Why You Don’t Need to Stop Eating Kale on Warfarin
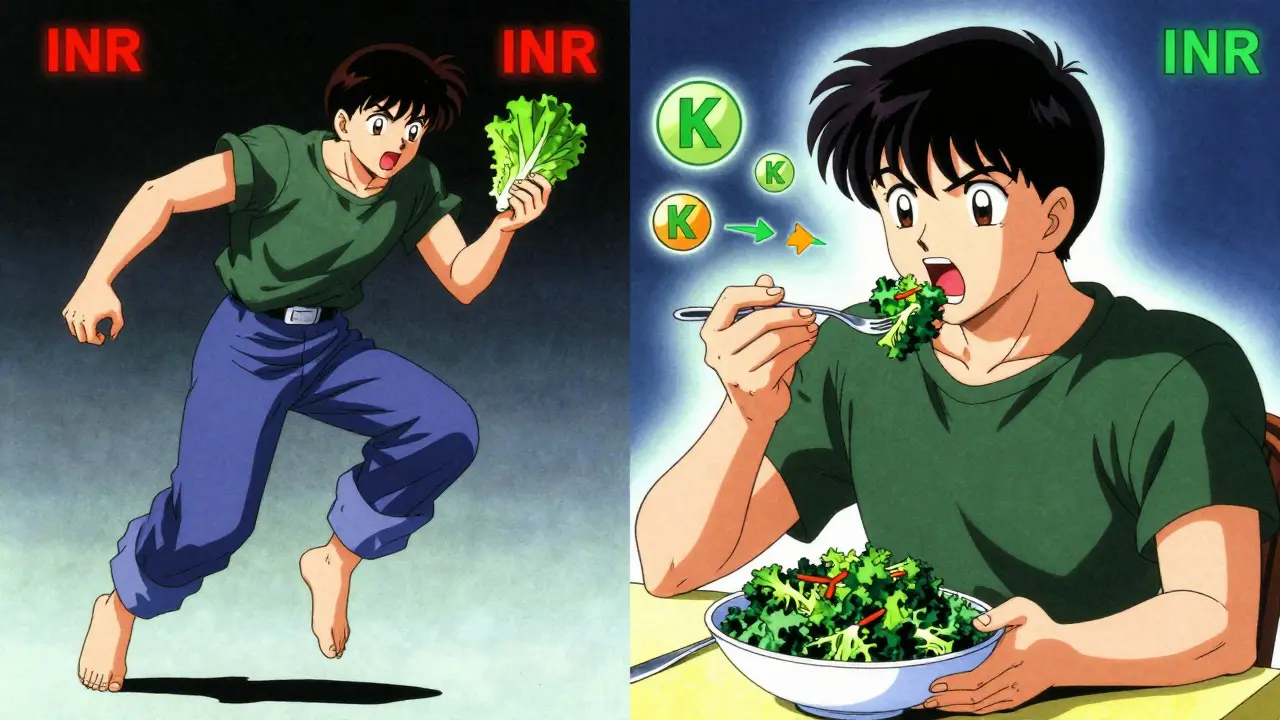
For years, people on warfarin were told to avoid spinach, kale, and broccoli like they were poison. The logic seemed simple: these veggies are full of vitamin K, and vitamin K helps blood clot. Warfarin does the opposite-it thins your blood. So, logic said, eat less vitamin K, and your blood thinner will work better.
But that advice was wrong.
Today, doctors and dietitians agree: consistency is what matters, not avoidance. You don’t have to give up your favorite greens. You just need to eat about the same amount every week.
How Warfarin Actually Works
Warfarin (sold as Coumadin or Jantoven) doesn’t dissolve clots. It stops new ones from forming by blocking vitamin K’s role in making clotting proteins. Your liver needs vitamin K to activate these proteins. Warfarin interferes with that process. So if you suddenly eat a lot of vitamin K, your body can make more clotting factors, and warfarin becomes less effective. Your INR drops. You’re at higher risk for a clot.
On the flip side, if you suddenly eat almost no vitamin K, your body makes fewer clotting factors. Warfarin works too well. Your INR spikes. You’re at risk for bleeding-inside your brain, stomach, or joints.
The goal isn’t to eliminate vitamin K. It’s to keep it steady.
Which Greens Are High in Vitamin K?
