Most sinus infections don’t need antibiotics - and using them too soon can hurt you
You wake up with a stuffy nose, facial pressure, and a headache. By day three, your snot is thick and green. You’re tempted to call your doctor for antibiotics. But here’s the truth: 9 out of 10 cases of sinusitis are caused by viruses - and antibiotics won’t touch them.
Every year, millions of people in the U.S. get antibiotics they don’t need for sinus infections. The Centers for Disease Control and Prevention says this overuse is one of the biggest drivers of antibiotic resistance. That means drugs that used to work might not work when you really need them - like if you get a serious infection later.
So how do you know if your sinus infection is viral or bacterial? And when, if ever, should you take antibiotics? Let’s cut through the noise.
What’s actually happening in your sinuses?
Sinusitis - or rhinosinusitis - means your nasal passages and the air-filled spaces around your nose (your sinuses) are swollen and inflamed. This can happen after a cold, allergies, or even a flu. The inflammation blocks drainage, traps mucus, and creates pressure that feels like a constant headache.
Most of the time, this is caused by a virus - the same ones that give you a runny nose and cough. Viral sinusitis makes up 90% to 98% of all acute cases, according to the American College of Allergy, Asthma, and Immunology. Bacterial sinusitis? That’s rare - only 2% to 10% of cases. Fungal infections are even rarer and usually only happen in people with weakened immune systems.
Here’s the catch: viral and bacterial sinusitis can feel almost identical in the first few days. That’s why so many people - and doctors - get confused. But there are clear patterns that tell them apart.
How to tell viral from bacterial sinusitis
It’s not about the color of your mucus. Yes, green or yellow discharge sounds like a bacterial infection - but that’s a myth. Viral infections can produce thick, discolored mucus too. The real clues are in timing and how your symptoms change.
Viruses: Symptoms start suddenly after a cold. You might have a low-grade fever, clear or cloudy mucus, mild facial pressure, and a stuffy nose. These symptoms usually peak around day 3 to 5 and then slowly get better. Most people feel normal again by day 7 to 10.
Bacteria: Two red flags stand out. First, symptoms last longer than 10 days without improving. Second, you get a double-worsening - you start feeling better after 5 to 7 days, then suddenly get worse again. That’s a classic sign your body couldn’t fight off the virus alone, and bacteria moved in.
Other signs of bacterial sinusitis include:
- High fever over 102°F (38.9°C) lasting more than 3 days
- Severe pain on one side of your face - especially under your eyes or around your cheeks
- Pain in your upper teeth (the roots sit right below your sinuses)
- Pus-like discharge that doesn’t clear up after 3 to 4 days
These aren’t just annoying - they’re signals your body needs help beyond rest and fluids.
When antibiotics are actually needed
Antibiotics are powerful - but they’re not magic. They only kill bacteria. If your infection is viral, they do nothing except increase your risk of side effects like diarrhea, rash, or even a dangerous gut infection called Clostridioides difficile (C. diff). C. diff can cause severe, life-threatening diarrhea, especially in older adults or people on other medications.
According to the Infectious Diseases Society of America and the American Academy of Otolaryngology, antibiotics should only be considered if:
- Symptoms last more than 10 days without improvement
- Or symptoms improve for a few days, then get much worse after day 5 to 7
- Or you have a high fever over 102°F with severe facial pain lasting more than 3 days
When antibiotics are needed, first-line treatment is usually amoxicillin - 500mg taken three times a day for 5 to 10 days. If you’ve had antibiotics recently, or live in an area with high rates of resistant bacteria, your doctor might prescribe amoxicillin-clavulanate (Augmentin) instead.
Some antibiotics you should avoid for sinusitis:
- Macrolides (like azithromycin or clarithromycin) - resistance rates are over 30%
- Trimethoprim-sulfamethoxazole (Bactrim) - resistance exceeds 40% in many areas
Why? Because these drugs have been overused for years. Bacteria have adapted. Using them now is like bringing a knife to a gunfight - it won’t work.
What to do instead - the real relief plan
For viral sinusitis - which is almost always the case - your best weapons are simple, cheap, and backed by science:
- Hydration: Drink at least 2 to 3 liters of water daily. Thinner mucus drains better.
