Ever notice how a simple pill can carry so much hope and so many questions? Plavix, or clopidogrel as you might spot on the label, is one of those medications that's become almost a household name for folks dealing with heart risks. There's a lot of chatter—good, bad, and confusing—about what Plavix really does, how safe it is, and whether all that fuss is justified. But beneath the medical jargon and rushed doctor visits, there's actually a lot to know. Whether you've just had a stent put in, recently survived a heart scare, or you're here because a loved one got prescribed Plavix, you probably want more straightforward answers. So let's strip away the fluff and get real about what this small tablet means for real people like us.
What Is Plavix, and Why Is It So Widely Prescribed?
Ask around, and you'll hear Plavix described as a 'blood thinner.' That's close—but not the whole story. Plavix is the brand name for clopidogrel, a drug designed to help keep your blood from getting too sticky and forming unhealthy clots in your arteries. It isn't thinning your blood like pouring in water; instead, it stops platelets from sticking together so easily. That matters a lot if you've ever faced a heart attack, stroke, or certain types of heart procedures like getting a stent.
Back in 1997, when the FDA first approved Plavix, it pretty much changed the game for people with high clotting risk. According to the Centers for Disease Control and Prevention, over 800,000 people in the US have a heart attack every year, and a huge part of their recovery involves medications to keep the arteries open. Plavix quickly found its place as a go-to for preventing a second heart attack or stroke. It's also given to patients after certain surgeries or angioplasty, usually alongside aspirin, to keep new clots from ruining a freshly unblocked artery.
So, why does it stand out? For a start, Plavix is taken just once a day, usually as a 75mg tablet. Simplicity always wins points when it comes to remembering your meds. It's not just heart folks, either. Anyone with a recent stroke, or people with certain heart rhythm problems and risk of forming clots, might get a script.
Researchers spent years observing folks on Plavix—millions worldwide now—and the numbers show it actually cuts the risk of another scary event by nearly 25% compared to those not taking it. For anyone who’s already had a heart incident, that drop in risk is nothing to shrug off. Still, doctors will only hand out Plavix if they’re convinced the benefit outweighs the bleeding risk. It’s not a multivitamin—this one means business.
One surprising fact: Plavix is a common sight in emergency rooms, tucked next to aspirin and nitroglycerin. Hospitals have protocols to give it fast after certain heart attacks because the sooner it works, the better your odds. It’s now on the World Health Organization’s List of Essential Medicines.
How Plavix Actually Works in Your Body
The science here is pretty wild. Your platelets—tiny cell fragments in your blood—are like the first responders to any wound. Their job is to stick together and plug holes so you don’t keep bleeding. The problem is, in heart disease or after surgery, those platelets can go haywire and form clots where they shouldn’t, blocking up arteries and causing real trouble.
So, what does Plavix do? When you swallow that tablet, it's absorbed and converted by your liver into a form that blocks a specific protein on the surface of platelets called the P2Y12 receptor. Once that’s blocked, your platelets can’t stick together so easily. Think of it as putting traffic cones in front of cars—no one’s forming a pileup.
The effect of Plavix is pretty targeted. It doesn’t mess with other parts of your blood, which means you’re less likely to have unexpected side effects not related to bleeding. Still, you might be surprised to hear that about one in three people has a gene that can make Plavix less effective for them. There’s a real trend now where doctors sometimes order genetic tests—called CYP2C19 tests—before choosing Plavix, especially if you’re at higher risk or have a history of stent issues. It’s not mainstream for everyone yet, but the science keeps unraveling new stuff each year.
What about foods and other meds? Plavix is notorious for interacting with a few things. For example, certain acid reflux drugs (like omeprazole) can block the enzyme that helps activate Plavix, making it less useful. If you’re on those, always ask if you can switch to another acid blocker or adjust how you take them.
Timing is also key. Missing doses is a real danger—one skipped day and your platelets can bounce back to normal function in 5-7 days. If you’ve recently had a stent, even a short break boosts your risk of a clot and emergency trip to the ER. So most doctors say if you miss one dose, take it as soon as you remember unless it’s almost time for the next. Double dosing is not the answer unless your doctor says otherwise.
