Lithium Toxicity: Signs, Risks, and What to Do If You Suspect It
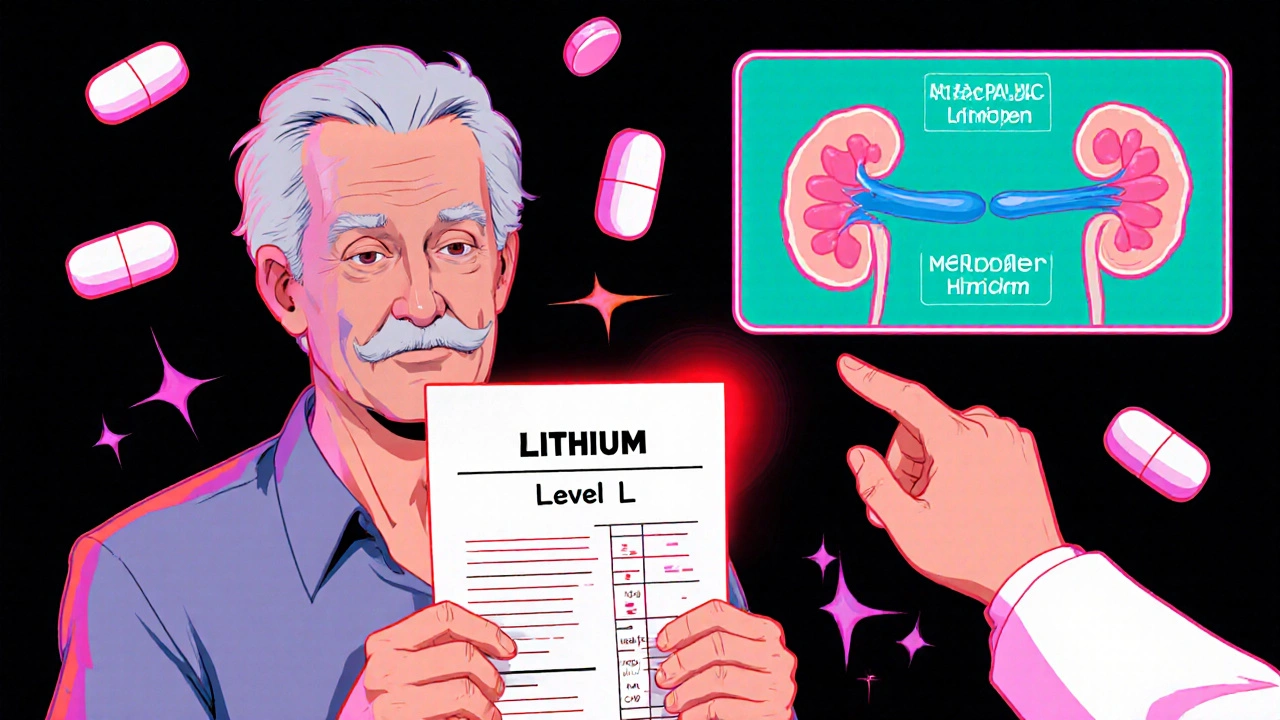
When you take lithium, a mood-stabilizing drug used primarily for bipolar disorder. Also known as lithium carbonate, it helps control extreme mood swings—but it doesn’t take much for it to turn harmful. Lithium toxicity happens when the level in your blood climbs too high, even slightly. Unlike many drugs, lithium has a very narrow window between helping and harming you. A normal blood level is between 0.6 and 1.2 mmol/L. Go just a little above that, and you could start feeling sick—really sick.
What causes lithium to build up? It’s not usually about taking too many pills. More often, it’s your body not flushing it out like it should. Kidney problems, dehydration, low salt intake, or mixing lithium with common drugs like ibuprofen, ACE inhibitors, or diuretics can all trap lithium in your system. Older adults are especially at risk because kidneys slow down with age. Even a mild illness like the flu or a stomach bug can throw your levels off if you’re not drinking enough water. You might not realize what’s happening until you’re already in trouble.
Early signs of lithium toxicity are easy to miss: shaky hands, nausea, or feeling more tired than usual. But if it gets worse, you could start vomiting, having trouble walking, slurring your words, or even experiencing confusion or seizures. These aren’t just side effects—they’re red flags that your body can’t handle the lithium anymore. If you’re on lithium and notice any of these, don’t wait. Call your doctor or go to the ER. Blood tests can confirm the level, and treatment often means stopping the drug, giving fluids, and sometimes using dialysis.
It’s not just about the drug itself. lithium blood levels, the key measure doctors use to monitor safety. Also known as serum lithium concentration, it’s checked regularly—especially when you first start, after a dose change, or if you get sick. You need these tests. Skipping them is like driving without a speedometer. And bipolar disorder medication, a category that includes lithium as one of the oldest and most studied options. Also known as mood stabilizers, they require careful management because the line between benefit and harm is thin. That’s why so many posts here focus on safe prescribing, drug interactions, and monitoring—because safety isn’t optional.
There’s no magic fix for lithium toxicity other than awareness and prevention. Stay hydrated. Don’t cut salt without talking to your doctor. Keep a list of every medicine and supplement you take. Tell every new provider you’re on lithium. And if something feels off—trust that feeling. The posts below cover real cases, common mistakes, and how to spot trouble before it becomes an emergency. You’ll find advice on what to do when symptoms show up, how to avoid dangerous drug combos, and why some people need more frequent testing than others. This isn’t theoretical. It’s life-saving information, written by people who’ve seen what happens when lithium goes wrong—and how to stop it before it’s too late.