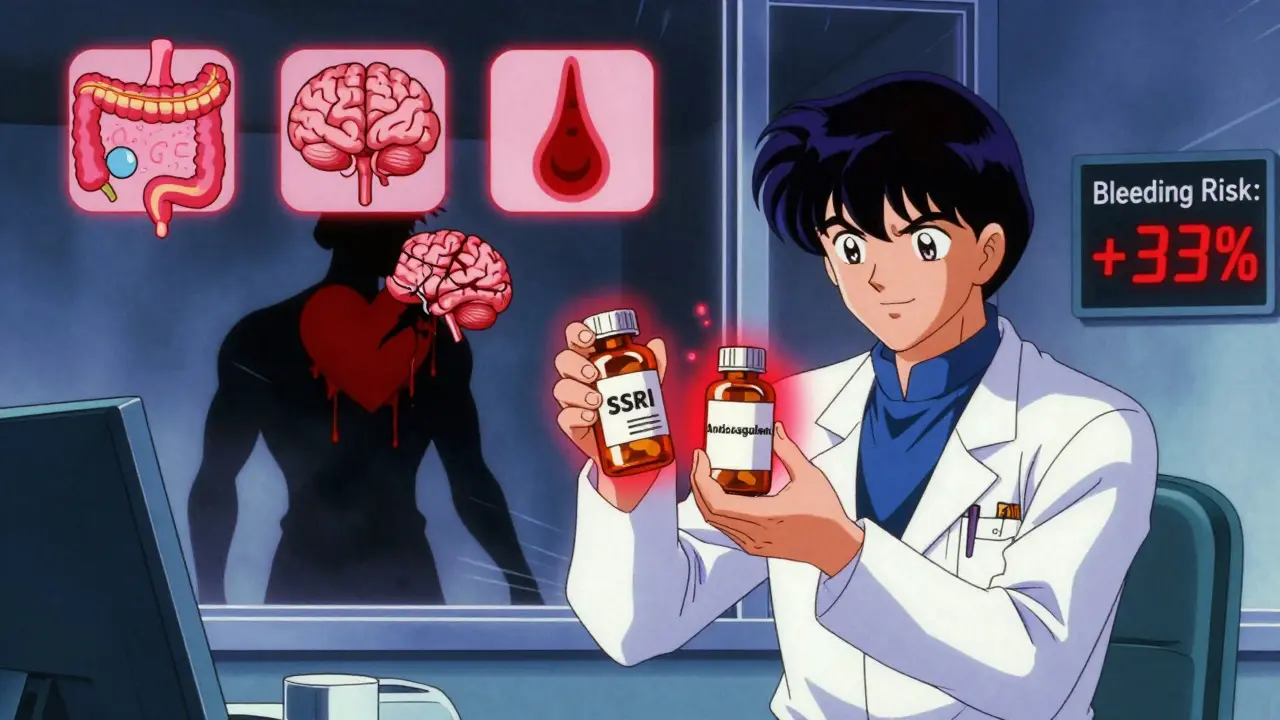
SSRI and Anticoagulant Bleeding Risk Calculator
Your Bleeding Risk Assessment
This tool estimates your risk of major bleeding when taking both an SSRI and an anticoagulant medication. Based on recent studies, combining these medications increases bleeding risk by up to 33% compared to anticoagulants alone.
Results
Your risk level indicates you should maintain regular monitoring and follow your doctor's recommendations. If you have additional risk factors, discuss alternative antidepressants with your physician.
When you’re taking an SSRI for depression or anxiety and also need an anticoagulant for atrial fibrillation or a blood clot, you might assume both medications are safe together. But here’s the reality: combining them increases your risk of serious bleeding - and it’s not just a theoretical concern. A major 2024 study of over 42,000 patients found that people taking both types of drugs had a 33% higher risk of major bleeding than those on anticoagulants alone. That’s not rare. It’s common enough that doctors now track it closely.
