Every day, pharmacists hand out millions of generic drugs. They’re cheaper, widely used, and trusted. But what happens when a generic pill doesn’t work the same way as the brand-name version? What if a patient starts having strange side effects after switching? These aren’t rare guesses-they’re real problems, and pharmacists are often the first to notice them.
Why Pharmacists Are Key to Generic Drug Safety
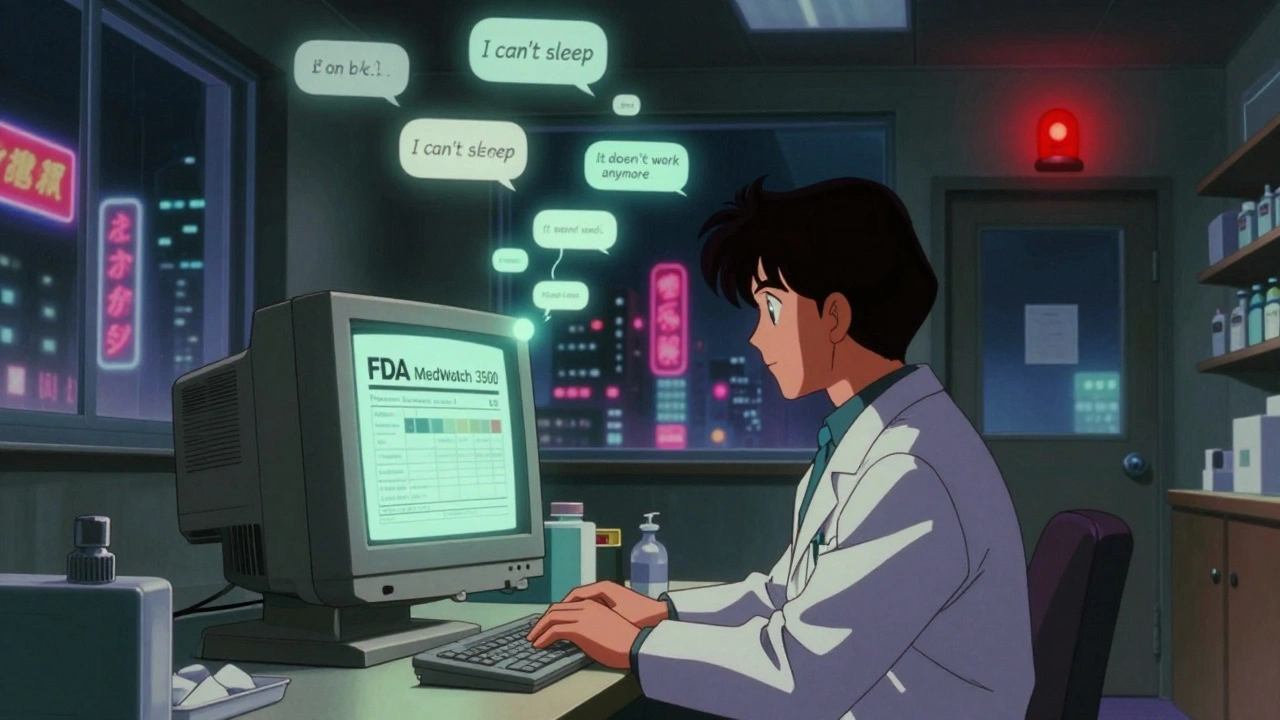
Pharmacists don’t just fill prescriptions. They see what happens after the patient leaves the pharmacy. They hear from patients who say, ‘This new pill makes me dizzy,’ or ‘I used to feel fine on this medication, now I can’t sleep.’ When a generic drug behaves differently than expected, it’s often the pharmacist who connects the dots.
The FDA calls this therapeutic inequivalence. It means a generic drug meets lab standards for bioequivalence but doesn’t perform the same in real life. Maybe the inactive ingredients cause an allergic reaction. Maybe the tablet breaks down too slowly in the stomach. Maybe the dose isn’t absorbed consistently. These aren’t manufacturing defects. They’re subtle differences that only someone who sees dozens of patients every day can spot.
