More than one in three adults in the U.S. has metabolic syndrome - and many don’t even know it. It’s not a single disease. It’s a cluster of warning signs that quietly raise your risk for heart disease, stroke, and type 2 diabetes. The three most telling signs? Your waist size, your triglyceride levels, and how well your body handles glucose. These aren’t random numbers on a lab report. They’re connected. And understanding how they work together is the first step to turning things around.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t diagnosed by one test. It’s diagnosed when you have at least three out of five specific problems: a large waistline, high triglycerides, low HDL (good) cholesterol, high blood pressure, and elevated fasting blood sugar. The big three - waist size, triglycerides, and glucose - are the most visible drivers. They don’t happen by accident. They’re symptoms of something deeper: insulin resistance.
Insulin is your body’s key for moving glucose from your blood into your cells for energy. When your cells stop responding well to insulin, your pancreas pumps out more to compensate. Over time, it can’t keep up. Blood sugar rises. Fat builds up. Triglycerides climb. And your waistline expands - especially around your belly. This isn’t just about looking bigger. It’s about fat tissue becoming inflamed and toxic.
Why Waist Size Matters More Than Weight
Two people can weigh the same but have very different health risks. The difference? Where the fat is stored. Belly fat - also called visceral fat - is metabolically active. It doesn’t just sit there. It releases chemicals that interfere with insulin signaling, increase inflammation, and push your liver to make more fat and sugar.
The cutoffs aren’t arbitrary. For men, a waist size over 40 inches (102 cm) raises risk. For women, it’s over 35 inches (88 cm). But these numbers aren’t the same for everyone. South Asian, East Asian, and Indigenous populations often develop metabolic problems at much smaller waist sizes - as low as 31.5 inches (80 cm) for women. That’s why global guidelines now adjust thresholds by ethnicity. If you’re carrying extra weight around your middle, even if your BMI is normal, you’re at higher risk.
Every extra 4 inches (10 cm) around your waist increases your chance of heart disease by about 10%, even after accounting for overall weight. That’s not a small bump. That’s a red flag.
Triglycerides: The Hidden Lipid Threat
Triglycerides are the most common type of fat in your blood. When you eat more calories than your body needs - especially from sugar and refined carbs - your liver turns the excess into triglycerides and stores them in fat cells. But when insulin resistance kicks in, your liver doesn’t stop. It keeps churning them out.
The threshold for high triglycerides is 150 mg/dL. But here’s the catch: levels above 200 mg/dL are a major red flag for heart disease, even if your LDL (bad) cholesterol is normal. High triglycerides don’t just sit in your blood. They contribute to plaque buildup in your arteries. They also make your HDL cholesterol drop and your blood more prone to clotting.
What spikes triglycerides? Sugar. Alcohol. Refined grains. Fried foods. And sitting for long periods. A single sugary drink can send your triglycerides soaring within hours. Over time, that leads to fatty liver, which worsens insulin resistance and makes glucose control even harder.
Glucose Control: The Early Warning Sign
Fasting blood sugar of 100 mg/dL or higher is the diagnostic cutoff for impaired fasting glucose - a form of prediabetes. This isn’t diabetes yet. But it’s your body screaming that something’s wrong. At this stage, your cells aren’t taking up glucose efficiently. Your pancreas is working overtime. Your liver is dumping out extra sugar.
People with fasting glucose between 100-125 mg/dL have a 5-10% chance each year of developing full-blown type 2 diabetes. That’s higher than the risk for many other chronic conditions. And the worse your waist size and triglycerides are, the faster this progression happens.
The good news? This stage is reversible. The Diabetes Prevention Program showed that people who lost 5-7% of their body weight and got 150 minutes of walking per week cut their diabetes risk by 58%. That’s more effective than medication for most people. Lifestyle isn’t a backup plan - it’s the frontline treatment.