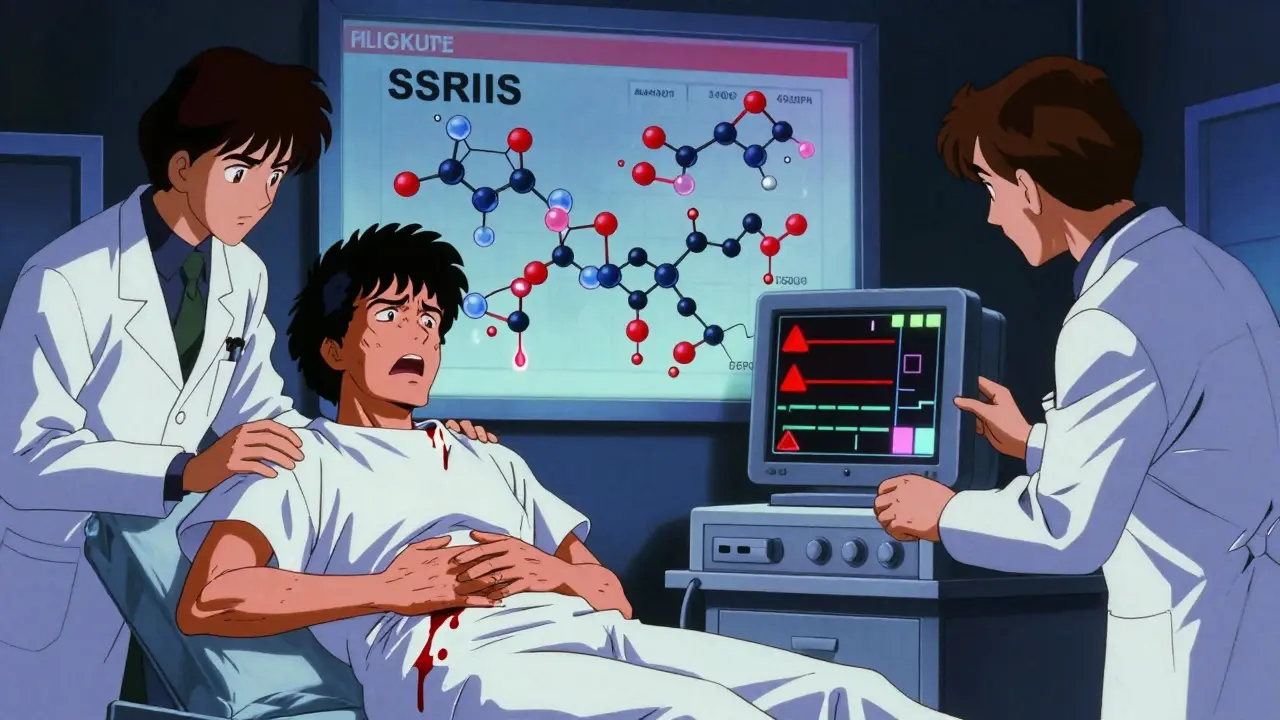
Why This Interaction Happens
SSRIs - like sertraline, escitalopram, and fluoxetine - work by boosting serotonin in the brain. But serotonin isn’t just a mood chemical. It’s also stored inside platelets, the blood cells that help clots form. When SSRIs block serotonin reuptake in the brain, they also block it in platelets. This depletes platelet serotonin by up to 90%. Without enough serotonin, platelets can’t stick together properly when you get a cut or bruise. The result? Slower clotting, longer bleeding.This isn’t about blood thinning like warfarin or apixaban does. It’s about platelets being less responsive. Think of it like having fewer workers on a construction crew trying to patch a hole. The hole still needs fixing, but the team can’t work as fast or efficiently.
Research from early 2025 confirmed this mechanism: SSRIs don’t mess with the actual clotting cascade - the proteins that form the final clot. Instead, they blunt the first step: platelet activation. That’s why bleeding happens even when INR levels are stable.
Where the Bleeding Happens
Not all bleeding is the same. The most common site? The stomach and intestines. About 58% of major bleeding events in patients taking both SSRIs and anticoagulants occur in the GI tract. That means black, tarry stools, vomiting blood, or sudden abdominal pain. These aren’t minor issues - they often require hospitalization.One in six cases involve bleeding in the brain. Intracranial hemorrhage is rare overall, but when it happens with this drug combo, it’s more likely to be fatal. Other bleeding sites include nosebleeds, bruising under the skin, and bleeding after minor injuries or dental work.
The numbers tell the story: while anticoagulants alone cause about 1.8 major bleeding events per 100 people each year, adding an SSRI bumps that to 2.4 events per 100 people. That’s 6 extra bleeding events for every 1,000 patients every year. For older adults or those with kidney disease, that risk climbs even higher.
