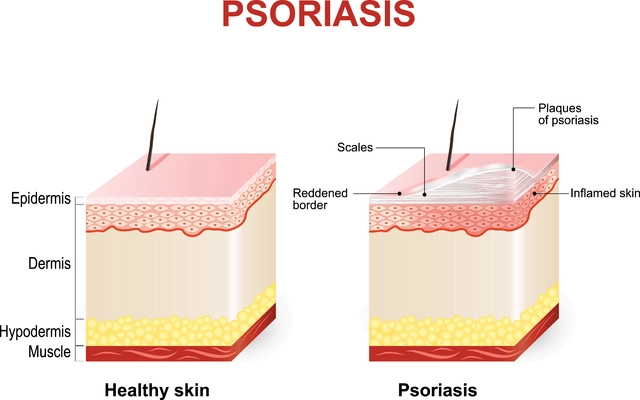
What Is Metabolic Acidosis in Chronic Kidney Disease?
When your kidneys can’t remove enough acid from your blood, your body becomes too acidic. This is called metabolic acidosis. In people with chronic kidney disease (CKD), this isn’t rare-it’s common. By stage 3, about 15% of patients have it. By stage 5, that number jumps to over 40%. The main sign? Low serum bicarbonate-below 22 mEq/L. Normal levels are 23 to 29 mEq/L. When bicarbonate drops, your body starts breaking down muscle to buffer the acid. Your bones weaken. Your heart works harder. And your kidneys decline faster.
It’s not just a lab number. It’s a signal your body is under stress. For years, doctors treated it as a side effect of CKD. Now, we know it’s a driver of progression. Correcting it isn’t optional-it’s part of slowing the disease.
Why Bicarbonate Matters
Bicarbonate is your blood’s natural buffer. It neutralizes acid so your pH stays around 7.35 to 7.45. In healthy kidneys, bicarbonate is regenerated and acid is excreted. In CKD, that system breaks down. The kidneys can’t make enough new bicarbonate, and acid builds up. That’s why treatment focuses on replacing what’s missing.
Oral sodium bicarbonate is the most common fix. A 650mg tablet gives you about 7.6 mEq of bicarbonate. Some patients take two or three a day. Studies show this can raise serum bicarbonate by 4 to 6 mEq/L in a few months. But it’s not just about fixing the number. The real win? Slowing kidney decline. One 3-year trial found patients on bicarbonate lost eGFR at a rate 5.9 mL/min/1.73m² slower than those on placebo. That’s the difference between reaching dialysis in 10 years versus 6.
Who Should Get Bicarbonate Therapy?
KDIGO guidelines say: start alkali therapy when serum bicarbonate falls below 22 mEq/L. That’s a Grade 1B recommendation-strong, based on solid evidence. But not everyone gets it. A 2023 analysis found only 43% of eligible CKD patients receive treatment. Why? Fear of side effects, lack of awareness, or just not testing bicarbonate regularly.
It’s not just for advanced CKD. Even in stage 3, if bicarbonate is low, treatment helps. The CRIC study showed patients with bicarbonate ≥22 mEq/L had a 23% lower risk of kidney failure or a 50% drop in eGFR. That’s why experts like Dr. L. Lee Hamm say correcting acidosis should be standard care for all CKD stages 3 to 5.
The Sodium Problem
Every 500mg sodium bicarbonate tablet contains 610mg of sodium. That’s a lot if you have high blood pressure, heart failure, or swelling. A 2020 study found CKD patients on sodium bicarbonate had a 32% higher risk of hospitalization for heart failure compared to those on calcium citrate.
This is why many nephrologists hesitate. They see the benefit but worry about the cost. The solution? Don’t skip treatment-choose wisely. If you’re fluid-sensitive, start low: one 650mg tablet daily. Monitor blood pressure and weight weekly. If your numbers climb, switch to a sodium-free option.

