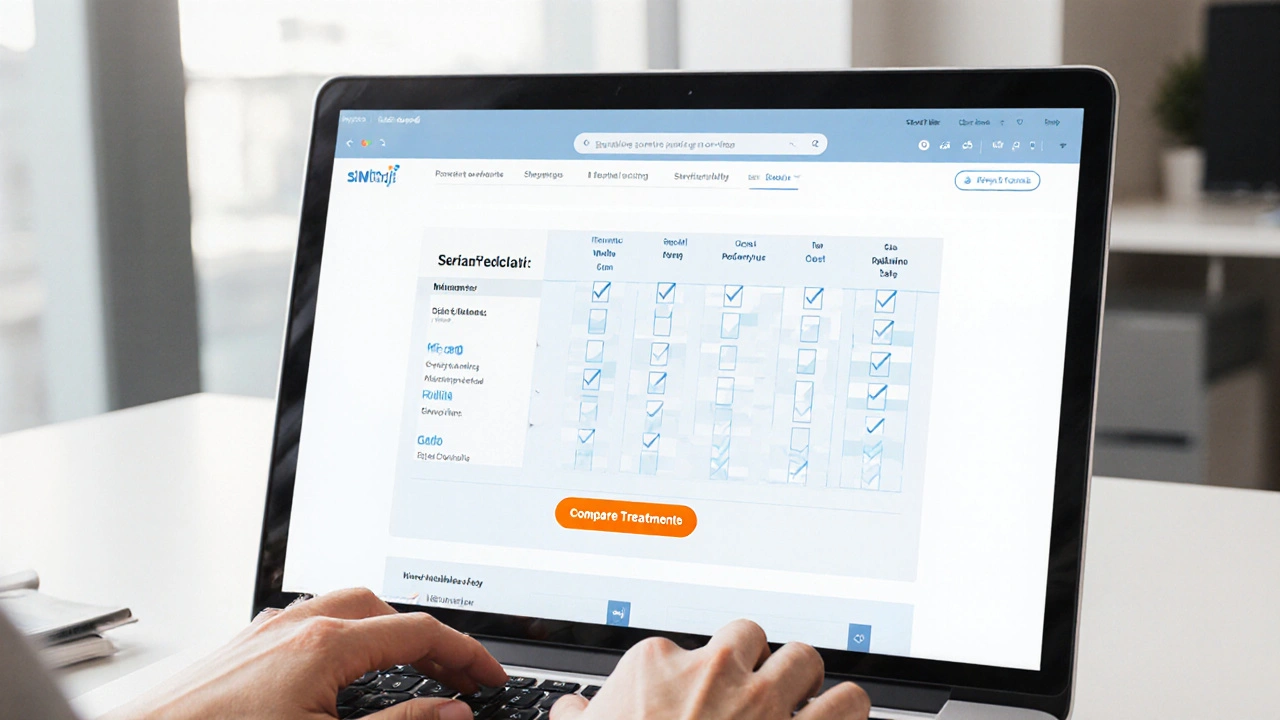
Dapsone vs. Alternatives Comparison Tool
Select Treatment Criteria
Choose factors that matter most for your treatment decision.
Treatment Comparison Results
Based on your selected criteria, here's how Dapsone compares to its alternatives:
| Drug | Efficacy | Side Effects | Cost | Interactions | Convenience | Special Safety |
|---|---|---|---|---|---|---|
| Dapsone | ★★★☆☆ | ★★☆☆☆ | ★★★★☆ | ★★★☆☆ | ★★★★★ | ★★☆☆☆ |
| Sulfapyridine | ★★★☆☆ | ★★★★☆ | ★★★★★ | ★★★☆☆ | ★★★★★ | ★★★☆☆ |
| Sulfamethoxazole | ★★★★☆ | ★★★☆☆ | ★★★★★ | ★★★☆☆ | ★★★★★ | ★★★★☆ |
| Minocycline | ★★★★☆ | ★★★☆☆ | ★★★★☆ | ★★★★☆ | ★★★★★ | ★★☆☆☆ |
| Rifampin | ★★★★★ | ★★☆☆☆ | ★★★☆☆ | ★★☆☆☆ | ★★★★★ | ★★★☆☆ |
| Clofazimine | ★★★★☆ | ★★★☆☆ | ★★☆☆☆ | ★★★☆☆ | ★★★★☆ | ★★★★☆ |
Quick Summary
- Dapsone is effective for leprosy and dermatitis herpetiformis but carries a risk of hemolysis and liver toxicity.
