Graves' Disease Probiotic Selector
Personalized Probiotic Recommendations
Select your primary digestive symptoms and medications to get tailored probiotic recommendations based on Graves' disease management research.
Recommended Probiotic
Lactobacillus reuteri
Supports immune regulationThis strain reduces inflammatory cytokines associated with thyroid autoimmunity.
For Graves' disease patients with diarrhea, this strain helps balance gut flora while supporting immune regulation.
Probiotic Comparison Guide
| Strain | Key Benefit | Typical Dose (CFU) | Best For |
|---|---|---|---|
| Lactobacillus reuteri | Reduces inflammatory cytokines | 1-2 billion | Immune regulation, diarrhea |
| Bifidobacterium longum | Supports gut barrier integrity | 5-10 billion | IBS symptoms, gut healing |
| Saccharomyces boulardii | Helps with diarrhea from medication | 5-10 billion | Medication-induced diarrhea |
When it comes to managing Graves' disease is a chronic autoimmune condition that overstimulates the thyroid gland, leading to excess thyroid hormone production, most people focus on blood tests and medication. Yet the gut often suffers in silence, and a troubled digestive system can amplify thyroid symptoms, fuel inflammation, and even interfere with treatment effectiveness. This guide walks you through the gut‑thyroid connection and gives clear, everyday steps to keep your digestive tract running smoothly while you manage Graves' disease.
Why the Gut Matters for Graves' Disease
The gut microbiome is a community of trillions of bacteria, fungi, and viruses that live in your intestines. Research shows that an imbalanced microbiome (dysbiosis) can trigger or worsen autoimmune responses, including the production of thyroid‑stimulating antibodies. Moreover, the gut lines the pathway for nutrient absorption; deficiencies in selenium, zinc, or vitamin D-key players in thyroid metabolism-often stem from poor gut health. In short, a healthy gut helps keep the immune system calm and ensures your body gets the minerals it needs to regulate thyroid hormones.
How Graves' Disease Affects Your Digestive System
Excess thyroid hormone speeds up metabolism, which can accelerate gastric emptying. The result? Frequent bowel movements, diarrhea, or sometimes a feeling of constant urgency. Additionally, many patients experience heightened anxiety, which can lead to irritable bowel syndrome (IBS)‑like symptoms. Medications such as methimazole can also disrupt gut flora, especially when taken long‑term.
Core Gut‑Health Pillars for Thyroid Patients
- Balanced microbiome - Support diversity with fermented foods and targeted probiotics.
- Adequate fiber intake - Soluble fiber (e.g., oats, chia) helps regulate blood sugar and eases bowel transit.
- Optimal iodine levels - While iodine excess can aggravate Graves', a modest amount is essential for hormone synthesis.
- Stress management - Chronic stress raises cortisol, which can interfere with thyroid conversion.
- Consistent sleep - Poor sleep disrupts the gut’s circadian rhythm and may increase autoimmunity.

Nutrition Strategies That Really Work
1. Choose the right probiotic. Not all strains are equal. Lactobacillus reuteri and Bifidobacterium longum have the strongest evidence for modulating immune markers in thyroid disorders.
| Strain | Key Benefit | Typical Dose (CFU) |
|---|---|---|
| Lactobacillus reuteri | Reduces inflammatory cytokines | 1‑2 billion |
| Bifidobacterium longum | Supports gut barrier integrity | 5‑10 billion |
| Saccharomyces boulardii | Helps with diarrhea from medication | 5‑10 billion |
2. Eat fiber-rich foods. Aim for 25‑30 g of fiber daily. Good sources include berries, legumes, whole grains, and leafy greens. Pair soluble fiber with healthy fats (avocado, olive oil) to slow glucose spikes, which can otherwise trigger anxiety.
3. Mind iodine. Seaweed, dairy, and iodized salt are common iodine sources. For Graves' disease, keep daily iodine below 150 µg unless your doctor advises otherwise. Use non‑iodized sea salt for seasoning and limit kelp snacks.
4. Add selenium and zinc. Both minerals assist the enzyme that converts T4 to the active T3 form. Brazil nuts (one‑two per day) provide ~200 µg selenium; pumpkin seeds deliver zinc.
5. Stay hydrated. Water supports mucus production and smooth bowel movements. Aim for at least 2 L daily, more if you’re sweating from hypermetabolism.
Lifestyle Habits to Keep the Gut Calm
- Stress reduction - Try guided breathing, yoga, or short walks. Even five minutes of diaphragmatic breathing can lower cortisol and improve gut motility.
- Regular sleep schedule - Keep bedtime consistent; target 7‑8 hours of deep sleep.
- Gentle exercise - Low‑impact activities like swimming or cycling help regulate bowel movements without overstimulating the nervous system.
- Avoid trigger foods - Highly processed meals, excess caffeine, and artificial sweeteners often provoke diarrhea or bloating in thyroid patients.