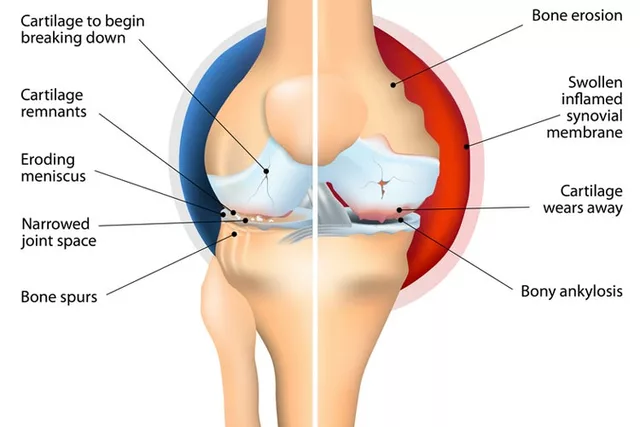
Plavix Uses: Who Needs It and For How Long?
Here’s where the Plavix stories really branch off. Not everyone takes it for the same reason, and the length of treatment can change a lot based on why it was prescribed in the first place. The big three: stopping heart attacks after they start, preventing future strokes, and keeping stents open (plavix is a vital keyword here because it's so core to these scenarios).
- Recent Heart Attack: If you’ve just had a heart attack, it’s common to get Plavix right away, along with aspirin. This combo may continue for up to a year, sometimes a bit longer if you have high risk of clots.
- Stent Placement: After getting a stent, the standard is to stay on Plavix (often with aspirin, a dual therapy) for anywhere from one month to two years, depending on your stent type and how much risk you’re facing. Newer stents (called drug-eluting stents) usually need longer Plavix use than the old bare metal ones.
- Stroke or TIA: If you’ve had a mini-stroke (TIA) or full stroke caused by a clot, Plavix is often the first-choice medicine to stop another episode. Here, some people stay on it for several years, while others may eventually switch to aspirin alone.
You'll sometimes find it prescribed for people with peripheral artery disease (PAD)—that numb, painful leg feeling from clogged leg arteries. In these cases, it helps keep blood flowing down to your toes.
With all these different uses, it’s easy to see how confusion might set in about when to stop. The truth is, only your doctor can decide that, based on what’s happening in your arteries and your overall risk of bleeding (age, kidney health, other medicines). Sometimes, if you need surgery while taking Plavix, you’ll pause it a few days before and restart after, but never decide that on your own—bleeding and clotting both come with serious risks.
Here’s a glimpse from the front lines. Dr. Deepak Bhatt, a well-known cardiologist, summed it up this way:
"The trick with Plavix is finding the right sweet spot—enough to protect you from dangerous clots but not so much that you’re living in fear of every paper cut. It’s not one-size-fits-all, and that’s why talking with your doctor is everything."
Side Effects: The Good, the Bad, and When to Worry
No one likes reading side effects lists, but with Plavix, being aware isn’t about paranoia—it’s about being prepared. The most famous side effect (no surprise here) is bleeding. Nosebleeds, easy bruising, or gum bleeding are common. Most of the time, these aren’t emergencies—just a reminder that your blood isn’t clotting as quickly as before. Keep an eye out, but don’t panic if you notice a bruise that looks nastier than it used to.
Rarely, some people might see heavier bleeding after minor cuts, or even more serious nosebleeds that won’t stop without medical help. Stool or urine that’s black, tarry, or red, coughing up blood, vomiting ‘coffee ground’ stuff—those are all big red flags. Go to the ER straight away if you see anything like that.
A quirky but real tip: some people on Plavix report pinpoint red spots on the skin (petechiae) or strange rashes. While rare, there is a small risk of a very low platelet count called thrombotic thrombocytopenic purpura (TTP). This can show up with unexplained bruises, fever, confusion, or kidney issues. It shows up in just a handful of patients out of every million, but it does happen, so don’t hesitate to call your doctor if something feels really off.
Feeling dizzy or unusually tired? Sometimes, minor anemia from slow, hidden bleeding pops up. It’s not a deal breaker, but worth checking blood counts if you’re feeling weak or short of breath.