The Vicious Cycle: How These Three Feed Each Other
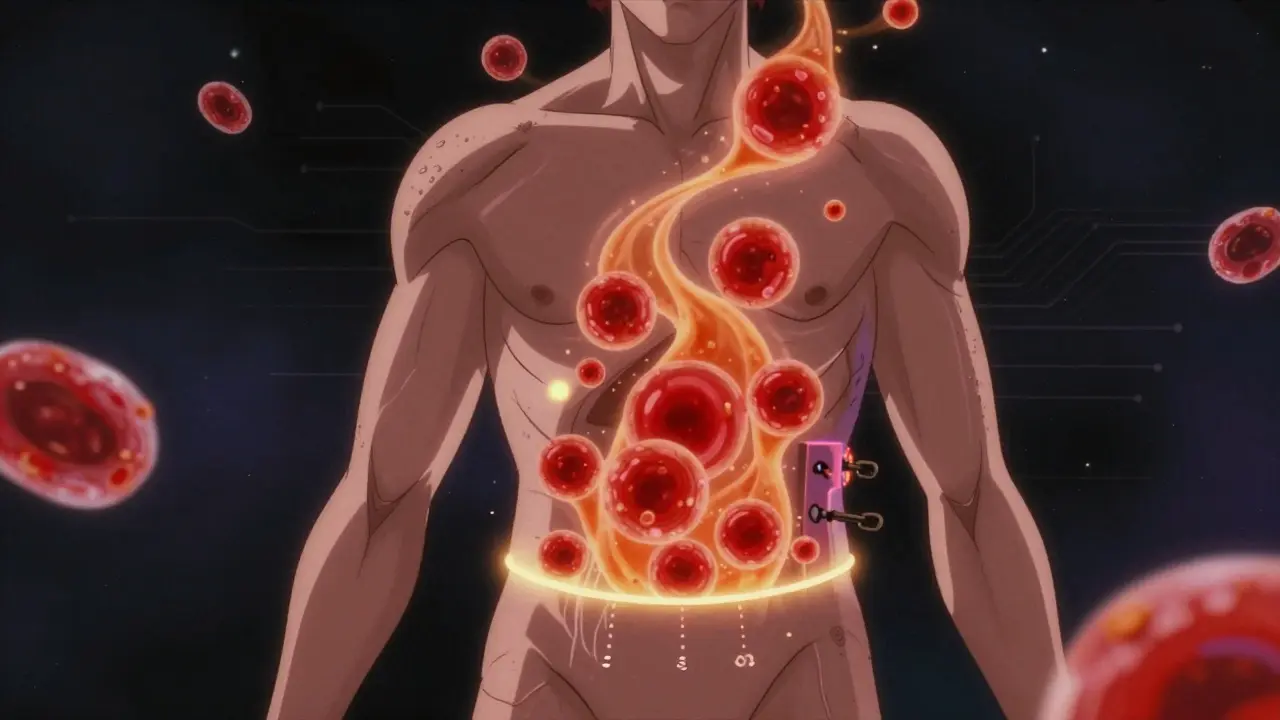
It’s not a coincidence that these three problems appear together. They feed each other in a loop:
- Excess belly fat releases inflammatory signals that block insulin receptors.
- Insulin resistance makes your liver produce more triglycerides and less HDL.
- High triglycerides spill over into muscle and liver cells, making them even more resistant to insulin (this is called lipotoxicity).
- Glucose stays high because muscles can’t absorb it, so your pancreas overworks.
- High blood sugar damages blood vessels and worsens fat storage, especially around the abdomen.
This cycle doesn’t stop unless you break it. Medications can help lower numbers, but they don’t fix the root cause. Only lifestyle changes can reverse insulin resistance.
How to Break the Cycle
You don’t need a miracle. You need consistency. Here’s what actually works:
- Move more, sit less. Aim for 150-300 minutes of brisk walking, cycling, or swimming per week. Even short walks after meals help lower blood sugar spikes.
- Cut added sugar. That includes sodas, sweetened coffee, pastries, and even "healthy" granola bars. The American Heart Association recommends less than 10% of daily calories from added sugar - ideally less than 5%.
- Choose whole foods. Focus on vegetables, legumes, whole grains, nuts, fish, and olive oil. The Mediterranean diet has been shown to reduce heart events by 30% in people with metabolic syndrome.
- Lose 5-10% of your body weight. That’s not about being thin. That’s about reducing visceral fat. For someone weighing 200 pounds, that’s 10-20 pounds. That alone can lower triglycerides by 20-50%, improve insulin sensitivity, and bring blood sugar down.
- Limit alcohol. One drink a day for women, two for men - but even that can raise triglycerides. For many, cutting alcohol completely is the fastest way to lower them.
Medications like metformin can help with glucose control. Fibrates or prescription omega-3s may be used for very high triglycerides. But none of these replace the need to reduce belly fat. Weight loss remains the most powerful tool - and the only one that can reverse all five components of metabolic syndrome.
What Comes Next?
Research is moving beyond just counting waist inches and lab numbers. Scientists are now looking at the triglyceride-glucose (TyG) index - a simple calculation using your fasting triglycerides and glucose levels. It’s a better predictor of insulin resistance than any single number. Some labs are starting to offer it.
Another emerging area? Gut bacteria. People with metabolic syndrome have different gut microbiomes than healthy people. Early studies suggest that changing your diet can shift these microbes in ways that improve insulin sensitivity - even before you lose weight.
But the bottom line hasn’t changed. If you have a large waist, high triglycerides, and elevated blood sugar, you’re not just "a little out of shape." You’re in the early stages of a preventable health crisis. The good news? You can reverse it. Not with a pill. Not with a quick fix. But with daily choices - food, movement, sleep, stress management - that slowly undo the damage.
Start small. Walk after dinner. Swap soda for sparkling water. Take the stairs. These aren’t grand gestures. But they add up. And they’re the only thing that truly works.
Can metabolic syndrome be reversed?
Yes - and many people do. Losing just 5-10% of body weight, cutting added sugar, and getting regular physical activity can reverse insulin resistance, lower triglycerides, improve glucose control, and shrink waist size. Studies show that lifestyle changes can reduce the risk of type 2 diabetes by over 50% and lower cardiovascular risk significantly. It’s not easy, but it’s possible.
