When a child has asthma, the difference between a normal day and an emergency visit often comes down to one small plastic tube: the spacer. It’s not flashy. It doesn’t have buttons or lights. But for millions of kids, it’s the quiet hero that keeps them breathing, in school, at play, and at home.
Why Spacers Are Non-Negotiable for Kids
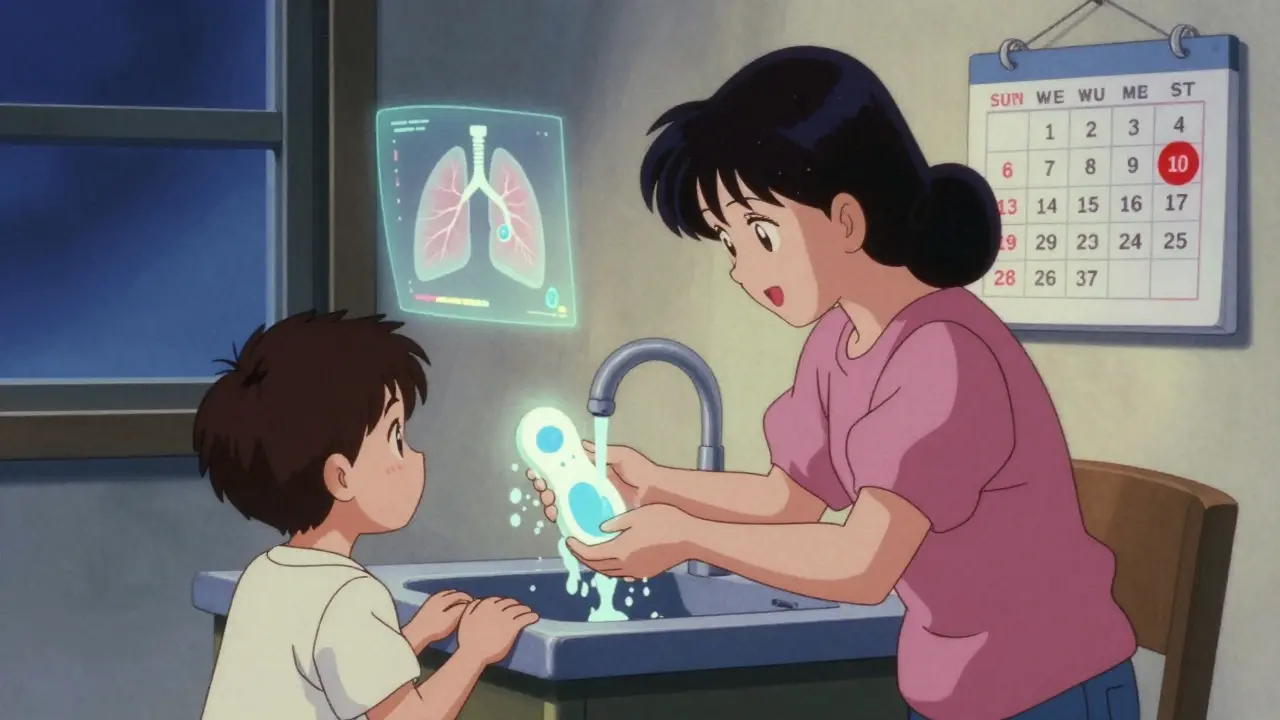
Metered-dose inhalers (MDIs) look simple - press and breathe. But for a 3-year-old, coordinating that press with a deep breath? Nearly impossible. That’s where spacers come in. They’re hollow tubes, usually made of plastic or anti-static material, that attach to the inhaler. When you press the inhaler, the medicine floats inside the spacer. The child then breathes in slowly, four or five times, and gets nearly all of the dose - not just a puff lost to the air or stuck in their throat. Studies show that without a spacer, less than 20% of the medicine reaches the lungs. With one, that jumps to over 70%. The Royal Children’s Hospital in Melbourne confirms that spacers are the gold standard for kids under five. The Global Initiative for Asthma (GINA) says the same: for preschoolers with wheezing, an MDI with a spacer is better than a nebulizer. It’s faster, cheaper, and just as effective. And the numbers back it up. A JAMA Pediatrics study found that kids using spacers had a 5% chance of being admitted to the hospital after an asthma flare-up. Those using nebulizers? 20%. That’s a four-fold difference. For families, that means fewer ER trips, fewer missed workdays, and less fear.How to Use a Spacer Correctly (No Guesswork)
It’s not enough to have a spacer. You have to use it right. Here’s the exact way to do it, step by step:- Have your child sit upright. No lying down.
