Warfarin-NSAID Interaction Risk Calculator
WARNING: Combined Use is DANGEROUS
Combining warfarin with any NSAID significantly increases bleeding risk. This calculator shows relative risk multipliers based on current medical evidence.
Risk Assessment
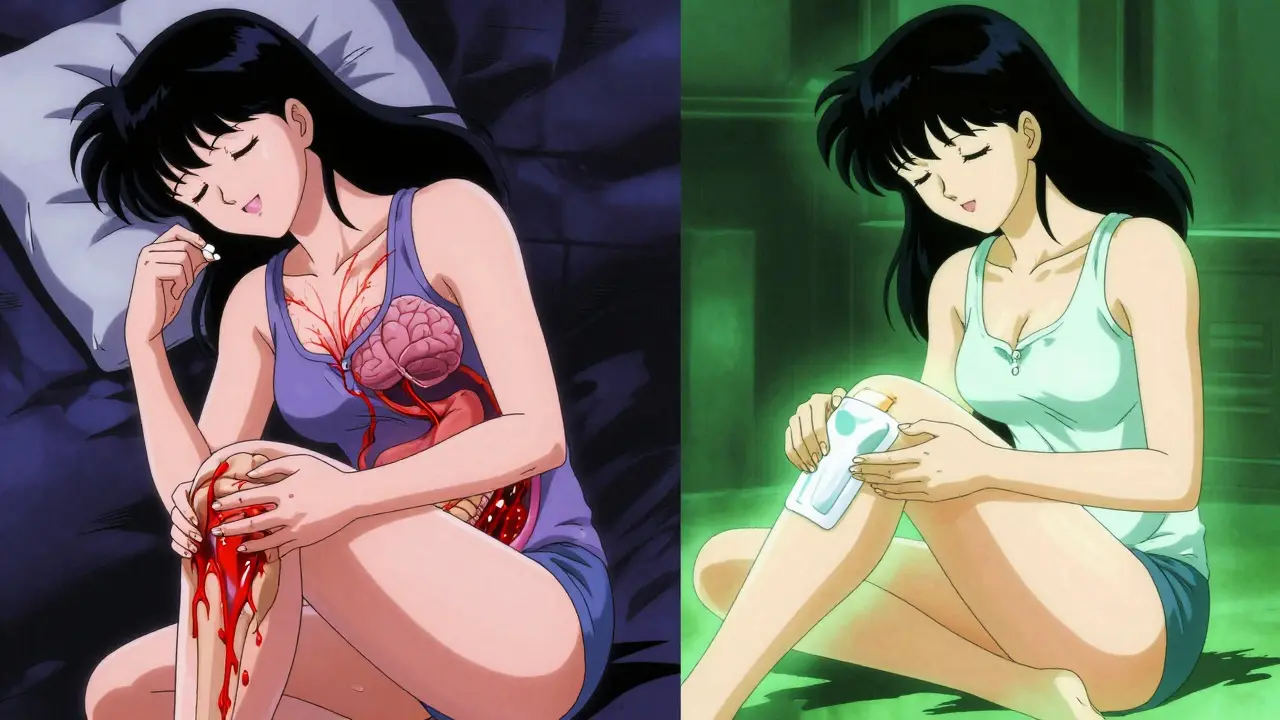
When you’re on warfarin, even a simple headache can become a dangerous decision. Taking an over-the-counter NSAID like ibuprofen or naproxen might seem harmless-after all, millions do it every day. But here’s the truth: combining these two medications doesn’t just raise your risk of bleeding. It multiplies it. And the consequences aren’t theoretical-they’re happening right now, in hospital emergency rooms and at kitchen tables across the country.
