Cardiac Drug Interactions: What You Need to Know to Stay Safe
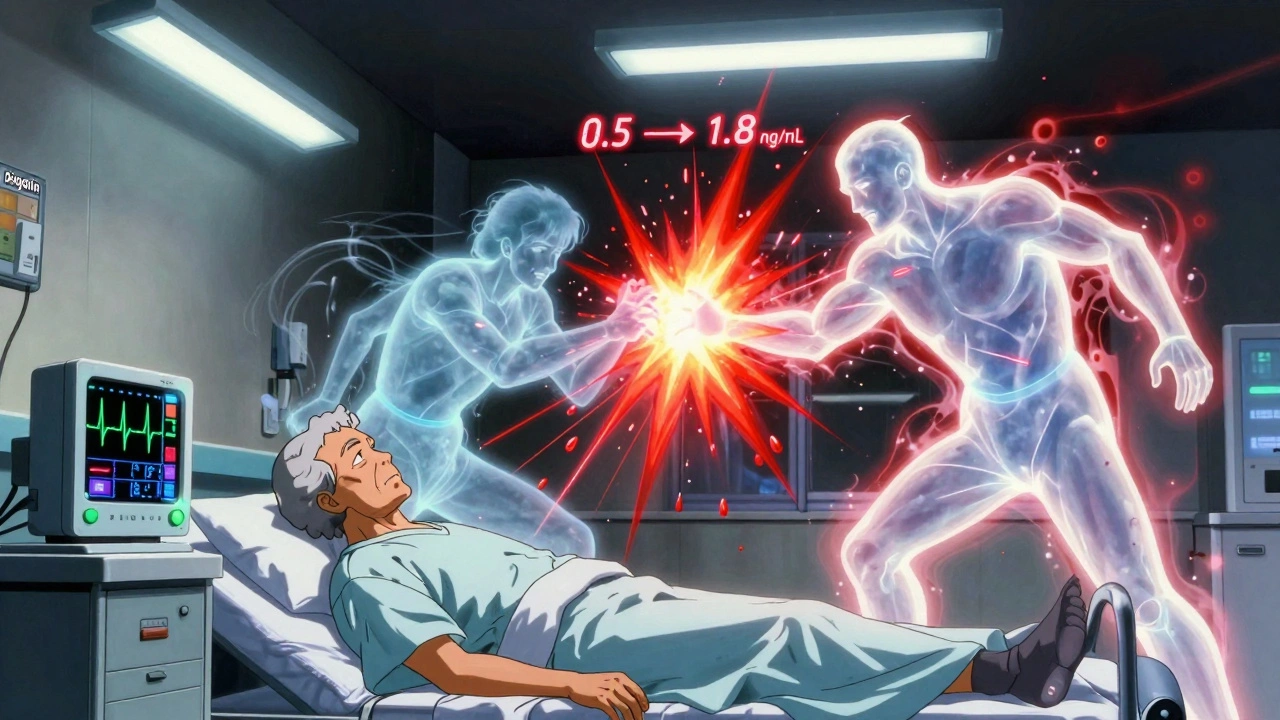
When you take cardiac drug interactions, harmful clashes between heart medications and other drugs or supplements. Also known as heart medication interactions, they happen when one drug changes how another works in your body—often without warning. These aren’t just theoretical risks. They’re real, common, and can send you to the ER. A blood thinner like warfarin mixed with ginkgo biloba? That’s a bleeding risk. A statin like pitavastatin combined with certain antibiotics? That’s muscle damage waiting to happen. And if you’re on a beta-blocker and suddenly start taking an OTC cold medicine with decongestants? Your blood pressure could spike dangerously high.
Heart medication, drugs used to treat conditions like high blood pressure, irregular heartbeat, or heart failure. Also known as cardiovascular drugs, it includes everything from lisinopril to amiodarone. These aren’t simple pills. They’re finely tuned tools. Even small changes in how they’re absorbed or broken down can throw off your whole system. That’s why drug interactions, when two or more substances affect each other’s effects in the body. Also known as medication clashes, they’re not just about pills—you need to watch what you eat, what supplements you take, and even what you drink. Grapefruit juice can wreck your cholesterol meds. Calcium supplements can block your thyroid drug. And don’t assume natural means safe—ginkgo, St. John’s wort, and garlic supplements all have known risks with cardiac drugs.
You’re not alone in this. Older adults, people on multiple prescriptions, and those with chronic conditions like diabetes or kidney disease are at highest risk. That’s why medication safety, the practice of using drugs correctly to avoid harm. Also known as drug safety, it’s not just about taking your pills on time—it’s about knowing what else is in your system. Pharmacists spot these risks daily. They’re the ones who catch when a patient’s new blood pressure drug clashes with their old anti-inflammatory. They’re the ones who warn about mixing lithium with diuretics. And they’re the ones who remind you that even a single new OTC painkiller can undo months of heart health progress.
The good news? You don’t need to guess. You don’t need to memorize a list of 50 dangerous combos. You just need to know what to ask. Bring your full list of meds—prescriptions, supplements, even herbal teas—to every appointment. Ask your doctor or pharmacist: "Could this interact with my heart meds?" If you’re on more than three drugs, get a medication review. Simple steps like these prevent hospitalizations. They save lives. Below, you’ll find real, practical guides from pharmacists and clinicians who’ve seen these interactions play out in real life—from how to avoid dangerous combos with blood thinners, to why some statins are safer than others, to what to do when your doctor adds a new pill to your routine. This isn’t theory. It’s what works.