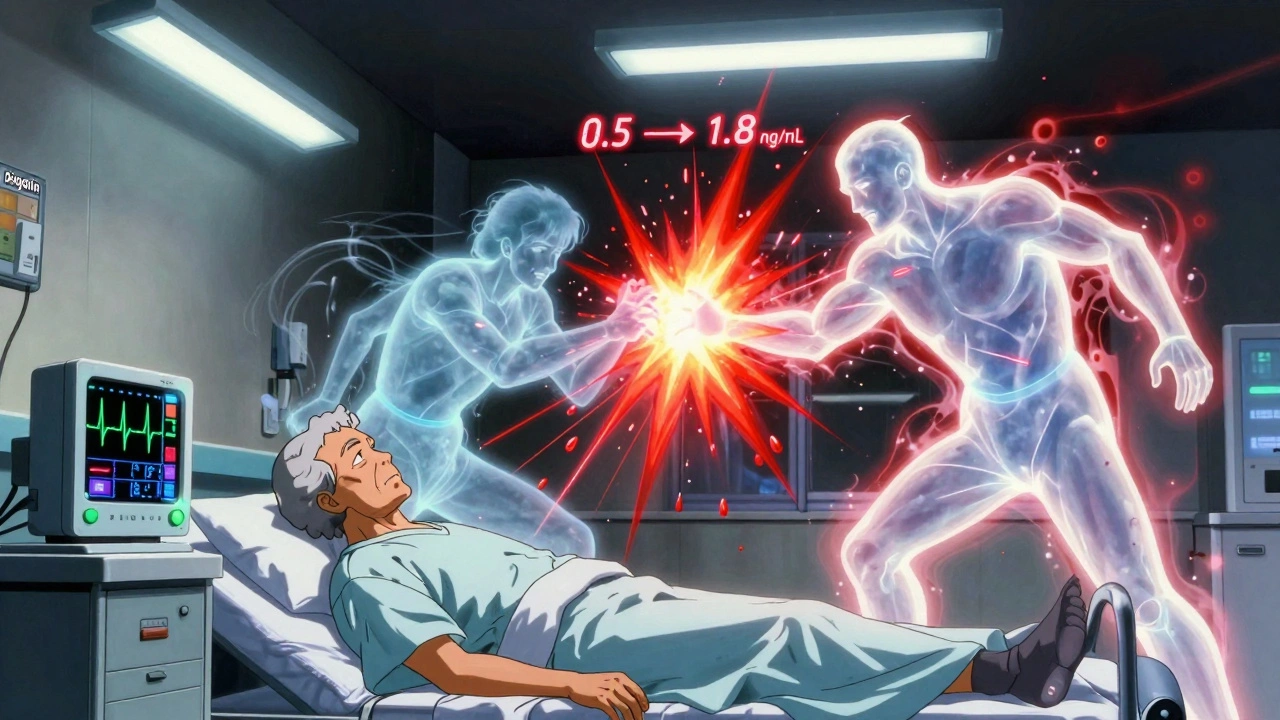
Drug interactions, when two or more medications react in ways that change how each one works are the biggest cause. Think of lithium, used for bipolar disorder. It’s safe on its own—but mix it with common NSAIDs like ibuprofen or a diuretic, and your blood levels can spike overnight. That’s lithium toxicity, a life-threatening condition that causes confusion, tremors, and kidney failure. Or take blood thinners like warfarin: add ginkgo biloba, and your risk of bleeding skyrockets. These aren’t edge cases—they’re everyday risks hidden in medicine cabinets.
Adverse drug events, harmful reactions that happen even when drugs are used correctly don’t always show up right away. Some build up slowly—like swelling from amlodipine or liver damage from long-term statins. Others strike fast, like neuroleptic malignant syndrome from antipsychotics, or serotonin syndrome from mixing antidepressants with cold meds. The common thread? They’re often missed because they look like something else: fatigue, dizziness, or even aging.
What makes this worse is that most people don’t realize their pharmacist or doctor needs to know every single thing they’re taking—not just prescriptions, but supplements, herbal teas, or even over-the-counter pain relievers. A single extra pill can tip the balance. That’s why reports from pharmacists about generic drug problems or excipient intolerances matter. They’re not just paperwork—they’re early warnings.
You don’t need to memorize every drug interaction. But you do need to know your own risks. Are you over 65? Do you have kidney or liver issues? Are you on more than five medications? If yes, you’re in the high-risk group. The good news? Most drug toxicity cases are preventable. It starts with asking: "Could this be interacting with something else?" and "What happens if I stop this?" Then, get your meds reviewed—regularly.
Below, you’ll find real stories and clear guides on how drug toxicity shows up in everyday life—from older adults on multiple pills to kids on school medications, from heart drugs to mental health treatments. These aren’t theory pieces. They’re what happens when safety slips through the cracks—and how to stop it before it’s too late.