- Attach the inhaler to the spacer. Make sure it’s snug.
- Hold the spacer and inhaler level - don’t tilt it up or down.
- Press the inhaler once. Just one puff.
- Ask your child to breathe in and out slowly through the mouthpiece (or mask) four times. Count to five each breath.
- Wait 30 seconds. If a second puff is needed, repeat the steps.
And here’s what most parents get wrong: they wipe the spacer dry after washing. Don’t. Static electricity traps the medicine. Instead, wash it once a week with mild dish soap and water. Let it air-dry - no towel, no rinsing. Just leave it alone until it’s dry. That’s it.
For kids under six, use a mask. For older kids, switch to a mouthpiece. But if your child is 10 or older and refuses the mask? That’s fine - just make sure they seal their lips tightly around the mouthpiece. Many teens don’t. And that’s why their technique fails.
The School Problem: Spacers Get Left Behind
Six million U.S. children have asthma. That’s one in every 12 kids. But in schools, the tools to manage it? Not always available. School nurses say the biggest issue isn’t lack of policy - it’s lack of access. Even though 42 states require schools to keep asthma meds on-site, many don’t have spacers. Rural schools are 45% less likely to have them than urban ones, according to the American Lung Association. And even when they do, they’re often stored in a locked cabinet, forgotten, or used only during emergencies. Then there’s the social hurdle. One 10-year-old told his mom, “I won’t take my spacer to school. Everyone stares.” He’s not alone. Teens especially hate standing out. They don’t want to be the kid with the plastic tube. So they skip it. Or they use the inhaler alone - and get less medicine, more side effects, more flare-ups. Schools that do it right? They train teachers, not just nurses. They keep spacers in the classroom, not just the nurse’s office. They make sure every child with asthma has a written care plan - and that it’s reviewed every term. One 2022 study found schools with full asthma policies cut absenteeism by 37%.
What a Real Asthma Care Plan Includes
A care plan isn’t a piece of paper. It’s a lifeline. The National Asthma Education and Prevention Program (NAEPP) says every child with asthma needs one. And it’s not just for the nurse - it’s for teachers, coaches, bus drivers, even the lunch lady. Here’s what a good plan must have:- The child’s name, birthdate, and emergency contacts
- Specific triggers: pollen, cold air, pets, exercise
- Medications: which ones, how often, and how to use them (with spacer instructions)
- Early warning signs: coughing, wheezing, tiredness, fast breathing
- What to do when symptoms start (green zone)
- What to do if it gets worse (yellow zone)
- When to call 911 or go to the ER (red zone)
- Signature of the child’s doctor and parent/guardian
Some schools use color-coded cards - green for “good,” yellow for “caution,” red for “emergency.” Simple. Clear. Fast.
And here’s the kicker: the plan must be reviewed every 6 to 12 months. Asthma changes. Kids grow. Their triggers shift. A plan from last year might not work now.
Why Technique Fails - And How to Fix It
The science is clear: spacers work. But only if used right. A 2022 study found that only 54% of kids aged 9-13 used their spacer correctly without a mask. With a mask? 89%. That gap tells you everything. The biggest mistakes?- Pressing the inhaler more than once
- Breathing in too fast
- Not holding the spacer level
- Wiping it dry after washing
- Using a wet spacer
And here’s what most parents don’t realize: if the spacer is wet, don’t use it. The medicine sticks to the water. The child gets nothing. Always keep a spare spacer at school - one for home, one for school. Wash them on the same day every week. Mark it on the calendar.
For teens? Make it normal. Let them choose their own spacer color. Let them pick a case that fits in their backpack. Some even come with fun designs - superheroes, animals, glow-in-the-dark. If it feels like theirs, they’ll carry it.
What’s Next: Tech, Training, and Better Access
The good news? Things are improving. In 2024, the American Academy of Pediatrics pushed schools to train teachers on spacer use - not just nurses. The CDC is funding spacer distribution in low-income districts. And researchers are testing smartphone apps that record how kids use their inhalers. One NIH-funded study, running through 2025, uses a tiny sensor on the spacer to track usage and give feedback. It’s not about fancy gadgets. It’s about making sure every child, no matter where they live or how much their family earns, has access to the same tools. Because asthma doesn’t care about zip codes. It only cares if the medicine gets to the lungs.Final Thought: It’s Not About the Device. It’s About the System.
A spacer won’t fix asthma. A care plan won’t cure it. But together - with trained staff, consistent use, and school support - they give kids back their childhood. They let them run, laugh, and breathe without fear. It’s not complicated. It’s not expensive. It just takes knowing how to use it - and making sure no child ever has to go without it.Do all children with asthma need a spacer?