Common Pitfalls and Red Flags
Even with a solid plan, some habits can sabotage gut health:
- Self‑prescribing supplements - High‑dose iodine or selenium can worsen autoimmunity. Always check with your endocrinologist.
- Skipping meals - Irregular eating can lead to blood‑sugar swings, feeding anxiety and gut dysbiosis.
- Over‑reliance on laxatives - They mask underlying gut issues and can deplete electrolytes, worsening thyroid symptoms.
If you notice persistent abdominal pain, unexplained weight loss, or new skin changes, schedule a follow‑up. These could signal a secondary condition such as celiac disease, which shares a genetic link with many autoimmune disorders.

7‑Day Sample Meal Plan (Gut‑Friendly & Thyroid‑Supportive)
- Day 1: Breakfast - Greek yogurt with chia seeds, blueberries, and a sprinkle of cinnamon; Lunch - Quinoa salad with roasted pumpkin, spinach, and a handful of Brazil nuts; Dinner - Grilled salmon, steamed broccoli, and a side of lentil soup.
- Day 2: Breakfast - Overnight oats with almond milk, sliced kiwi, and 1 g of probiotic powder; Lunch - Turkey lettuce wraps with avocado and fermented kimchi; Dinner - Stir‑fried tofu, bok choy, and brown rice.
- Day 3: Breakfast - Scrambled eggs with sautéed mushrooms and a slice of sourdough; Lunch - Chickpea and beetroot salad with feta; Dinner - Baked cod, roasted carrots, and a small sweet potato.
- Day 4: Breakfast - Smoothie (spinach, banana, kefir, flaxseed); Lunch - Lentil and vegetable stew; Dinner - Grass‑fed beef steak, quinoa pilaf, and steamed asparagus.
- Day 5: Breakfast - Cottage cheese with pineapple chunks and pumpkin seeds; Lunch - Salmon sashimi bowl with seaweed, cucumber, and brown rice; Dinner - Chicken curry with coconut milk, cauliflower rice.
- Day 6: Breakfast - Buckwheat pancakes topped with fresh berries; Lunch - Greek salad with olives, cucumber, and a drizzle of olive oil; Dinner - Shrimp stir‑fry with bell peppers and soba noodles.
- Day 7: Breakfast - Miso soup with tofu and scallions; Lunch - Roasted vegetable quinoa bowl; Dinner - Turkey meatballs in tomato sauce with spaghetti squash.
Adjust portion sizes based on your calorie needs, and keep a food journal to spot patterns that affect your gut.
Quick Checklist for a Thyroid‑Friendly Gut
- Take a daily probiotic containing Lactobacillus reuteri or Bifidobacterium longum.
- Consume 25‑30 g of fiber from whole foods.
- Limit iodine to <150 µg/day unless advised otherwise.
- Include selenium (Brazil nuts) and zinc (pumpkin seeds) 3‑4 times per week.
- Stay hydrated - at least 2 L water daily.
- Practice stress‑relief techniques for 5 minutes each day.
- Maintain a regular sleep‑wake schedule.
Frequently Asked Questions
Can probiotics really affect my Graves' disease?
Yes. Certain strains, especially Lactobacillus reuteri and Bifidobacterium longum, have been shown in small clinical trials to lower inflammatory markers and improve gut barrier function, which can indirectly lessen autoimmune activity.
Should I avoid all iodine because I have Graves' disease?
Not entirely. Iodine is needed for thyroid hormone production, but excess iodine can trigger flare‑ups. Aim for the recommended daily allowance (150 µg) and avoid large servings of seaweed or iodine‑rich supplements unless a doctor advises otherwise.
My medication gives me diarrhea. What can I do?
Talk to your endocrinologist about adjusting the dose or switching to an alternative like propylthiouracil. Meanwhile, adding a probiotic with Saccharomyces boulardii and increasing soluble fiber can help normalize stool consistency.
Is a low‑carb diet safe for Graves' disease?
A moderate low‑carb approach can work, but extreme restriction may aggravate stress hormones and gut dysbiosis. Balance carbs with plenty of fiber‑rich vegetables to keep the microbiome happy.
How often should I check my gut health?
If you’re actively managing Graves', a quarterly review of digestive symptoms (bowel habits, bloating, nutrient levels) with your healthcare team is reasonable. Lab tests for vitamin D, B12, and zinc can flag hidden deficiencies.







8 Comments
Poornima Ganesan
Oct 18 2025Alright, let’s cut to the chase because the scientific community has already spelled out what most of us are still fumbling around for.