- Common alternatives include Sulfapyridine, Sulfamethoxazole, Minocycline, Rifampin, and Clofazimine.
- When choosing an alternative, consider disease focus, side‑effect profile, drug‑interaction risk, and cost.
- Rifampin and Clofazimine are the go‑to partners for multi‑drug leprosy regimens, while Minocycline is often favored for acne‑type or inflammatory skin issues.
- Always discuss lab monitoring and pregnancy safety with your prescriber before switching.
What Is Dapsone?
Dapsone is a synthetic sulfone antibiotic that’s been used for decades to treat leprosy, dermatitis herpetiformis, and certain types of pneumonia. It works by inhibiting bacterial dihydropteroate synthase, which blocks folate synthesis, and also has anti‑inflammatory properties that help skin conditions.
Typical oral dose for leprosy: 100mg once daily. For dermatitis herpetiformis, the dose is usually 50‑150mg per day, split as needed. The drug is absorbed well (≈80% bioavailability) and has a half‑life of 20-30hours, allowing once‑daily dosing.
Key Criteria for Comparing Treatments
When you line up Dapsone against other meds, these six factors usually decide which one wins:
- Clinical efficacy - how well the drug clears the infection or skin rash.
- Side‑effect profile - especially hemolysis, liver enzymes, and hypersensitivity.
- Dosing convenience - number of pills per day and need for food.
- Drug‑interaction risk - especially with antibiotics, anticoagulants, or HIV meds.
- Cost & insurance coverage - out‑of‑pocket price in 2025 US dollars.
- Special population safety - pregnancy, children, renal or hepatic impairment.
Common Alternatives to Dapsone
Below are the most frequently considered substitutes. Each entry starts with a micro‑data block so search engines can recognize the entity.
Sulfapyridine is a sulfonamide used historically for dermatitis herpetiformis and ulcerative colitis. It works similarly to Dapsone by blocking folate synthesis, but it tends to cause more gastrointestinal upset.
Sulfamethoxazole (often combined with trimethoprim as co‑trimoxazole) is a broad‑spectrum sulfonamide antibiotic. It’s a go‑to for Pneumocystis jirovecii prophylaxis and urinary‑tract infections, and can replace Dapsone in some skin‑related infections.
Minocycline is a tetracycline‑class antibiotic with strong anti‑inflammatory activity. Dermatologists love it for acne, rosacea, and some forms of chronic hives, making it a popular Dapsone alternative for inflammatory skin disease.
Rifampin is a potent bactericidal drug that targets RNA polymerase. It’s a cornerstone of multi‑drug therapy for leprosy and also treats tuberculosis. Rifampin has a known interaction with many oral contraceptives, which is key to consider.
Clofazimine is a phenazine dye with anti‑mycobacterial activity. It’s used as a second‑line agent for leprosy and for some resistant skin infections. The main drawback is skin discoloration, which can be striking.
Side‑by‑Side Comparison
| Drug | Primary Uses | Typical Oral Dose | Common Side Effects | Cost (US$/month) | Interaction Risk |
|---|---|---|---|---|---|
| Dapsone | Leprosy, dermatitis herpetiformis, PCP prophylaxis | 50‑100mg daily | Hemolysis (esp. G6PD‑def.), methemoglobinemia, liver enzyme elevation | ≈$30 | Medium - interacts with isoniazid, warfarin |
| Sulfapyridine | Dermatitis herpetiformis, ulcerative colitis | 500‑1000mg daily | GI upset, rash, sulfa allergy | ≈$25 | Low - similar sulfa class |
| Sulfamethoxazole | UTI, PCP prophylaxis, respiratory infections | 800mg daily (often with trimethoprim) | Kidney stones, nausea, photosensitivity | ≈$15 | Medium - strong CYP450 inducer |
| Minocycline | Acne, rosacea, inflammatory dermatoses | 100mg twice daily | Dizziness, vestibular toxicity, hyperpigmentation | ≈$20 | Low - minor with oral contraceptives |
| Rifampin | Leprosy (multidrug), TB, MRSA prophylaxis | 600mg daily | Hepatotoxicity, orange body fluids, drug interactions | ≈$45 | High - induces many CYP enzymes |
| Clofazimine | Leprosy (multidrug), Mycobacterium infections | 100mg daily | Skin discoloration, GI cramps, QT prolongation | ≈$80 | Medium - interacts with warfarin, methadone |
When One Alternative Beats Dapsone
Dapsone alternatives shine in specific scenarios:
- Pregnant or breastfeeding patients: Dapsone crosses the placenta and can cause neonatal hemolysis. Minocycline is contraindicated in pregnancy, so sulfamethoxazole‑trimethoprim (after the first trimester) or rifampin may be safer choices.