On the upside, Plavix doesn’t usually affect your daily energy, and there’s no risk of high blood pressure, kidney damage, or liver trouble in most cases. You also don’t have to avoid foods rich in vitamin K (like with warfarin), so you get a bit more flexibility in your daily meals.
Here are some practical tips:
- Use a soft-bristled toothbrush and electric razor.
- Wear gloves when gardening or doing messy jobs.
- Tell your dentist and any surgeon you’re on Plavix before any procedure, even routine cleanings.
- Avoid contact sports and limit alcohol, since both can boost bleeding risk.
If you’re juggling several medicines, keep a list handy and double-check with your pharmacist that nothing new clashes with Plavix. Herbal stuff like ginkgo, garlic supplements, or fish oil can also increase bleeding risk, so be open about every pill you take, even over-the-counter stuff.

Smart Strategies for Staying Safe on Plavix
Let’s be real—taking Plavix can feel like walking a tightrope between protecting your heart and worrying about every cut or bruise. But millions manage just fine, and a few simple habits can help you dodge most trouble.
- Stick to your routine: Make Plavix as automatic as brushing your teeth. Set alarms, use a pillbox, or pair taking your dose with breakfast.
- Keep an emergency card: A wallet card or phone note that lists 'Taking Plavix' can save precious time if you wind up in the ER or need urgent surgery. Let friends or family know too, especially if you travel often.
- Treat fevers with care: Fevers or infections can change how your body handles Plavix, so let your doctor know if you suddenly feel unwell or spike a fever for more than 48 hours.
- Plan for dental work: Teeth cleaning, extractions, or even deep cleanings can cause bleeding. Dentists now expect to see Plavix patients but always double-check before booking a visit.
- Review all new medications: Always clear every new prescription, supplement, or herbal remedy with your doctor or pharmacist. Some drugs, like certain SSRIs (antidepressants), NSAIDs (like ibuprofen), or proton pump inhibitors, can mess with Plavix or raise your bleeding odds.
- Don’t just stop: Never quit Plavix cold turkey—even for 'just a few days'—without talking to your cardiologist. The rebound risks for a heart attack or stent clot are real and can be deadly.
Ever heard about carrying quick blood clotting agents? Some people who work with tools or play sports keep single-use hemostatic pads in their first aid kits for peace of mind. It’s not overkill; it’s just smart if you drive nails for a living or coach little league.
The future’s bright for anti-platelet therapy—there’s already talk about next-gen drugs that work even faster, wear off quicker, and don’t rely so much on your genes. For now, Plavix remains a proven heavyweight in keeping hearts and brains out of danger. Just remember, every med has its story. Ask questions, keep your team in the loop, and stay curious. That little pink pill only works when you do the simple stuff right—every, single, day.






10 Comments
Becky B
Jun 12 2025Look, the pharma giants love pushing cheap clones like Plavix, and the government quietly backs them with fast‑track approvals. It's not a coincidence that they market it as a miracle without telling you about the hidden bleeding risks. Remember, every big drug rollout has a shadow agenda to keep the healthcare system dependent on patents. Stay vigilant, read the fine print, and don't let the hype swallow your critical thinking.
Aman Vaid
Jun 18 2025Plavix (clopidogrel) is a pro‑drug that requires hepatic conversion via the CYP2C19 pathway to generate its active metabolite. Once activated, it selectively and irreversibly binds to the platelet P2Y12 ADP receptor, thereby inhibiting ADP‑mediated platelet activation and aggregation. This mechanism is fundamentally different from aspirin, which irreversibly acetylates cyclooxygenase‑1, reducing thromboxane A2 synthesis. Clinical trials have demonstrated that dual antiplatelet therapy with aspirin and clopidogrel reduces the composite endpoint of myocardial infarction, stroke, and vascular death by approximately 20–25% compared with aspirin alone. However, the degree of inhibition varies significantly among individuals due to genetic polymorphisms in the CYP2C19 gene. Approximately one in three patients carries loss‑of‑function alleles (*2, *3) that diminish the formation of the active metabolite, resulting in suboptimal platelet inhibition.
