Drinking a glass of grapefruit juice in the morning might seem like a healthy habit-until it turns dangerous. For people taking certain medications, that refreshing citrus drink can cause serious, even life-threatening side effects. This isn’t a myth or a warning from an old wives’ tale. It’s a well-documented, scientifically proven interaction that affects more than 85 prescription drugs. And the worst part? Many people don’t even know they’re at risk.
How Grapefruit Juice Changes How Your Body Handles Medication
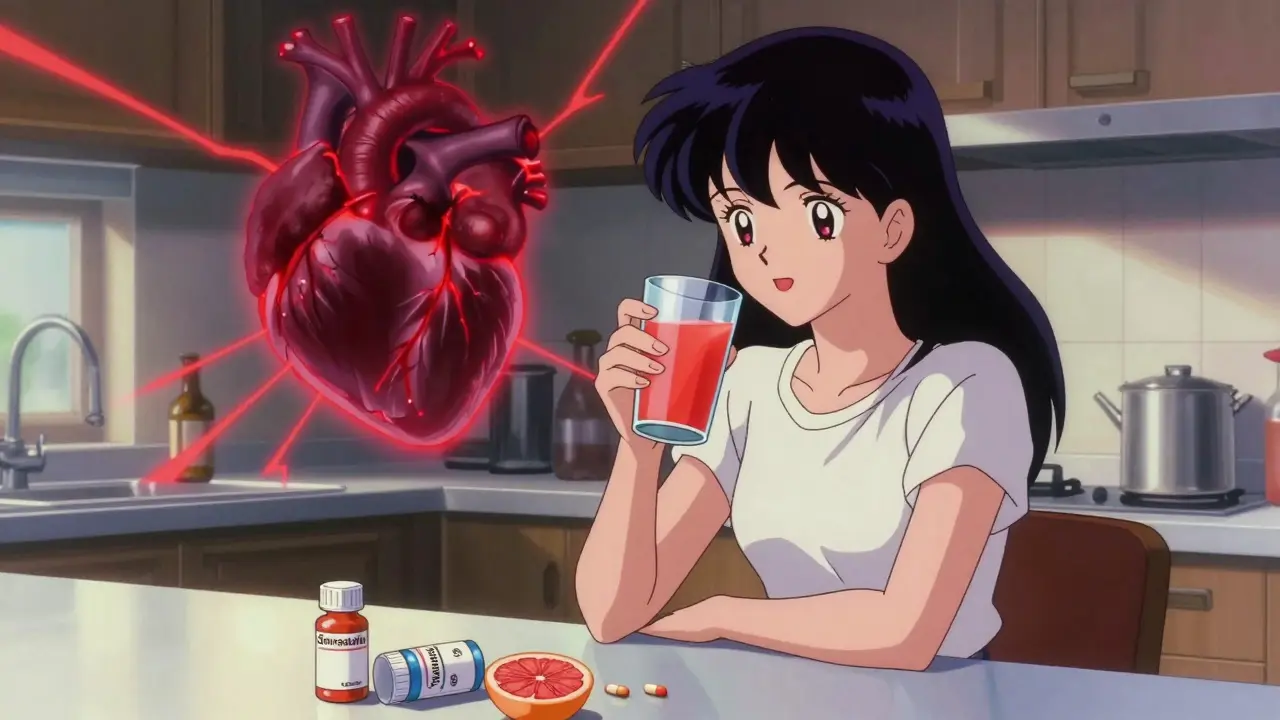
Grapefruit juice doesn’t just mix with your meds-it rewires how your body processes them. The culprit? Furanocoumarins, natural chemicals found in grapefruit, especially in the peel and pulp. These compounds shut down an enzyme in your small intestine called CYP3A4. This enzyme normally breaks down about half of all oral medications before they enter your bloodstream. When it’s blocked, your body absorbs way more of the drug than it should. The result? Drug levels in your blood can spike to dangerous levels. A single 200-milliliter glass (about 6.7 ounces) of fresh grapefruit juice can reduce CYP3A4 activity by nearly half within four hours. And the effect lasts up to 72 hours. That means even if you take your pill at night and drink juice in the morning, you’re still at risk. You can’t time your way out of this interaction. Unlike other food-drug interactions, grapefruit doesn’t just cause mild side effects. It can turn a safe dose into an overdose. For example, one study showed that a person taking felodipine-a blood pressure medication-had up to eight times more drug in their blood after drinking grapefruit juice compared to when they drank water. That’s not a small difference. That’s the difference between controlling your blood pressure and risking a heart attack or stroke.Medications That Can Become Dangerous with Grapefruit Juice