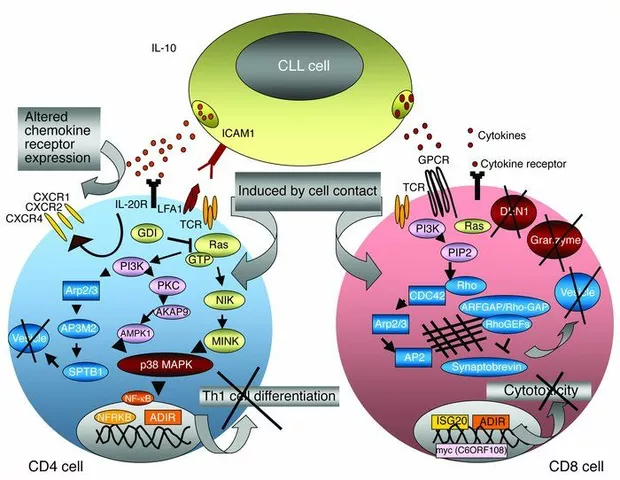
First, your gut microbiome isn’t just a passive collection of microbes; it actively modulates the immune system through pattern‑recognition receptors and cytokine signaling pathways.
When dysbiosis sets in, you essentially give the immune system a free pass to start producing auto‑antibodies, including the dreaded thyroid‑stimulating immunoglobulins that drive Graves' disease.
Second, nutrient malabsorption isn’t a myth – a leaky gut can literally prevent you from absorbing selenium, zinc, and vitamin D, all of which are cofactors in the conversion of T4 to T3.
Third, the hyper‑metabolic state of Graves' disease accelerates gastric emptying, which means you’ll often experience diarrhea, urgency, and an overall chaotic bowel routine.
Fourth, let’s not forget that common antithyroid drugs like methimazole have antimicrobial properties that can further destabilize your gut flora if taken long‑term.
Now, on to actionable steps: start a probiotic regimen that includes Lactobacillus reuteri and Bifidobacterium longum – these strains have been shown in multiple peer‑reviewed studies to reduce inflammatory cytokines and reinforce tight‑junction proteins.
Couple that with a daily prebiotic fiber source such as inulin or resistant starch to feed those beneficial bacteria.
Don’t overlook fermented foods like sauerkraut, kefir, and kimchi, which provide both live cultures and bioactive compounds that can modulate immune signaling.
When it comes to iodine, the mantra is “less is more” for Graves' patients: stay under 150 µg per day unless your endocrinologist tells you otherwise, and avoid high‑iodine seaweed snacks.
Every teaspoon of iodized salt can push you over the threshold, so opt for non‑iodized sea salt if you must season your meals.
For selenium, a single Brazil nut a day delivers roughly 200 µg, which is sufficient to support selenoprotein activity without risking toxicity.
Similarly, a handful of pumpkin seeds will cover your zinc needs, helping the enzyme deiodinase that converts T4 to the active T3 form.
Hydration is non‑negotiable: aim for at least 2 L of water daily, adjusting upward if you sweat profusely due to hypermetabolism.
Stress management isn’t a buzzword – chronic cortisol elevation directly impairs the gut barrier and can exacerbate autoimmunity, so incorporate at least five minutes of diaphragmatic breathing or yoga each day.
Finally, make sleep a priority; a consistent 7‑8‑hour schedule aligns the gut’s circadian rhythm and supports overall immune homeostasis.
Rajesh Singh
Oct 19 2025Honestly, if you’re not already on a probiotic, you’re basically inviting your own immune system to betray you.
Matthew Miller
Oct 21 2025Hey everyone, just wanted to shout out how much energy I get from a solid gut routine – it’s like fueling a high‑performance engine!
Start your day with a probiotic shake, pack in some fiber‑rich berries, and keep your iodine intake in check.
Remember, consistency beats perfection – even a small daily habit stacks up to big results over weeks.
Alex Lineses
Oct 22 2025Great points, Matthew! To add some clinical context, integrating prebiotic fibers such as Oatβ‑Glucan can synergize with probiotic strains by enhancing SCFA production, which in turn promotes regulatory T‑cell differentiation.
Practically, try sprinkling a tablespoon of ground flaxseed into your morning smoothie – you’ll boost both soluble fiber and omega‑3 intake, supporting thyroid hormone conversion.
Wyatt Schwindt
Oct 23 2025Take a probiotic daily.
Lyle Mills
Oct 24 2025Daily probiotic plus 25‑30g fiber works; keep iodine low.
Barbara Grzegorzewska
Oct 25 2025Look, I’ve read a gazillion articles and let me tell ya, the whole “just eat a salad” mantra is pure baloney unless you’re also watching your iodine like a hawk.
These elite nutrition gurus love to sprinkle fancy terms like “microbiome diversity index” but forget that most of us are just trying not to poop in public.
If you’re serious, ditch the processed junk, grab a handful of Brazil nuts, and sip kefir like it’s the elixir of the gods – not because it’s trendy, but because the science backs it up.
Nis Hansen
Oct 26 2025Barbara, your vivid description captures the urgency of a holistic approach.
Philosophically, the gut‑thyroid axis exemplifies the interconnectedness of bodily systems; neglecting one compromises the harmony of the whole.
Practically, I would recommend a structured schedule: morning probiotic, mid‑day fiber-rich meal, evening low‑iodine dinner, and a nightly mindfulness routine to modulate cortisol.
This integrative protocol respects both empirical evidence and the lived experience of patients.