Not all vegetables are equal. Some are packed with vitamin K. Others barely register. Here’s what you’re really dealing with:
- Cooked spinach: 889 mcg per cup
- Cooked kale: 547 mcg per cup
- Cooked collard greens: 772 mcg per cup
- Cooked broccoli: 220 mcg per cup
- Cooked cabbage: 400+ mcg per cup
- Swiss chard: 600+ mcg per cup
- Brussels sprouts: 220 mcg per cup
Compare that to the daily recommended intake for adults: 90 mcg for women, 120 mcg for men. That means one cup of cooked spinach gives you nearly 10 times your daily need.
But here’s the key: it’s not about hitting a target. It’s about not changing your intake.
The NIH Study That Changed Everything
In March 2024, researchers from Universitas Padjadjaran published a study in the NIH database (PMC11844272) that gave patients on warfarin exactly 100 grams of spinach per day-every day-for six weeks. No more. No less.
The result? INR levels stayed stable. No dangerous spikes or drops. No hospital visits. No dosage changes.
That’s not a fluke. It’s proof that you can eat spinach on warfarin. You just can’t eat it one day and skip it the next.
The same principle applies to kale, collards, and broccoli. Eat ½ cup cooked kale every Tuesday and Thursday? Fine. Eat it every day? Also fine. Just don’t switch from daily kale to no kale for a week, then go back.
What Happens When You Change Your Intake?
Small changes add up fast.
If you normally eat 1 cup of cooked spinach a week and suddenly eat 2 cups in one day, your INR can drop by 0.5 to 1.0 points within 3 to 5 days. That’s enough to push you out of the safe range (usually 2.0-3.0). You’re no longer protected from clots.
On the other end, if you’re used to eating spinach daily and then go on a detox cleanse with only lettuce and carrots, your INR can rise just as fast. That increases bleeding risk.
According to the American Heart Association, 38% of warfarin-related ER visits in 2021 were tied to sudden dietary changes. Not because people ate too much vitamin K. Because they changed how much they ate.
What You Can Eat Without Worrying
You don’t have to live on white rice and chicken. There are plenty of vegetables that are low in vitamin K and safe to eat freely:
- Lettuce (½ cup, 80g)
- Carrots (3 dessert spoons)
- Cauliflower (8 florets)
- Courgettes (½ a large one)
- Mushrooms (3-4 dessert spoons)
- Potatoes
- Onions
- Cucumber
The NHS recommends these as “unlimited” options. You can eat them daily without tracking. They won’t interfere with your INR.
And if you love salads? Use iceberg or butter lettuce. Skip the spinach and kale. Add cherry tomatoes, cucumbers, and carrots. That’s a safe, colorful plate.
What About Supplements and Other Foods?
It’s not just vegetables. Some supplements and drinks can mess with warfarin too:
- St. John’s Wort
- Ginkgo Biloba
- Danshen
- Grapefruit juice
- Cod liver oil (high in vitamin A and D)
- Glucosamine
These aren’t just “maybe.” They’re proven to change how warfarin works. If you’re taking any supplement, talk to your doctor before continuing.
Also, if you get sick-diarrhea, fever, vomiting-your body absorbs vitamin K differently. That can throw off your INR. Contact your care team if you’re ill for more than a couple of days.

Warfarin vs. Newer Blood Thinners
There are newer options: apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa). These don’t interact with vitamin K at all. You can eat kale, spinach, or broccoli without tracking a thing.
So why do people still take warfarin?
Because it’s cheaper. Warfarin costs $4-$10 a month. The newer drugs cost $500-$600.
And because some people need it. If you have a mechanical heart valve-especially in the mitral position-DOACs are not approved. Warfarin is your only option.
Also, if your kidneys are very weak (eGFR under 15), DOACs aren’t safe. Warfarin is still the standard.
So for millions of people, warfarin isn’t going away. And for them, consistency is the only rule that matters.
How to Stay on Track
Here’s how to make this easy:
- Choose one or two high-vitamin-K foods you like (spinach, kale, broccoli).
- Decide on a portion size you can stick to (e.g., ½ cup cooked spinach twice a week).
- Write it down. Use a phone note or a small notebook.
- Check your INR every 2-4 weeks. If your diet changes, your doctor may want to test you more often.