Alternatives to Sodium Bicarbonate
- Calcium citrate: Each 500mg tablet has 120mg of elemental calcium. It’s sodium-free and helps bone health. But too much can raise calcium levels and increase kidney stones. Limit to 1,000mg elemental calcium daily.
- Potassium citrate: Good for people with low potassium. But if your potassium is already above 4.5 mEq/L (common in CKD), this can push you into dangerous hyperkalemia. Studies show 22.4% of stage 4 patients on potassium citrate developed potassium levels over 5.0 mEq/L.
- Sodium citrate (Shohl’s solution): Liquid form, easier to dose. But it still has sodium. And many patients hate the taste-some mix it with orange juice, adding sugar they shouldn’t have.
- Dietary changes: Eat more fruits and vegetables. They’re base-producing. Apples, broccoli, spinach, and bananas reduce acid load. Meat, cheese, and processed grains are acid-forming. A diet with 5-9 servings of produce daily can cut acid load by 40-60 mEq/day. One patient in Cleveland Clinic raised bicarbonate by 3.5 mEq/L in six months just by swapping meat for beans and greens.
Why Veverimer Failed
For years, a drug called veverimer was the hope for sodium-free alkali therapy. It binds acid in the gut without being absorbed. Phase 2 trials looked great-bicarbonate rose by 4.3 mEq/L in 12 weeks. But the phase 3 trial in 2021 missed its goal. The difference vs. placebo was 2.07 mEq/L-statistically insignificant. The FDA didn’t approve it. The company plans to resubmit in 2024 with new data, but right now, it’s not an option.
This highlights a bigger problem: we need better drugs. But until then, we work with what we have.
Monitoring and Dosing
Don’t start high. Start low and go slow. Most nephrologists begin with 650mg sodium bicarbonate once or twice daily. Recheck serum bicarbonate in 4 to 6 weeks. Adjust dose by 650mg every 2 to 4 weeks until you hit 23-29 mEq/L. Once stable, test every 3 to 6 months.
Watch for side effects: bloating, nausea, swelling, or rising blood pressure. If you’re on calcium citrate, check serum calcium every 3 months. If potassium citrate is used, check potassium weekly at first. And always, always track your diet. Many patients don’t realize how much acid they’re eating.
The Real Barrier: Adherence
A 2022 survey of 457 CKD patients found 68% struggled with pill burden-averaging 4.2 tablets a day. 41% hated the taste of liquid forms. 29% had stomach issues. That’s why many stop.
One patient on Reddit said he had to mix baking soda powder in orange juice just to swallow it. Another said her legs cramped after switching to calcium citrate. These aren’t just complaints-they’re reasons treatment fails.
The best solution? Combine therapy with support. Work with a renal dietitian. Learn which foods help and which hurt. Use a PRAL score calculator (Potential Renal Acid Load) to track your daily acid intake. Target: below 0 mEq/day. Only 35% of patients hit that, even with counseling.
What’s Next?
The COMET-CKD trial, enrolling 1,200 patients, is testing high-dose vs. low-dose bicarbonate. Results come in late 2025. Early data on a new citrate-free alkali supplement (TRC001) shows promise-better tolerance, similar bicarbonate boost.
KDIGO’s 2024 draft update suggests lowering the treatment threshold from 23 to 22 mEq/L. Why? Because even 22 still protects the kidneys. And they’re pushing for personalized targets: 24-26 mEq/L for heart failure patients, 22-24 for elderly or malnourished ones.
But the biggest opportunity isn’t a new drug. It’s better screening. If every CKD patient had their bicarbonate checked every 6 months, we could prevent 28,000 cases of kidney failure a year in the U.S. alone. That’s $1.4 billion saved. All because we paid attention to a simple blood number.
Key Takeaways
- Metabolic acidosis is common in CKD stages 3-5 and speeds up kidney damage.
- Serum bicarbonate below 22 mEq/L should trigger treatment per KDIGO guidelines.
- Sodium bicarbonate works-but can worsen heart failure or high blood pressure.