Not All Anticoagulants Are Equal
If you’re on warfarin, your risk is higher than if you’re on a DOAC like apixaban, rivaroxaban, or dabigatran. The 2024 study showed warfarin plus SSRI had a 28% increased bleeding risk, while DOACs plus SSRI had a 22% increase. That difference sounds small, but in real-world terms, it means more hospital visits, more blood transfusions, and more time in the ER.Why? Warfarin is harder to control. Its effects swing with diet, other medications, and even how well your liver works. DOACs have more predictable levels. So if you’re on warfarin and your doctor adds an SSRI, you’ll need more frequent blood tests - sometimes twice a week in the first month.

Not All SSRIs Are the Same - But Not for the Reason You Think
You might assume that stronger SSRIs like paroxetine cause more bleeding than weaker ones like escitalopram. That’s logical, but it’s not what the data shows. The same 2024 study found no difference in bleeding risk between high-potency and low-potency SSRIs. Paroxetine, sertraline, fluoxetine, and escitalopram all carried the same 33% increased risk.This overturns older theories that suggested potency mattered. The key isn’t how strongly the drug binds to the serotonin transporter - it’s that all SSRIs do it enough to affect platelets. Even if one drug is slightly less potent, it’s still enough to cause trouble.
That’s why switching from one SSRI to another won’t fix the problem if you’re also on an anticoagulant. You need a different class of antidepressant entirely.
What to Do If You’re on Both
If you’re already taking an SSRI and your doctor prescribes an anticoagulant - or vice versa - don’t panic. But do take action.- Ask your doctor if you can switch to a non-SSRI antidepressant. Mirtazapine and bupropion don’t affect platelets and are often safer choices for people on blood thinners.
- Get baseline blood tests: CBC (complete blood count) and fecal occult blood test. These check for hidden bleeding.
- If you’re on warfarin, expect more frequent INR checks - especially in the first 30 days.
- Watch for signs of bleeding: unusual bruising, nosebleeds that won’t stop, dark stools, vomiting blood, sudden headaches or vision changes.
- Tell every doctor, dentist, and pharmacist you see that you’re on both medications. Many don’t ask.
According to a 2022 audit, nearly 7 out of 10 unsafe SSRI-anticoagulant combinations happen in primary care. That’s because depression and heart disease are both common - but few family doctors get formal training on how these drugs interact.
Who’s at Highest Risk?
Not everyone needs to avoid SSRIs. But if you have any of these, your risk jumps:- Age 75 or older
- History of stomach ulcers or GI bleeding
- Kidney or liver disease
- High HAS-BLED score (3 or higher - this measures bleeding risk in atrial fibrillation patients)
- Taking NSAIDs like ibuprofen or naproxen
- Alcohol use
If you have two or more of these, your doctor should strongly consider switching your antidepressant. The European Heart Rhythm Association recommends mirtazapine or bupropion in these cases.
What’s New in 2025
The FDA updated its anticoagulant medication guides in January 2025 to include clear warnings about SSRI interactions. For the first time, they recommend considering non-SSRI antidepressants in patients with additional bleeding risks.A major clinical trial called PRECISION-AF is currently underway. It’s tracking 5,000 patients on anticoagulants who are starting either an SSRI or a non-SSRI antidepressant. Results are due in late 2026 - and they could change guidelines again.
Meanwhile, the American College of Cardiology is developing digital tools that will help doctors pick the safest antidepressant based on your bleeding risk score, depression severity, and other medications. This isn’t science fiction - it’s coming to electronic health records soon.
Bottom Line
Combining SSRIs and anticoagulants isn’t forbidden. But it’s not risk-free. The bleeding risk is real, measurable, and preventable. If you’re on both, talk to your doctor about alternatives. Don’t stop your SSRI on your own - depression is dangerous too. But do ask: Is there a safer option for my heart and my brain?For many, switching to mirtazapine or bupropion means better sleep, fewer side effects, and less worry about bleeding. For others, careful monitoring and avoiding NSAIDs can make the combo safe enough to continue. The goal isn’t to avoid treatment - it’s to treat both conditions in the safest way possible.