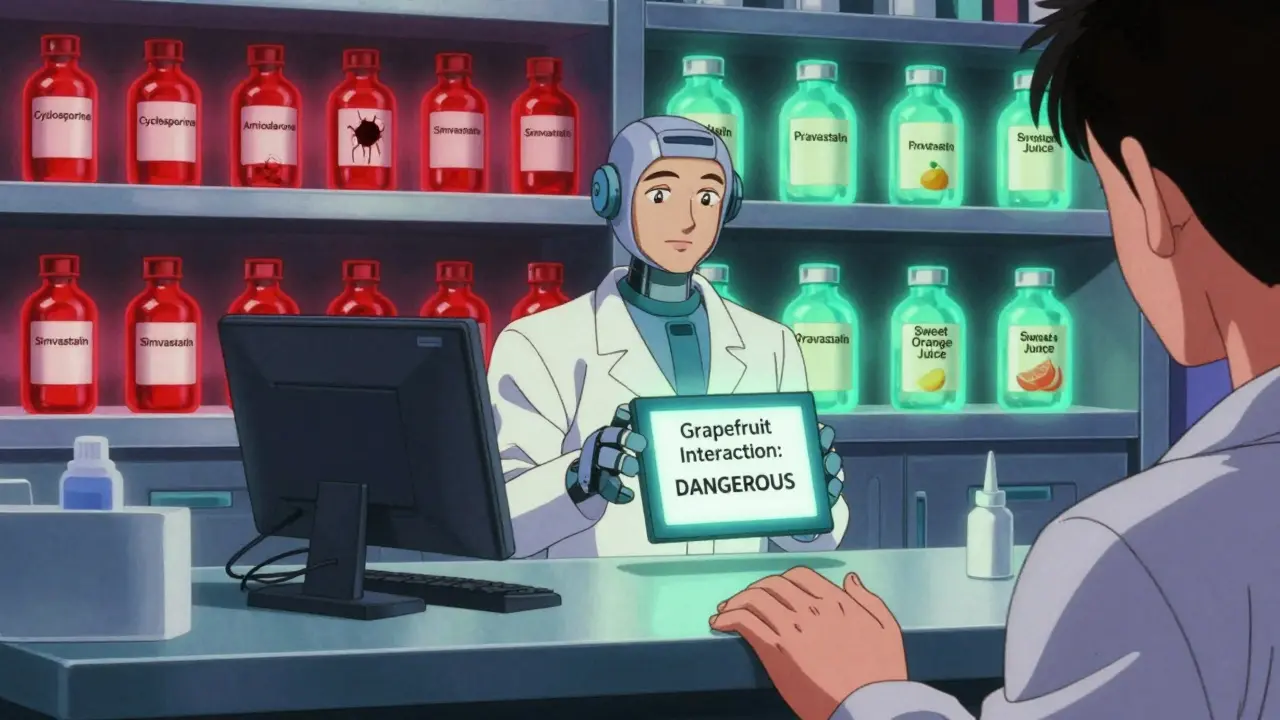
Not all drugs are affected the same way. Some are highly sensitive. Others barely react. Here are the most common and dangerous ones:- Statins (cholesterol drugs): Simvastatin (Zocor) is the most risky. Just one glass of grapefruit juice daily for three days can triple its levels in your blood, sharply increasing the chance of rhabdomyolysis-a condition where muscle tissue breaks down and can cause kidney failure. Atorvastatin (Lipitor) is less affected, but still risky. Pravastatin and rosuvastatin, however, are safe alternatives.
- Calcium channel blockers (blood pressure meds): Felodipine (Plendil) sees a five-fold increase in blood concentration. Nifedipine (Procardia) jumps by 3.3 times. But amlodipine (Norvasc) barely changes. If you’re on one of these, your doctor needs to know what you’re drinking.
- Immunosuppressants: Cyclosporine (Neoral), used after organ transplants, can increase by 50-60% with grapefruit. That raises the risk of kidney damage and other toxic effects.
- Antiarrhythmics: Amiodarone (Cordarone), used for irregular heartbeats, can spike in concentration by 30-40%, leading to dangerous heart rhythms.
- Some psychiatric drugs: Certain benzodiazepines and sedatives can become too strong. But others, like trazodone and zolpidem, show little to no interaction.
On the flip side, many common medications-including metformin, lisinopril, and most antidepressants-have no known interaction. That’s why guessing isn’t safe. You need to check your specific meds.