- Calcium citrate and dietary changes are safer alternatives for sodium-sensitive patients.
- Potassium citrate is risky unless you have low potassium.
- Adherence is the biggest hurdle. Taste, pill burden, and side effects cause many to quit.
- Dietary acid load matters. Aim for 5-9 servings of fruits and vegetables daily.
- Regular monitoring every 3-6 months is essential for safe, effective treatment.



15 Comments
Matthew Peters
Nov 19 2025Man, I never realized how much acid our diets throw at us daily. I ate a burger and fries for lunch today and now I’m wondering if I’m slowly killing my kidneys without even knowing it. 🤯
Liam Strachan
Nov 20 2025Interesting read. I’ve always thought of CKD as just ‘kidneys wearing out,’ but this makes it clear it’s more like a chemical imbalance slowly eating away at the body. Good to see science catching up to what some of us have suspected.
Jeremy Samuel
Nov 21 2025so like… bicarb is just baking soda right? why are we makin’ this into a big pharma thing? just take a tsp in water. done. 🤷♂️
Ron and Gill Day
Nov 21 2025Another case of medical overcomplication. You want to fix acidosis? Stop eating processed junk. Stop drinking soda. Stop pretending you’re a ‘health-conscious’ person while chowing down on bacon and protein shakes. This isn’t rocket science-it’s basic nutrition.
Alyssa Torres
Nov 22 2025I’m a nurse who works with dialysis patients and I’ve seen this firsthand. One lady started on sodium bicarbonate and her energy shot up-she started gardening again. But then she got swollen ankles and had to switch. It’s not magic, but it’s a game-changer when done right. 🙌
Summer Joy
Nov 22 2025So let me get this straight… we’re giving people baking soda to fix a problem caused by… eating? 🤔 And nobody’s asking why the system is broken? This is just another way to make people dependent on pills while Big Food keeps selling you cheeseburgers. 😒
Aruna Urban Planner
Nov 23 2025The pathophysiological implications of chronic metabolic acidosis in CKD are profound. The compensatory mechanisms-muscle proteolysis, bone resorption, and reduced ammonia excretion-create a vicious cycle. Alkali therapy interrupts this cascade, but the sodium burden necessitates individualized risk-benefit stratification.
Nicole Ziegler
Nov 24 2025frfr i started eating more spinach and apples and my last bloodwork showed my bicarb went up by 2 points 😍 maybe diet really does work?? 🍎🥬
Bharat Alasandi
Nov 26 2025bro, i’m in stage 3 and i just started taking one bicarb tab a day. no more leg cramps, my BP is better, and i’m not feelin’ so wiped out all day. also swapped meat for dal and chana. best decision ever. 🙏
Kristi Bennardo
Nov 26 2025This is a dangerous precedent. We are medicalizing dietary habits and encouraging patients to rely on pharmaceuticals instead of taking personal responsibility. The FDA should be investigating the long-term effects of chronic alkali supplementation-not endorsing it.
Shiv Karan Singh
Nov 27 2025They say veverimer failed… but what if it was just suppressed? Big Pharma doesn’t want you taking cheap baking soda. 🤫
Ravi boy
Nov 27 2025so if i eat a banana every day and skip the chips i dont need pills? i mean… sounds too easy lol
Matthew Karrs
Nov 29 2025Who funds these studies? Who profits from prescribing bicarbonate? Why is no one talking about the real cause: glyphosate in our food? It’s not acidosis-it’s toxin overload. And they’re selling you a bandaid.
Russ Bergeman
Nov 30 2025Wait-so you’re telling me eating more vegetables can replace a pill? That’s… actually kind of amazing. I didn’t think diet could do that. I’m gonna try it. 🤞
Dana Oralkhan
Dec 2 2025To everyone saying ‘just eat more veggies’-yes, but not everyone can afford them. Or has time to cook. Or lives in a food desert. This isn’t just about willpower. It’s about access. We need better systems, not just more pills or more guilt.