10 Comments
Dominic Suyo
Dec 18 2025So let me get this straight - we’re telling people to swap SSRIs because platelets are ‘depleted’ of serotonin like some kind of broken vending machine? 🤦♂️ Meanwhile, the real issue is that we’re medicating depression with chemicals that were designed for lab rats and now we’re surprised when the human body throws a tantrum. The data’s solid, sure - but the medical mindset? Still stuck in the 90s. Just give me a pill that doesn’t make me bleed or cry.
Kevin Motta Top
Dec 18 2025Biggest takeaway: SSRIs aren’t the villain. The combo is. And doctors still treat this like a footnote, not a red flag. If you’re on a blood thinner, ask for bupropion or mirtazapine upfront. No drama. Just safer.
Marsha Jentzsch
Dec 19 2025OMG I’M ON BOTH AND I JUST HAD A NOSEBLEED THAT LASTED 20 MINUTES 😭 I THOUGHT IT WAS DRY AIR BUT NOW I’M SCARED TO DEATH!! WHY DIDN’T MY DOCTOR TELL ME THIS?!?!?!?!?!?!!? I’M SWITCHING TO MIRTAZAPINE TOMORROW NO MATTER WHAT!!
Carolyn Benson
Dec 20 2025It’s not about the drugs - it’s about the reductionist paradigm of modern psychiatry. We reduce complex emotional suffering to a serotonin deficit, then treat it with a blunt instrument that disrupts hemostasis. The body is not a biochemical vending machine. The brain is not a circuit board. And yet, we prescribe like engineers with a clipboard and zero reverence for the organism we’re tampering with. This bleeding risk? It’s not an adverse event - it’s a moral indictment.
Aadil Munshi
Dec 21 2025Bro, the fact that you think paroxetine is ‘stronger’ than escitalopram and therefore more dangerous? Classic. It’s not about potency - it’s about occupancy. All SSRIs hit that SERT receptor hard enough to drain platelet serotonin. Even the ‘mild’ ones. So no, switching SSRIs won’t help. You need a whole different class. Bupropion = dopamine/norepinephrine. Mirtazapine = histamine & serotonin antagonist. Neither touch platelets. Simple. Math. Science. No drama.
Danielle Stewart
Dec 22 2025If you’re on an anticoagulant and an SSRI, please don’t ignore the signs. Bruising easily? Dark stools? Headaches that feel ‘different’? These aren’t ‘just aging’ - they’re warnings. Talk to your doctor. Get a CBC. Ask about bupropion. You deserve to feel better - without fearing every little cut. You’re not alone in this. Many of us are navigating the same tightrope. Take care of yourself - and don’t be afraid to ask for safer options.
mary lizardo
Dec 23 2025The original post is meticulously referenced, statistically sound, and clinically nuanced - a rare gem in the sea of medical misinformation. Yet, the commentariat reduces it to emotional outbursts and oversimplified slogans. ‘Switch to bupropion!’ - as if it’s a one-size-fits-all solution. The reality? Comorbidities, pharmacokinetics, and individual pharmacodynamics require personalized assessment. This is not a meme. It’s pharmacology. And if you’re not engaging with the data, you’re not helping - you’re amplifying noise.
Adrienne Dagg
Dec 25 2025My grandma is on warfarin and sertraline… and she’s 82. She just started taking ibuprofen for her knees. 😳 I’m so glad I read this. I’m calling her doctor tomorrow. 🙏❤️ #DontLetYourGrandmaBleed
Glen Arreglo
Dec 27 2025Carolyn’s comment is poetic but dangerously misleading. The brain isn’t a ‘circuit board’ - but neither is it a mystical soul-container. SSRIs affect platelets because serotonin receptors are evolutionarily conserved. That’s not a moral failure - it’s biology. We don’t need to vilify science. We need to use it better. The real problem isn’t the drugs - it’s that primary care docs get 15 minutes with patients and zero pharmacology training. Fix the system, not the molecules.
shivam seo
Dec 29 2025Yeah right. All this data and you still think switching antidepressants is the answer? In Australia, we’ve been using bupropion for smoking cessation since the 90s - and it’s still not first-line for depression. SSRIs work. They’re cheap. They’re accessible. If you’re bleeding, maybe you’re just old, or you’re drinking too much, or you’re on NSAIDs. Don’t blame the SSRI. Blame the system that lets people take ibuprofen with warfarin. That’s the real killer.