- G6PD deficiency: Hemolysis risk is high with Dapsone. Switch to sulfapyridine (still a sulfa but less hemolytic) or use a non‑sulfonamide like minocycline.
- Multi‑drug leprosy regimen: The WHO recommends Dapsone + Rifampin + Clofazimine. If Dapsone must be stopped, increase rifampin dose and add a fluoroquinolone (e.g., ofloxacin) as a substitute.
- Chronic dermatitis with severe itch: Minocycline’s anti‑inflammatory effect often clears symptoms faster than Dapsone, especially when acne is also present.
- Cost‑sensitive settings: Sulfamethoxazole‑trimethoprim is the cheapest option for PCP prophylaxis, while Dapsone remains modestly priced for leprosy bundles.
Safety & Monitoring Tips
Regardless of the drug you end up on, regular lab work saves headaches:
- Baseline CBC, liver function tests (ALT/AST), and G6PD screening before starting Dapsone or any sulfonamide.
- Repeat CBC and LFTs every 2‑4weeks for the first three months, then quarterly.
- Watch for orange‑red urine with rifampin; it’s harmless but can alarm patients.
- If you notice new skin discoloration, especially with clofazimine, discuss dose adjustments - discoloration is dose‑related and often reversible.
How to Talk to Your Doctor About Switching
Come prepared with a short list:
- Current dose and why you think it’s not working (side effects, lack of relief, etc.).
- Any lab results you have (CBC, LFTs, G6PD).
- Specific concerns-pregnancy, cost, drug interactions.
- Ask about the monitoring schedule for the alternative.
A clear, focused conversation makes it easier for your prescriber to pick the right replacement and set up the right follow‑up.
Frequently Asked Questions
Can I take Dapsone and Rifampin together?
Yes, they’re often combined in the WHO‑recommended triple therapy for leprosy. However, Rifampin speeds up Dapsone metabolism, so doctors may monitor blood levels more closely.
What should I do if I develop a rash on Dapsone?
Stop the drug immediately and contact your clinician. A rash may signal a hypersensitivity reaction that could progress to Stevens‑Johnson syndrome, especially when combined with other sulfonamides.
Is Sulfamethoxazole a safe replacement for Dapsone in pregnancy?
After the first trimester, sulfamethoxazole‑trimethoprim is generally considered safe, but folate supplementation is recommended because the drug interferes with folate metabolism.
Why does Clofazimine turn my skin red?
Clofazimine is a pigmented dye; it deposits in fatty tissues and skin, causing a reddish‑brown hue. The change is cosmetic, not harmful, and often fades once the drug is stopped.
Do I need to avoid sunlight while on Minocycline?
Minocycline can cause photosensitivity in some people, so using sunscreen and limiting intense sun exposure is advisable, especially if you have a history of sunburn.

Next Steps
Now that you’ve seen the pros and cons, pick the factor that matters most for you - be it safety, cost, or disease‑specific efficacy - and bring that priority to your next appointment. With the right lab monitoring and an open dialogue, you’ll land on a regimen that keeps you feeling better without unnecessary side effects.