Why Warfarin and NSAIDs Don’t Mix
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. That’s why it’s so effective at preventing strokes and blood clots. But NSAIDs? They attack clotting from a different angle. They shut down cyclooxygenase (COX) enzymes, which do two things: they reduce inflammation and pain, and they help platelets stick together to form clots. When you take both, you’re not just slowing down clotting-you’re nearly disabling it on two fronts. This isn’t a minor concern. A 2023 study from Aarhus University Hospital found that people on warfarin who also took NSAIDs had more than double the risk of bleeding compared to those on warfarin alone. That’s not a 10% increase. That’s a 2.09-fold jump. And it doesn’t matter if you’re taking a low-dose NSAID or a prescription-strength one. The risk is there.Not All NSAIDs Are Created Equal
If you think all NSAIDs are the same, you’re in danger. Some are far worse than others when paired with warfarin.- Naproxen: 4.1 times higher bleeding risk
- Diclofenac: 3.3 times higher risk
- Meloxicam: 2.8 times higher risk
- Ibuprofen: 1.79 times higher risk
COX-2 Inhibitors Aren’t Safer Than You Think
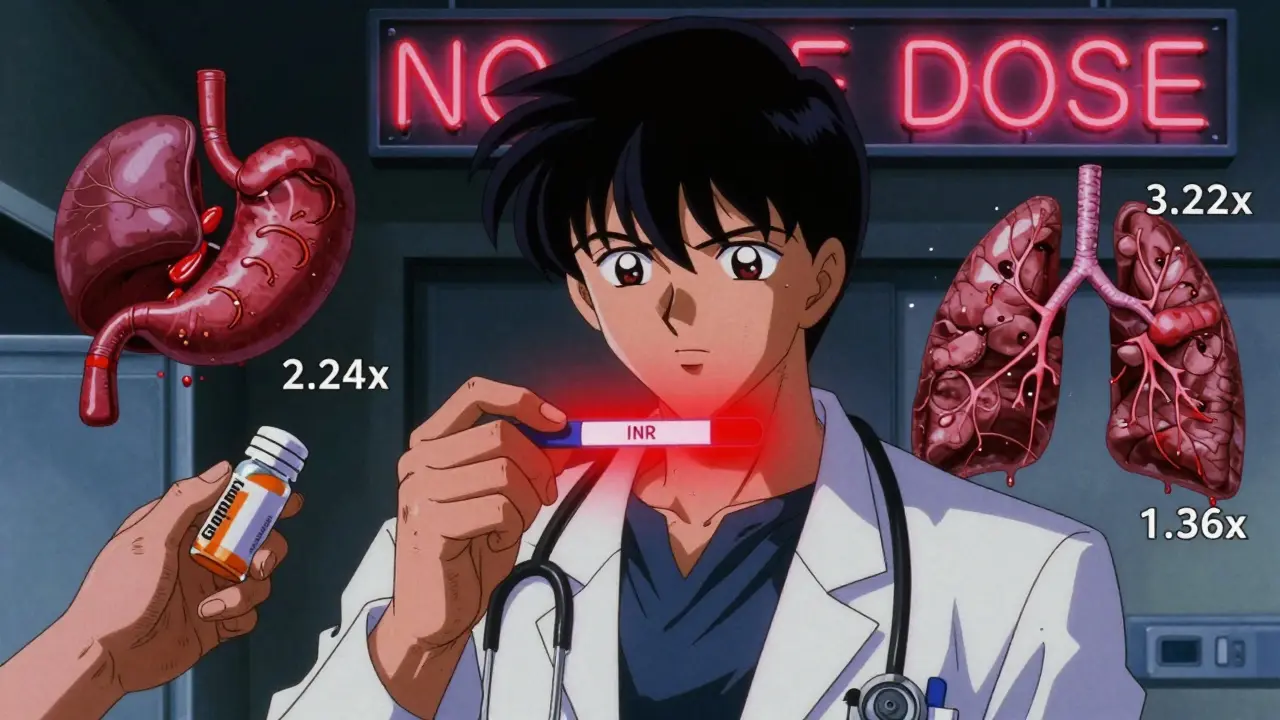
You might have heard that drugs like celecoxib (Celebrex) are "safer" because they don’t affect the stomach lining as much. That’s true for ulcers-but not for bleeding. Multiple studies, including a 2020 meta-analysis in PMC, show that COX-2 inhibitors carry the same bleeding risk as traditional NSAIDs when taken with warfarin. In fact, gastrointestinal bleeding risk nearly doubles with any NSAID, regardless of selectivity. The idea that selective COX-2 inhibitors are safe with blood thinners? That’s a myth.Where the Bleeding Happens
It’s not just one kind of bleed. The combination hits multiple organs:- Gastrointestinal: 2.24-fold increase (most common)
- Intracranial: 3.22-fold increase (deadliest)
- Urinary tract: 1.57-fold increase
- Lungs: 1.36-fold increase
What About Newer Blood Thinners? (NOACs)