- Saline nasal irrigation: Use a neti pot or nasal spray with sterile salt water 2 to 3 times a day. This flushes out mucus, allergens, and viruses. Studies show 75% of people master the technique after 3 to 5 tries with a video guide.
- Humidifiers: Keep indoor humidity between 40% and 60%. Dry air makes mucus thicker and harder to clear.
- Pain relief: Acetaminophen (650-1000mg every 6 hours) or ibuprofen (400-600mg every 6 hours) can ease pressure and headaches.
- Rest: Your immune system works better when you’re not running on empty.
These steps don’t just help you feel better - they speed up recovery. Most people feel significantly improved within 5 to 7 days without any drugs.
What doctors won’t always tell you
Many patients expect antibiotics because they’ve been prescribed them before. But research shows that’s often a mistake. A 2022 editorial in JAMA Otolaryngology found that 78% of antibiotics prescribed for sinusitis were unnecessary.
And here’s another surprise: CT scans and X-rays are rarely needed for routine sinusitis. A 2023 study found that 87% of healthy adults with no symptoms show sinus abnormalities on imaging. That means scans often show “problems” that aren’t causing anything - and lead to overtreatment.
Even the Cochrane Review, which analyzes hundreds of studies, found that antibiotics only help about 1 in 15 people with bacterial sinusitis. For every 10 people who get antibiotics, 1 to 2 will have side effects like diarrhea or nausea.
One patient on WebMD shared how she avoided seven rounds of antibiotics by sticking to saline rinses and nasal steroids for six months. Her symptoms vanished. Another patient on PatientsLikeMe developed C. diff after taking azithromycin for a viral infection - and ended up hospitalized.
Red flags: When to go to the doctor
Most sinus infections get better on their own. But some signs mean you need urgent care:
- Fever above 102°F lasting more than 3 days
- Swelling or redness around your eyes
- Blurred vision or double vision
- Severe headache that doesn’t improve with painkillers
- Stiff neck or confusion
- Difficulty breathing or high-pitched wheezing
These could mean the infection has spread to your eyes, brain, or lungs. Don’t wait.
The future of sinusitis care
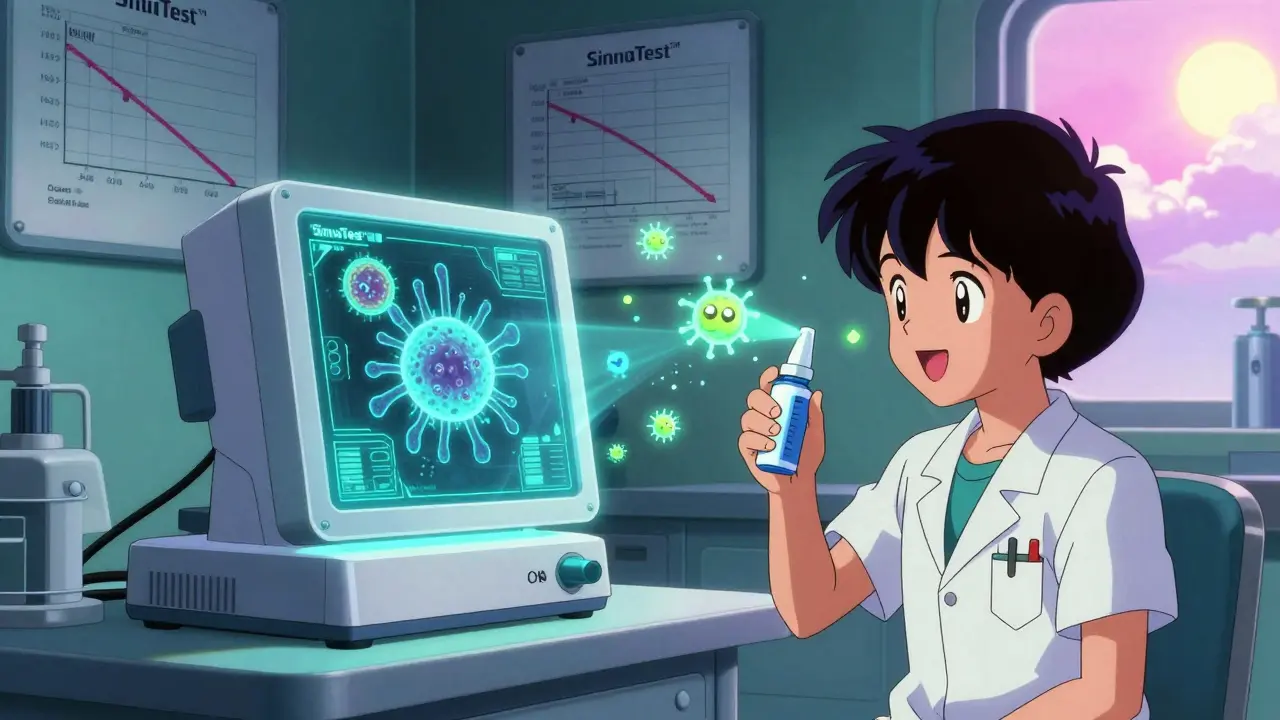
Science is moving fast. In May 2023, the FDA approved the first rapid test - SinuTest™ - that can detect common bacterial pathogens in minutes at the doctor’s office. It’s 89% accurate. Soon, doctors may be able to confirm bacterial infection before prescribing anything.
Researchers are also testing nasal probiotics - good bacteria sprayed into the nose - to prevent recurring infections. Early trials show a 42% drop in episodes compared to placebo.
And in the next few years, genetic tests might tell us who’s likely to respond to antibiotics - and who won’t. That could cut unnecessary prescriptions by half.