15 Comments
Melissa Shore
Oct 1 2025Dapsone has been a mainstay in dermatology for decades. Its dual antimicrobial and anti‑inflammatory actions make it uniquely suited for conditions such as leprosy and dermatitis herpetiformis. When clinicians evaluate a regimen they must balance efficacy with safety in a systematic way. The comparison table highlights how Dapsone scores moderately on efficacy while excelling in dosing convenience. However the side‑effect profile especially hemolysis in G6PD deficient patients remains a serious concern. In practice the need for regular blood work can deter some prescribers from choosing it as first line. Alternatives such as sulfamethoxazole offer comparable efficacy with a lower risk of hemolysis but bring their own issues like renal stone formation. Minocycline provides strong anti‑inflammatory benefits for acne like presentations yet its vestibular toxicity limits its use in certain populations. Rifampin stands out for its high efficacy in leprosy but its enzyme induction can compromise hormonal contraceptives and many other drugs. Clofazimine’s hallmark skin discoloration may be cosmetically unacceptable for many patients despite its decent efficacy. Cost considerations also shift the balance as Dapsone is relatively inexpensive compared with newer agents. Insurance coverage often favors older generics making Dapsone a financially viable option for many. The decision matrix should also incorporate patient specific factors such as pregnancy status or renal function. For a pregnant patient the risk of neonatal hemolysis pushes the clinician toward alternatives like sulfamethoxazole after the first trimester. In G6PD deficient individuals the safest route is to avoid sulfonamides altogether and consider agents without a sulfa backbone. Ultimately a shared decision making process that reviews these nuances yields the most appropriate therapeutic choice.
Maureen Crandall
Oct 8 2025This tool is way overkill.
Michelle Pellin
Oct 15 2025While the comparative chart is undeniably thorough, one cannot ignore the theatrical flair with which Dapsone’s side‑effect profile is presented; it reads like a melodrama of red blood cells and liver enzymes. The author deftly balances factual rigor with a hint of literary panache, turning pharmacology into a stage performance. Yet, beneath the curtain‑call of star‑rated ratings, the real protagonists are the patients who navigate these trade‑offs daily. In that sense the piece succeeds in both informing and captivating the audience.
Keiber Marquez
Oct 22 2025Yo Dapsone is a real american classic its just a sufa the way its put together in the table is kinda stupid we should push for more home grown meds u know.
Lily Saeli
Oct 29 2025Philosophically speaking the choice of a drug is a moral decision; we must ask ourselves if we are willing to risk hemolysis for the sake of convenience. The article presents data but fails to confront the ethical weight of prescribing a medication that can cause irreversible harm to vulnerable populations. A truly responsible clinician would weigh these values before making a recommendation.
Joshua Brown
Nov 5 2025Great overview! , I’d add that monitoring CBC and LFTs every 2–4 weeks during the first three months can catch early signs of hemolysis, , and patients on rifampin should be warned about the orange‑red discoloration of bodily fluids, , which is harmless but often alarming. , Also, consider drug‑interaction checklists for warfarin and oral contraceptives when prescribing rifampin, , as it can significantly reduce their efficacy. ,
andrew bigdick
Nov 12 2025Interesting tool, i think it’s handy for quick decisions but always double check with a doc before switching meds.
Shelby Wright
Nov 19 2025Oh wow, another chart trying to claim Dapsone is the ultimate hero-sure, if you love side‑effects like a fireworks show on your bloodstream! Let’s not forget that alternatives can sparkle just as brightly without the same drama.
Ellen Laird
Nov 26 2025The table is quite elte, but the use of rating stars is a bit childlike. A more sophisticted approach would involve statistical confidence intervals rather than simplistic ★ symbols.
rafaat pronoy
Dec 3 2025Nice comp, tho looks a bit heavy on data – kinda makes me want a ☕ while I read through all the rows.
Matt Miller
Dec 10 2025Good summary, concise and to the point.
Fabio Max
Dec 17 2025Love the balanced view! It’s refreshing to see both pros and cons laid out without bias.
Darrell Wardsteele
Dec 24 2025While the article is thorough, it suffers from inconsistent formatting and occasional typographical errors which detract from its professionalism. Moreover, the lack of citation for the cost data raises questions about its reliability. A more rigorous editorial process would improve credibility.
Heather Wilkinson
Dec 30 2025Thanks for the thorough explanation, Joshua! 😊 Your tips on monitoring are spot‑on and will help many avoid nasty surprises.
Neha Bharti
Jan 6 2026Melissa, your deep dive really clarifies the trade‑offs-appreciate the balanced perspective.