Many people switch from warfarin to dabigatran, rivaroxaban, or apixaban thinking they’re "safer"-and they are, in many ways. But they’re not safe with NSAIDs. A 2018 JACC study showed NSAID use increased major bleeding with both warfarin and dabigatran. The ARISTOTLE trial found that even apixaban, often considered the safest NOAC, still carries a significantly higher bleeding risk when combined with NSAIDs. And here’s the scary part: a 2023 study found that NSAID co-prescribing with NOACs increased by 34.8% between 2015 and 2022. People are assuming NOACs = safe with painkillers. They’re wrong.Real People, Real Consequences
Reddit threads, patient forums, and hospital records tell the same story. One user on r/BloodThinners wrote: "Took ibuprofen for a headache. 24 hours later, my hemoglobin dropped from 14 to 8. I was in the ER. I didn’t even know I was bleeding inside." A 2021 study of 5,237 warfarin users found that 78.4% of those who bled while on NSAIDs needed hospitalization. Their average stay? Over five days. That’s not just a medical emergency-it’s lost wages, lost time, lost peace of mind. Drugs.com reviews for this combination average a 2.1 out of 10 safety rating. Eighty-seven percent of 1,452 reviews say: "Don’t do it."What Should You Do Instead?
There are alternatives. And they’re safer.- Acetaminophen (Tylenol): The #1 recommended alternative. It doesn’t affect platelets or the stomach lining. Dose carefully-don’t exceed 3,000 mg/day, especially if you have liver issues.
- Topical analgesics: Gels and patches like diclofenac gel (applied to skin) or lidocaine patches. They deliver pain relief locally with almost no systemic absorption.
- Physical therapy and heat/cold therapy: For chronic joint or muscle pain, these are effective, zero-risk options.
- Non-pharmacological pain management: Yoga, acupuncture, massage-these aren’t "alternative" anymore. They’re evidence-backed tools.
What If You Absolutely Need an NSAID?
Sometimes, the pain is too severe to avoid. If your doctor says you must use one, here’s the only safe path:- Use the lowest possible dose-for the shortest time possible. No more than 3-5 days.
- Avoid naproxen, meloxicam, and diclofenac. If you must use one, ibuprofen is the least risky.
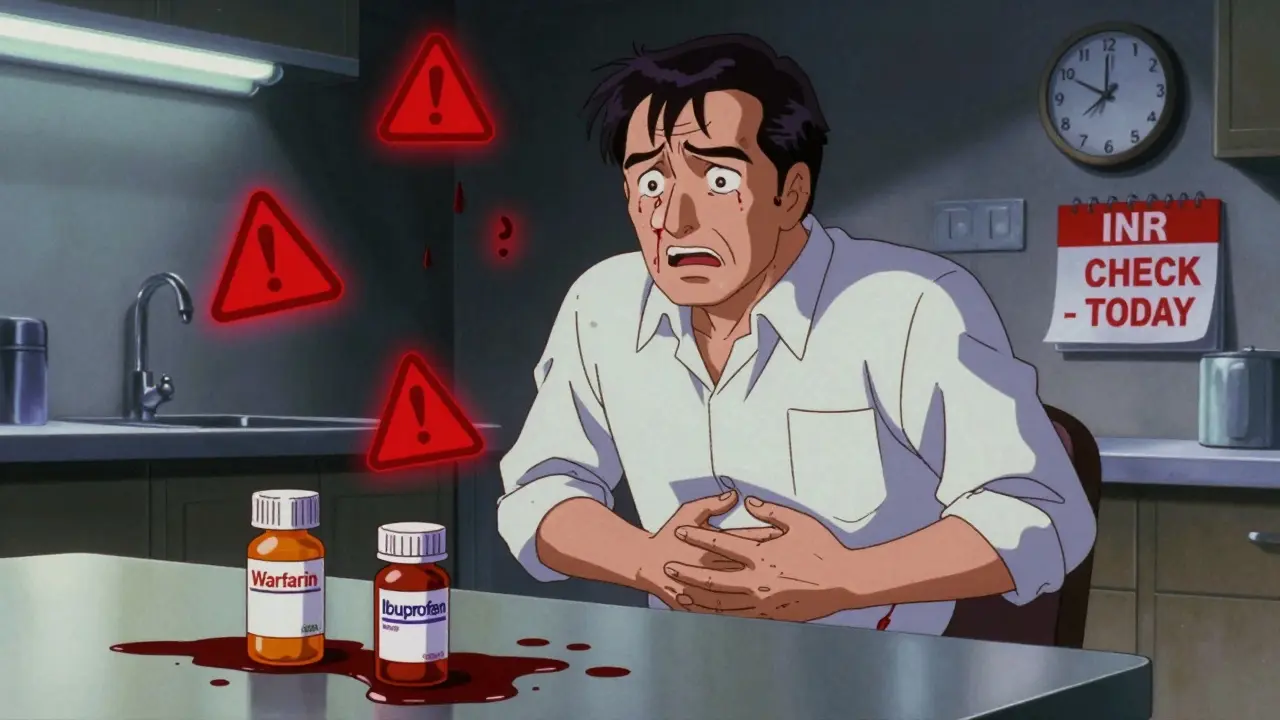
- Get your INR checked before starting the NSAID.