Yes. Every child using a metered-dose inhaler (MDI) should use a spacer, no matter their age. Even toddlers benefit - the spacer makes sure the medicine reaches the lungs instead of staying in the mouth or throat. The American Academy of Pediatrics and Global Initiative for Asthma (GINA) both recommend spacers for all children using MDIs.
Can my child use a spacer at school?
Absolutely - and they should. In 42 U.S. states, schools are required to keep asthma medications, including spacers, on-site. But availability varies. Talk to your child’s school nurse and ask for a copy of their asthma policy. If they don’t have one, request it. A written plan with spacer access reduces emergency visits and absenteeism.
How often should I clean my child’s spacer?
Wash it once a week with warm water and a drop of dish soap. Don’t rinse it after washing - just let it air-dry. Rinsing creates static, which traps medicine. Never wipe it dry with a towel. If the spacer is wet and your child needs medicine, use the inhaler alone - a wet spacer won’t work.
Why does my teenager refuse to use the spacer at school?
Teens often feel self-conscious. Carrying a plastic tube makes them feel different. Try letting them pick a colorful case or a spacer with a design they like. Some brands make slim, compact spacers that fit in a pocket. Also, talk to the school nurse - can the spacer be kept in the classroom instead of the nurse’s office? Normalizing it helps.
Is a spacer better than a nebulizer for kids?
For mild to moderate asthma flare-ups, yes. Studies show spacers deliver more medicine to the lungs, work faster, and cost less than nebulizers. They’re just as effective - and kids can use them anywhere. Nebulizers are bulky, need electricity, and take 10-15 minutes. Spacers take 30 seconds. The American Academy of Pediatrics recommends spacers as the first choice for children.
What if my child’s school doesn’t have a care plan?
Ask for one. Every child with asthma should have a written, individualized asthma action plan signed by their doctor and parent. If the school says no, contact your local health department or the American Lung Association. Schools that ignore asthma plans risk legal liability and put children in danger. You have the right to request this.
Can a spacer be used with any inhaler?
Most standard metered-dose inhalers (MDIs) work with spacers. Check the inhaler packaging - it should say if it’s compatible. Spacer brands like AeroChamber, Volumatic, and NebuTech are widely used. Avoid cheap, no-name spacers - they may leak or build up static. Always use a spacer designed for your child’s inhaler.
How do I know if my child is using the spacer correctly?
Watch them. Do they press the inhaler once? Do they breathe in slowly for 4-5 breaths? Do they seal their lips around the mouthpiece? If they’re using a mask, is it snug on the face? Ask the school nurse or your child’s doctor to watch them use it. Many clinics offer free technique checks. Even one visit can fix years of bad habits.








8 Comments
Jay Ara
Dec 26 2025spacers are a game changer i wish i knew this when my nephew was little
Michael Bond
Dec 27 2025schools need to stop treating asthma like a paperwork problem. it's a health crisis.
Kuldipsinh Rathod
Dec 27 2025my cousin uses a spacer and no more hospital trips. simple stuff but so many parents dont get it
SHAKTI BHARDWAJ
Dec 27 2025why are we even talking about this like its new news? every kid with asthma needs a spacer its not rocket science
Matthew Ingersoll
Dec 29 2025in rural india we use spacers too. no fancy tech. just clean plastic and good technique. the science is universal.
carissa projo
Dec 30 2025it's not just about the spacer-it's about creating a world where a child doesn't have to hide their breath. where a 10-year-old doesn't feel like a medical anomaly for carrying a little plastic tube. where teachers know the difference between a cough and a crisis. where care plans aren't buried in filing cabinets but living, breathing documents in every classroom. this isn't healthcare-it's humanity.
josue robert figueroa salazar
Dec 30 2025spacers are useless if the kid doesnt use them right and no one checks. schools are just ticking boxes
david jackson
Dec 31 2025think about this: a child with asthma spends more time in school trying to avoid being seen as different than they do actually breathing properly. the spacer is the quietest revolution in pediatric medicine-no one talks about it because it’s not glamorous. no one films it on tiktok. no one gets a grant for it. but every time a kid takes a slow breath through that plastic tube, they’re reclaiming a piece of childhood that was stolen by bureaucracy, stigma, and ignorance. and yet, in 2025, we still treat this like a luxury. imagine if we gave every kid a color-coded, personalized spacer like we give them backpacks. imagine if every school nurse had a checklist, not just a drawer full of unused devices. imagine if we taught kids to use it like they learn to tie their shoes. this isn’t about medicine. it’s about dignity.