Consequently, genotype‑guided therapy has emerged as a precision‑medicine approach, with rapid point‑of‑care tests now available to identify poor metabolizers before initiating therapy. In poor metabolizers, alternative agents such as ticagrelor or prasugrel are recommended because they do not depend on CYP2C19 activation.
Furthermore, drug‑drug interactions can attenuate clopidogrel efficacy. Proton pump inhibitors, particularly omeprazole and esomeprazole, competitively inhibit CYP2C19, reducing the conversion of clopidogrel to its active form. It is advisable to either adjust the timing of administration or select a different acid‑suppressive agent, such as pantoprazole, which has a lower affinity for CYP2C19.
Bleeding risk remains the primary safety concern. The pharmacodynamic effect of clopidogrel is dose‑dependent; however, increasing the dose does not proportionally increase bleeding risk, but rather may improve antiplatelet effect in resistant individuals. The typical maintenance dose is 75 mg once daily, and dose escalation should only be considered under specialist supervision.
In summary, the effectiveness of Plavix hinges on proper metabolic activation, awareness of genetic variability, and vigilant management of potential drug interactions. Tailoring therapy based on genotype and concomitant medications can optimize outcomes while minimizing adverse events.
xie teresa
Jun 25 2025Reading this brings back memories of my dad’s stent procedure-he was terrified of the bleeding scares, but with the right guidance he managed just fine. It helps to know that missing a dose can let platelets bounce back in a week, so setting a daily alarm really makes a difference. Also, keep a small card in your wallet that says you’re on Plavix; it’s a lifesaver if you ever end up in an ER. And don’t forget to let your dentist know before any cleaning-you’ll avoid those nasty post‑procedure bleeds. Stay safe and keep supporting each other!
Srinivasa Kadiyala
Jul 2 2025Interesting how the article glosses over the fact that not all patients respond equally to clopidogrel; indeed, the variability is scientifically documented, yet media narratives often ignore such nuance, perpetuating a simplistic view, which feels almost negligent, don’t you think? Moreover, the emphasis on “one‑size‑fits‑all” dosage overlooks the impact of CYP2C19 polymorphisms-an area where genetics clearly informs pharmacology; consequently, a more individualized approach would be prudent, especially when considering alternative agents. Lastly, the claim that “most patients have no serious side effects” should be contextualized with epidemiological data, rather than presented as an absolute.
Alex LaMere
Jul 8 2025Plavix works, but watch out for interactions. Omeprazole can blunt its effect 🚫. Keep a pillbox; it saves you from missed doses 👍.
Dominic Ferraro
Jul 15 2025Take heart-you’re already doing the hardest part by staying informed. Pair your daily dose with a habit you already love, like a morning coffee, and you’ll never miss it. If you’re headed for a dental appointment, a quick call to the office lets them prep the right protocol, sparing you unnecessary bleeding. And remember, a quick check‑in with your pharmacist about new supplements can preempt hidden risks. Small steps, big peace of mind!
Jessica Homet
Jul 22 2025Honestly, the hype around Plavix feels overblown; you’ll see random bruises and think it’s dangerous, but most of the time it’s just your body adjusting. If you’re not into constant worry, maybe skip the extra supplements that claim to “boost” its effect-most of them just increase bleed risk. Bottom line: stick to the prescription, avoid unnecessary meds, and you’ll be fine.
mitch giezeman
Jul 25 2025Good points on staying cautious with extra supplements; many over‑the‑counter products can indeed heighten bleeding. It’s worth noting that if you ever need surgery, the standard practice is to hold Plavix for about five days to let platelet function recover. Also, if you notice unexplained bruising that’s worsening, a quick CBC can rule out hidden anemia. Keep a medication list handy for any new doctor visits.
Kelly Gibbs
Aug 1 2025Never skip a dose unless your doctor says so.
KayLee Voir
Aug 8 2025Remember, consistency is key-set a simple reminder and stick to it. If you ever feel uneasy about bleeding, a brief chat with your healthcare team can reassure you and adjust the plan if needed. You’ve got this, and we’re all here cheering you on.