- Check it again 3 to 5 days after you start, then weekly until you stop.
- Take a proton pump inhibitor (PPI) like omeprazole at the same time. It doesn’t stop bleeding from platelet issues, but it protects your stomach lining.
- Tell your doctor every single time you take an NSAID-even if it’s "just once."
Why This Keeps Happening
You’d think this would be obvious. But it’s not. A 2021 University of Michigan study found that 68.2% of warfarin-related bleeding cases happened because patients didn’t tell their doctors they were taking OTC painkillers. They didn’t think it mattered. They were wrong. And electronic health records? In 41.7% of U.S. hospitals, they don’t even flag this interaction. If your doctor doesn’t know you’re taking ibuprofen, the system won’t warn them. Even the FDA’s warnings are buried. Warfarin guides have clear alerts. But most NSAID labels? They just say "risk of bleeding." No mention of warfarin. No specifics. That’s a gap in communication-and it’s costing lives.The Bottom Line
There’s no safe way to mix warfarin and NSAIDs. Not for a week. Not for a day. Not even for one pill. The risk is real, predictable, and preventable. If you’re on warfarin, treat NSAIDs like you would a loaded gun: keep them away. Use acetaminophen. Try a topical gel. Talk to your doctor about non-drug options. Your next INR test, your next ER visit, your next hospital stay-all of it can be avoided. This isn’t about being overly cautious. It’s about survival.Can I take ibuprofen with warfarin if I only use it once in a while?
No. Even a single dose of ibuprofen can raise your INR and increase bleeding risk. The interaction is immediate and unpredictable. There’s no safe threshold. If you need pain relief, use acetaminophen instead.
Is naproxen worse than ibuprofen with warfarin?
Yes, significantly. Naproxen carries a 4.1 times higher bleeding risk compared to warfarin alone, while ibuprofen raises the risk by 1.79 times. Naproxen also has a longer half-life, meaning it stays in your system longer and suppresses platelet function continuously. Avoid naproxen entirely if you’re on warfarin.
Do newer blood thinners like apixaban or rivaroxaban interact with NSAIDs the same way?
Yes. While NOACs like apixaban and rivaroxaban have fewer overall drug interactions than warfarin, they still significantly increase bleeding risk when combined with NSAIDs. Studies show similar rates of gastrointestinal and major bleeding with NSAID use across all oral anticoagulants. Don’t assume your newer blood thinner is safe with painkillers.
What should I do if I accidentally took an NSAID while on warfarin?
Call your anticoagulation provider or pharmacist immediately. Do not wait for symptoms. Get your INR checked within 3 days. Watch for signs of bleeding: unusual bruising, dark stools, blood in urine, severe headache, dizziness, or weakness. If any of these occur, go to the ER.
Are there any NSAIDs that are considered safe with warfarin?
No. All NSAIDs-whether over-the-counter or prescription-carry increased bleeding risk when taken with warfarin. Even topical NSAIDs like diclofenac gel can be absorbed into the bloodstream, though the risk is lower. The safest choice is to avoid all NSAIDs entirely and use acetaminophen or non-drug therapies instead.