Bottom line: Don’t rush to antibiotics
Most sinus infections are viral. They’re uncomfortable, but they’ll pass. Antibiotics won’t help - and they might harm you in the long run.
Use saline rinses, stay hydrated, rest, and give it time. If symptoms last more than 10 days, get worse after improving, or come with a high fever and severe pain - then it’s time to talk to your doctor.
Being patient with your body isn’t weakness. It’s the smartest thing you can do - for yourself, and for everyone else.
Can green snot mean I have a bacterial sinus infection?
Not necessarily. Green or yellow mucus is common in viral infections too. It’s caused by your immune cells fighting the virus, not bacteria. The real signs of bacterial sinusitis are symptom duration (over 10 days), worsening after initial improvement, high fever, or severe one-sided facial pain.
How long should I wait before seeing a doctor for sinusitis?
Wait at least 10 days if your symptoms are slowly improving. If they get worse after day 5 to 7 - especially with new fever or increased pain - see a doctor. Also seek care immediately if you have vision changes, swelling around the eyes, severe headache, or a fever over 102°F lasting more than 3 days.
Are nasal sprays better than pills for sinusitis?
For inflammation, yes. Steroid nasal sprays (like fluticasone) reduce swelling and help drainage - and they’re safe for daily use. Oral decongestants (like pseudoephedrine) can help short-term but raise blood pressure and aren’t for everyone. Antibiotics are pills - and only useful if bacteria are confirmed.
Can I use a neti pot safely?
Yes - but only with distilled, sterile, or previously boiled (and cooled) water. Tap water can contain tiny organisms that cause rare but serious brain infections. Use a clean neti pot, rinse it after each use, and let it air dry. Most people get the technique right after 3 to 5 tries with a video tutorial.
Do children need antibiotics for sinusitis too?
Same rules apply. Most childhood sinus infections are viral. Antibiotics are only recommended if symptoms last over 10 days, worsen after improvement, or involve high fever and severe pain. The American Academy of Pediatrics strongly advises against early antibiotic use in kids due to side effects and resistance risks.
Why do doctors sometimes still prescribe antibiotics for viral sinusitis?
Pressure. Patients often expect them. Some doctors prescribe them to avoid follow-up visits or because they’re unsure. But guidelines from the CDC, American Academy of Family Physicians, and others clearly say: don’t prescribe antibiotics for symptoms under 10 days. Studies show that when doctors explain why antibiotics won’t help, patients accept it - and feel more satisfied with their care.