Is a large waist size always a sign of metabolic syndrome?
Not always, but it’s the strongest predictor. You can have a large waist without having all five diagnostic criteria - but you’re still at higher risk for heart disease and diabetes. Waist size is the first red flag. If your waist is over 40 inches (men) or 35 inches (women), you should get your triglycerides, blood pressure, and fasting glucose checked - even if you feel fine.
Can I have metabolic syndrome and still be "normal weight"?
Yes. This is called "normal-weight obesity" or "metabolically obese normal weight." People with a normal BMI but high belly fat, high triglycerides, and insulin resistance are at the same risk as those who are overweight. Genetics, lack of muscle, and inactivity can cause fat to accumulate around organs even if overall weight is low. Waist size is a better indicator than BMI.
Do I need medication if I have metabolic syndrome?
Not necessarily. Lifestyle changes are the first and most effective treatment. Medications like metformin, statins, or blood pressure drugs may be added if your numbers are very high or if you already have heart disease. But drugs don’t fix insulin resistance. Only weight loss, better food, and movement do. Many people get off medication entirely after making lasting lifestyle changes.
How long does it take to see improvements?
You can see changes in as little as 2-4 weeks. Triglycerides often drop quickly with reduced sugar and alcohol. Blood sugar improves within days of eating fewer refined carbs. Waist size may take longer - but losing 1-2 pounds per week will shrink your waistline over time. The key is consistency. Even small, steady progress adds up.
What to Do Next
If you’re reading this and wondering if you might have metabolic syndrome, here’s what to do:
- Measure your waist - at the level of your belly button, after exhaling.
- Check your last lab results: triglycerides, HDL, fasting glucose, and blood pressure.
- If two or more are out of range, talk to your doctor. Don’t wait for symptoms.
- Start with one change: swap one sugary drink for water every day.
- Walk for 15 minutes after dinner - every day.
You don’t need to fix everything at once. But you do need to start. Because metabolic syndrome doesn’t get better on its own. It gets worse. And the earlier you act, the more you can save - your heart, your pancreas, your future health.





8 Comments
Lisa Davies
Dec 15 2025OMG I just measured my waist and I’m at 38 inches 😳 I thought I was fine because my BMI was normal… but now I’m scared. I’m swapping soda for sparkling water tomorrow and taking a walk after dinner. Small steps, right? 💪💧
Nupur Vimal
Dec 15 2025Everyone in India knows this already. We’ve been eating too much sugar and rice for decades. Our grandparents ate millet and lentils. Now we eat pizza and biryani every day. No wonder we’re getting diabetes at 30. Stop pretending this is a Western problem. It’s a global failure of food culture. And yes I’m talking to you Americans with your oat milk lattes.
RONALD Randolph
Dec 15 2025Let’s be clear: This isn’t about ‘lifestyle.’ It’s about personal responsibility. If you can’t control your intake of sugar and carbs, you’re not ‘sick’-you’re weak. And if you think walking after dinner fixes insulin resistance, you’re delusional. Real change requires discipline. Not ‘small steps.’ Not ‘sparkling water.’ Real, daily, unrelenting control. The science is clear. The willpower isn’t.
Benjamin Glover
Dec 17 2025How quaint. The American obsession with waist circumference as a proxy for health. In the UK, we’ve known since the 1980s that visceral fat is the real villain. But we don’t need a 2000-word essay to tell us that eating less sugar and moving more works. The answer has always been simple. It’s the execution that fails.
Melissa Taylor
Dec 19 2025I was diagnosed with prediabetes last year. I started walking after dinner, cut out candy, and swapped white bread for sourdough. Three months later, my fasting glucose dropped from 118 to 92. I didn’t lose 20 pounds-I lost 8. But my waist shrank by 3 inches. It’s not magic. It’s consistency. You can do this. I believe in you.
Mike Nordby
Dec 20 2025One thing missing from this post is the role of sleep deprivation and chronic stress in exacerbating insulin resistance. Cortisol directly promotes visceral fat accumulation and impairs glucose uptake. If you’re sleeping less than 6 hours or constantly under pressure, no amount of walking will fully counteract that. The biological cascade is real. Address sleep and stress alongside diet and movement.
John Samuel
Dec 20 2025Let me paint you a picture: Your belly fat isn’t just padding-it’s a tiny, angry, hormone-spewing factory. It’s whispering poison into your bloodstream every second. Triglycerides? That’s your liver screaming for mercy. Glucose? Your pancreas is running on fumes, crying in the corner. This isn’t a medical condition-it’s a full-blown biological mutiny. And the only general who can restore order? You. With a kale smoothie, a pair of sneakers, and a stubborn refusal to give up.
Sai Nguyen
Dec 22 2025Western medicine is broken. You think walking fixes it? In my village, we didn’t have gyms. We worked. We ate rice with bitter gourd. We didn’t need labs to know we were healthy. Now you people eat gluten-free junk and call it wellness. Pathetic.