Why Some People Are More at Risk Than Others
Not everyone reacts the same way. Two people taking the same drug, drinking the same amount of juice, might have wildly different outcomes. Why? Because CYP3A4 enzyme levels vary from person to person. Some people naturally have more of it in their intestines. When grapefruit blocks it, their drug levels shoot up dramatically. Others have less to begin with, so the effect is smaller. Age matters too. People over 65 are more likely to be on multiple medications and consume grapefruit juice regularly. According to USDA data, older adults make up 40% of grapefruit juice drinkers in the U.S. And they’re also more likely to be taking drugs that interact with it. The American Geriatrics Society specifically warns this group to be extra careful. Even the type of grapefruit matters. White grapefruit has higher levels of furanocoumarins than red or pink. Fresh-squeezed juice is stronger than store-bought pasteurized versions. And even small amounts-like a splash in your water-can trigger the effect. There’s no safe threshold for high-risk drugs.What About Other Citrus Fruits?
Not all citrus is the same. Seville oranges (used in marmalade) and pomelos contain the same dangerous chemicals as grapefruit. So if you’re on a risky medication, avoid those too. Sweet oranges (like navel or Valencia), lemons, and limes? They’re generally safe. They don’t contain significant amounts of furanocoumarins. So if you’re looking for a citrus alternative, stick to these. The European Medicines Agency confirmed this in 2022. If you’re unsure, check the label. If it warns against grapefruit, assume it also applies to Seville oranges and pomelos.What Should You Do If You’re on Medication?
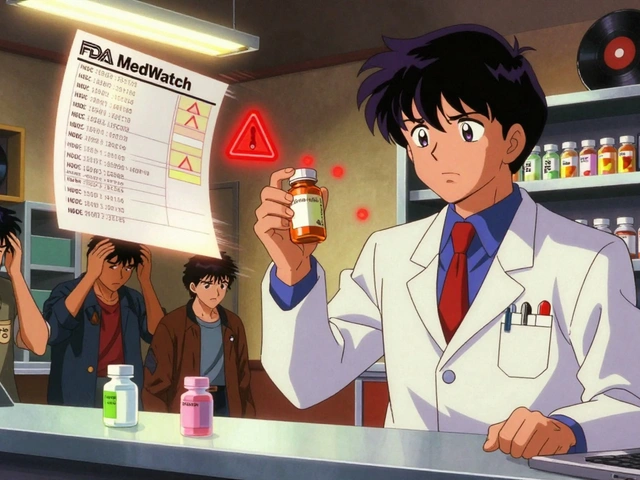
Don’t panic. But do act. Here’s what to do:- Check your medication labels. Since 2014, the FDA has required drug manufacturers to include grapefruit interaction warnings on labels. Look for phrases like “avoid grapefruit juice” or “do not consume grapefruit products.”
- Ask your pharmacist. Pharmacists are trained to catch these interactions. A 2021 study found that 89% of community pharmacists routinely screen for grapefruit-drug interactions when filling prescriptions.
- Keep a complete list of all your medications. This includes prescription drugs, over-the-counter pills, and supplements. Some herbal supplements, like St. John’s Wort, also interact with CYP3A4.
- Ask your doctor about alternatives. If you love grapefruit juice and are on simvastatin, ask if you can switch to pravastatin or rosuvastatin. If you’re on cyclosporine, tacrolimus might be a safer option.
- Don’t assume it’s safe just because you’ve been drinking it for years. The interaction doesn’t build up over time-it happens every time you drink it. Even if you’ve never had a problem before, the next glass could be the one that causes harm.
What’s Being Done to Fix This?
Scientists aren’t ignoring the problem. In October 2023, the USDA announced that CRISPR-edited grapefruit with 90% less furanocoumarin had passed early safety tests. If approved, these modified fruits could one day be sold as “safe for medication users.” Meanwhile, drug regulators are getting stricter. The FDA now requires all new oral drugs metabolized by CYP3A4 to be tested with grapefruit juice during development. The European Medicines Agency has similar rules. That means future medications will come with clearer warnings-or won’t be approved if they’re too risky. But until then, the safest advice remains: if your drug interacts with grapefruit, avoid it completely. Not just at dosing time. Not just in large amounts. Just avoid it entirely while you’re taking the medication.Why So Many People Still Don’t Know About This
It’s shocking, but true: only 38% of patients remember being told about grapefruit interactions when they were prescribed a risky drug, according to a 2022 survey by the National Community Pharmacists Association. That means over 6 in 10 people are drinking grapefruit juice without knowing they could be putting themselves in danger. Doctors are busy. Pharmacists are overwhelmed. Patients assume their meds are safe with food. But this isn’t a minor issue. It’s a preventable cause of hospitalizations, organ damage, and even death. The bottom line? If you’re on medication, don’t assume. Ask. Check. Confirm. Your body will thank you.Can I drink grapefruit juice if I take my medication at night and juice in the morning?