13 Comments
Joshua Smith
Feb 9 2026Just wanted to say thanks for laying this out so clearly. I’ve been on warfarin for five years now and never realized how sneaky NSAIDs could be. I used to grab ibuprofen like it was candy for back pain. Now I keep Tylenol in every room. Simple switch, huge difference.
PAUL MCQUEEN
Feb 10 2026Wow. So we’re supposed to just suffer through chronic pain because Big Pharma doesn’t want us to know the truth? Or maybe the real issue is that doctors don’t educate patients properly. Either way, this feels like fearmongering with data.
Camille Hall
Feb 11 2026As someone who’s helped manage my mom’s anticoagulation therapy for years, this is spot on. She used to swear by naproxen for her arthritis-until she ended up in the ER with a GI bleed. We switched to topical diclofenac gel and heat packs. No more hospital trips. No more panic. It’s not glamorous, but it works.
Ashlyn Ellison
Feb 13 2026My cousin took one ibuprofen for a headache. Three days later, she was bleeding internally. No warning. No symptoms until she passed out in the kitchen. She’s lucky to be alive. Don’t be like her.
Tricia O'Sullivan
Feb 14 2026While the data presented is compelling and aligns with current clinical guidelines, I must emphasize the importance of individualized patient care. Some individuals may have no alternative but to utilize NSAIDs transiently under close supervision. The risk-benefit calculus must be weighed with precision, not replaced by blanket avoidance.
Lyle Whyatt
Feb 14 2026Let me tell you, I’ve been on warfarin since my pulmonary embolism in 2018. I used to laugh at people who said ‘don’t take Advil.’ Then I saw a guy in the pharmacy aisle-mid-50s, wearing a ‘I ❤️ NSAIDs’ shirt-buying a 100-count bottle of naproxen. I wanted to scream. I didn’t. But I did send him a DM. He never replied. I hope he’s still breathing.
Susan Kwan
Feb 16 2026Oh great. So now we’re supposed to believe that every single OTC painkiller is a death sentence? What’s next? ‘Don’t breathe too hard-might cause a clot!’ This is why people stop trusting medical advice.
Random Guy
Feb 17 2026so like… if i take one ibuprofen like once a year… like for a migraine once every 5 years… am i gonna die?? like… just one? come on. this post is giving me anxiety. i just want to feel better. not get a blood transfusion.
Ryan Vargas
Feb 17 2026Consider the architecture of systemic risk. The pharmaceutical industry, reliant on recurring revenue, has engineered a landscape where chronic pain is commodified and anticoagulants are treated as binary variables. The FDA’s failure to mandate explicit warfarin-NSAID warnings on OTC labels is not negligence-it’s structural. We are living in a system that prioritizes profit over precaution, and this post is merely a symptom of a deeper pathology: the erosion of patient autonomy under corporate medical hegemony.
Tasha Lake
Feb 18 2026From a pharmacokinetic standpoint, the interaction isn’t just additive-it’s synergistic. Warfarin’s CYP2C9 metabolism can be inhibited by NSAIDs, leading to elevated INR even without direct platelet dysfunction. And let’s not forget the renal effects: NSAIDs reduce glomerular filtration, which can cause warfarin accumulation. It’s a triple threat: platelet inhibition, metabolic interference, and reduced clearance. This isn’t anecdotal-it’s mechanistic.
Sam Dickison
Feb 19 2026My pharmacist flagged me the second I asked about ibuprofen. She said, ‘You’re on warfarin? That’s like putting a match next to a gas leak.’ I thought she was being dramatic. Then I saw the INR chart from my last test-jumped from 2.1 to 4.8 in 48 hours after one Advil. I haven’t touched NSAIDs since. Best decision I ever made.
Brett Pouser
Feb 20 2026I’m from the South-we don’t talk about our pain. We just grit our teeth. But after my uncle had a brain bleed from mixing warfarin and Motrin, my whole family changed. Now we all use ice packs, stretch, and pop Tylenol like it’s M&Ms. It’s not sexy, but it keeps us alive. Sometimes the simplest things are the most powerful.
Karianne Jackson
Feb 22 2026One ibuprofen. That’s all I took. One. And now I’m scared to even sneeze.