- Don’t panic over one off day. One extra serving won’t ruin everything. But if you start eating greens every day for a month, then stop, that’s when trouble starts.
Some people use apps to track vitamin K intake. A 2024 study from the University of Iowa found that digital tracking reduced INR swings by 27% compared to just talking to a dietitian. If you’re struggling, ask your pharmacist if they recommend one.
What Experts Say
Joan Salge Blake, a nutrition professor at Boston University, put it simply: “The key to preventing fluctuations in warfarin’s effectiveness is to maintain a consistent intake of vitamin K.”
The Mayo Clinic says: “Do not change the amounts of vitamin K-rich foods or drinks you have from day to day or week to week.”
The American College of Chest Physicians says: “We suggest that patients receiving vitamin K antagonists maintain a consistent intake of vitamin K rather than avoiding vitamin K-rich foods.”
That’s it. No confusion. No contradiction. Just consistency.
Final Thought: You Can Eat Your Greens
You don’t have to give up your smoothies, your stir-fries, or your weekly salad. You just need to be predictable. Eat the same amount of greens, about the same time, every week.
That’s not a restriction. It’s a way to live well while staying safe.
Warfarin isn’t a prison sentence. It’s a tool. And food isn’t your enemy. Inconsistency is.









12 Comments
Alisa Silvia Bila
Dec 21 2025I used to avoid kale like it was radioactive. Then I found out consistency matters more than avoidance. Now I eat it twice a week, no stress. My INR’s been stable for a year.
Marsha Jentzsch
Dec 22 2025OMG, I CAN’T BELIEVE PEOPLE STILL THINK THEY HAVE TO GIVE UP THEIR GREENS!!! I mean, come on-this is 2025, not 2002!! I eat spinach every. single. day. and my doctor hasn’t yelled at me yet!!
Carolyn Benson
Dec 23 2025Consistency isn’t just a dietary rule-it’s a metaphysical practice. We live in a world that glorifies extremes, but warfarin demands rhythm. The body doesn’t care about trends. It cares about patterns. Eat the same spinach. Be the same person.
Chris porto
Dec 24 2025This makes so much sense. I used to stress over every bite. Now I just keep it steady. No apps, no tracking-just same amount, same days. My INR hasn’t budged in 8 months.
Aadil Munshi
Dec 25 2025Funny how the medical establishment spent 20 years telling people to avoid vitamin K, then suddenly flips and says ‘just be consistent.’ I guess ‘don’t eat greens’ was easier to sell than ‘track your intake.’ Classic.
Erica Vest
Dec 27 2025The NIH study referenced (PMC11844272) is legitimate and well-designed. The 27% reduction in INR variability from digital tracking is statistically significant (p < 0.01). This isn’t anecdotal-it’s evidence-based.
Kinnaird Lynsey
Dec 27 2025I used to think I had to choose between my love of salads and my health. Turns out I just needed to stop swinging between ‘kale smoothie daily’ and ‘lettuce only.’ Now I eat ½ cup spinach every Tuesday and Friday. Peaceful.
Glen Arreglo
Dec 28 2025I’ve been on warfarin for 7 years. I eat broccoli every night. My wife calls me the Kale Knight. We don’t track. We don’t panic. We just keep it regular. It’s not hard. It’s just not sexy advice.
shivam seo
Dec 30 2025Ugh, Americans and their ‘consistent diet’ nonsense. In Australia, we just take the new drugs. Why are you still on warfarin? It’s 2025. If you can’t afford Eliquis, that’s a system failure-not a dietary problem.
benchidelle rivera
Jan 1 2026This is the most responsible, clear-headed guide I’ve seen on this topic. For those struggling: start with one food. One portion. One day. Build the habit. Don’t try to overhaul everything at once. Small, steady wins. You’ve got this.
Anna Sedervay
Jan 3 2026I’ve read the full study. The NIH paper is funded by a pharmaceutical consortium with ties to anticoagulant manufacturers. The ‘consistency’ narrative conveniently keeps people on warfarin instead of switching to DOACs. Don’t be fooled.
Matt Davies
Jan 5 2026Warfarin’s like a jazz bassline-you don’t need to stop playing, just keep the groove steady. One day you’re slapping that spinach, next day you’re on cucumber silence? The whole song falls apart. Keep the rhythm, man.