No. The enzyme-blocking effect of grapefruit juice lasts up to 72 hours. Even if you take your medication at night and drink juice in the morning, the enzyme is still inhibited. The interaction isn’t about timing-it’s about whether the enzyme is active when the drug is absorbed. Avoid grapefruit entirely while on affected medications.
Is it safe to eat grapefruit instead of drinking the juice?
No. The same furanocoumarins that block the enzyme are present in the fruit’s pulp and peel. Eating a whole grapefruit has the same effect as drinking the juice. The form doesn’t matter-only the chemical content.
What if I only drink a small amount of grapefruit juice?
Even a small amount-like a splash in your water or a spoonful of pulp-can inhibit CYP3A4. There’s no known safe threshold for high-risk drugs like simvastatin or felodipine. If your medication is on the list, avoid grapefruit completely.
Are there any medications that are safe with grapefruit juice?
Yes. Many common drugs don’t interact with grapefruit. These include metformin, lisinopril, levothyroxine, and most antibiotics. But you can’t assume yours is safe. Always check your specific drug’s label or ask your pharmacist. The only way to be sure is to verify.
Can I switch to orange juice instead?
Sweet oranges (navel, Valencia), lemons, and limes are safe alternatives. They don’t contain furanocoumarins. But avoid Seville oranges and pomelos-they have the same dangerous chemicals as grapefruit. Always check the type of citrus before drinking.



10 Comments
Vanessa Barber
Jan 23 2026Okay but what if you only drink it once a week? I’ve been doing it for 10 years with my statin and I’m fine. Maybe your body just adapts?
Kerry Evans
Jan 23 2026People like you are why this country is falling apart. You treat medical advice like a buffet. Grapefruit isn’t ‘maybe dangerous’-it’s a biochemical grenade. If you’re too lazy to read the label, don’t blame the doctor when your kidneys fail.
Kerry Moore
Jan 24 2026Thank you for this thorough and clinically accurate breakdown. The distinction between CYP3A4 inhibition and pharmacokinetic variability is often overlooked in public health messaging. The data on simvastatin versus rosuvastatin is particularly compelling and should be emphasized in patient counseling materials.
Janet King
Jan 25 2026If you take blood pressure meds or cholesterol pills, skip the grapefruit. It’s not complicated. Check your bottle. Ask your pharmacist. Do it now. Your heart will thank you later.
Stacy Thomes
Jan 27 2026STOP DRINKING GRAPEFRUIT JUICE IF YOU’RE ON MEDS!!! I SAID STOP. I KNOW A WOMAN WHO ENDED UP IN THE ICU BECAUSE SHE THOUGHT ‘A LITTLE WON’T HURT.’ SHE DIDN’T. SHE’S FINE NOW BUT SHE’S SCARED TO DEATH. DON’T BE THAT PERSON.
dana torgersen
Jan 28 2026you know… i’ve been thinking… like… the body is this… *wonderful*… system… right? and grapefruit… it’s not ‘bad’… it’s just… interacting… with our biology… like… a key in a lock… but the lock was never meant for that key… and we just… didn’t know… until now… and maybe… we’re all just… trying to survive… in a world that doesn’t tell us enough…
Dawson Taylor
Jan 29 2026The 72-hour window is the most important takeaway. Timing doesn’t matter. Absorption does. Simple.
Sallie Jane Barnes
Jan 31 2026For anyone reading this and feeling overwhelmed: you’re not alone. This is why pharmacists exist. Walk in, show them your pill bottle, and say ‘Is this safe with grapefruit?’ No shame. No rush. Just ask. You deserve to be safe.
Andrew Smirnykh
Jan 31 2026In my country, we don’t drink grapefruit juice often. But I’ve seen people here assume ‘natural’ means ‘safe.’ It doesn’t. Nature gives us toxins, too. This is a good reminder that biology doesn’t care about marketing.
Laura Rice
Feb 1 2026My grandma took simvastatin for 8 years and drank grapefruit juice every morning. She’s 82 and still walks 3 miles a day. Maybe it’s not as scary as they say? Just saying…