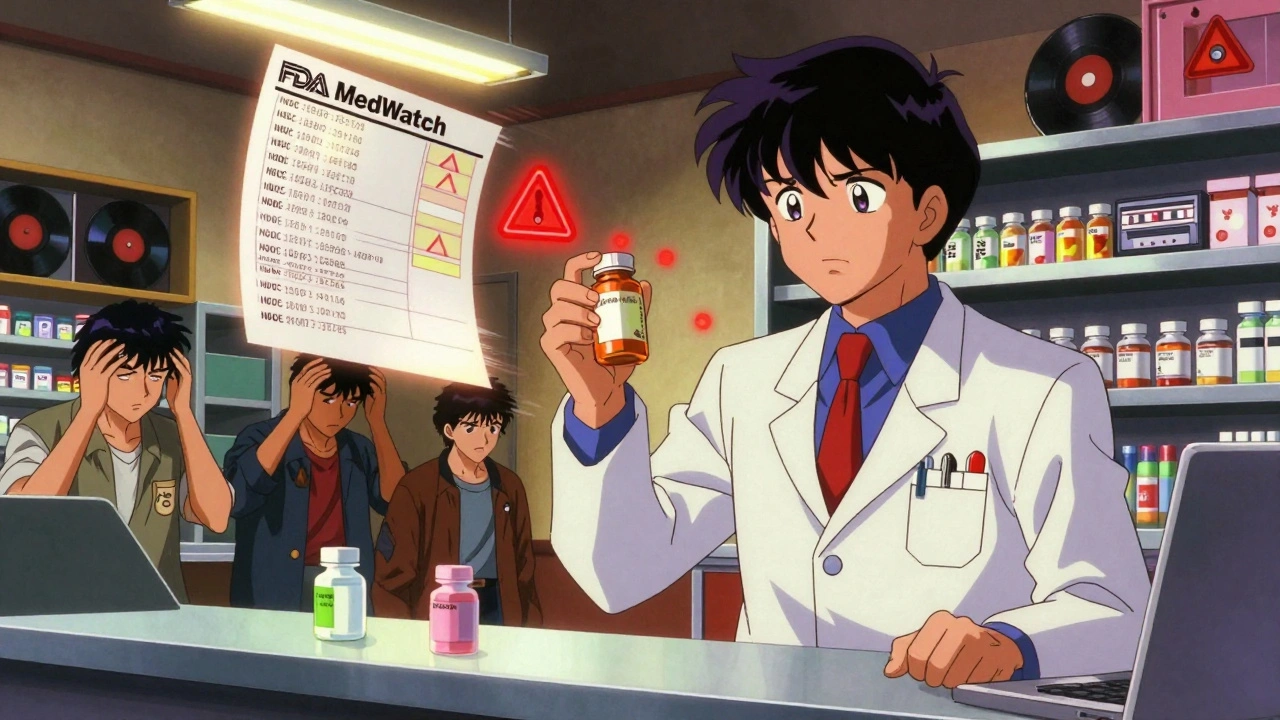
According to the FDA’s 2022 Annual Report, 1,842 reports of therapeutic inequivalence were submitted that year. Of those, 387-over 21%-came from pharmacists. That’s a big jump from just a year before. And yet, pharmacists still make up less than 3% of all adverse event reports to the FDA, even though they dispense 75% of all prescriptions in the U.S., and 90% of those are generics.
What Exactly Should You Report?
You don’t need to be 100% sure a drug caused the problem. The FDA says: if you suspect it, report it.
Here’s what counts as reportable:
- Severe side effects: hospitalization, life-threatening reactions, permanent disability
- Unexpected reactions: something not listed on the label
- Therapeutic failure: the drug just doesn’t work anymore after switching to generic
- Multiple patients with the same issue after a switch
- Problems with the pill’s appearance, taste, or how it dissolves
The FDA’s MedWatch Form 3500 (version 4.1, updated January 2023) asks for specific details: patient age and gender, the drug’s National Drug Code (NDC), the manufacturer name, the lot number, and a clear description of what happened. A report that just says ‘patient had side effects’ won’t help. But one that says ‘78-year-old male, switched from Brand-X to Generic-Y, developed severe tremors within 48 hours, symptoms resolved after switching back’? That’s gold.
And here’s something many pharmacists don’t realize: you can report even if you don’t know which brand or generic was originally prescribed. If you see a pattern-three patients in a week with the same issue after switching to the same generic-you can still flag it. The FDA’s Therapeutic Equivalence Working Group uses these patterns to trigger deeper reviews.
The Legal Reality: You’re Not Required to Report
Here’s the hard truth: federal law doesn’t force you to report generic drug problems. The FDA encourages it. Professional groups like ASHP and APhA say it’s part of your ethical duty. But there’s no federal penalty for not reporting.
That doesn’t mean you’re off the hook. Four states-California, Illinois, Massachusetts, and New York-have made reporting mandatory for serious adverse events. California’s Board of Pharmacy explicitly requires pharmacists to maintain a system for identifying and reporting therapeutic failures. If you practice in one of those states, you’re legally bound.
Even where it’s not required, your professional license is on the line. The American Society of Health-System Pharmacists says adverse event reporting is a fundamental professional responsibility. If a patient is harmed and you knew something was off but didn’t act, you could face disciplinary action from your state board.
Why So Few Pharmacists Report
Less than 3% of reports come from pharmacists. Why?
Time. 68.4% of pharmacists in a 2023 Pharmacy Times survey said they don’t report because they’re too busy. Filling prescriptions, counseling patients, managing inventory-it’s a nonstop grind.
Uncertainty. 52.1% don’t know if what they’re seeing is serious enough. Is it the drug? The patient’s other meds? Stress? Age? The line between coincidence and causation is blurry.
Attribution. 41.7% can’t tell if the problem came from the brand or the generic. And here’s the twist: generic manufacturers can’t update their labels independently. Thanks to the 2011 Supreme Court case PLIVA v. Mensing, they’re legally stuck with the brand’s label. That means if a patient has a bad reaction, the brand manufacturer often gets the report-even if they didn’t make the pill the patient took. The FDA’s data shows this creates a massive reporting gap. The real source of the problem gets buried.
And then there’s the lack of clear definitions. 54.2% of pharmacists in a 2023 ASHP survey said they don’t know what ‘therapeutic inequivalence’ actually looks like in practice. Is it a slight change in blood levels? A patient feeling ‘off’? The FDA’s 2022 guidance says: if the clinical response is different from what’s expected after a switch, report it. No need to prove bioequivalence failed in a lab-just document what you see.
How to Report: A Simple Step-by-Step Guide
You don’t need to be a regulatory expert. Here’s how to do it in under 10 minutes:
- Go to www.fda.gov/medwatch and download Form 3500 (or use the online portal).
- Check the box: ‘Generic Drug Concern.’ Then choose: Therapeutic Inequivalence, Manufacturing Quality, or Labeling Issue.
- Fill in the patient’s age, gender, and any relevant medical history (no names needed).
- Enter the NDC, manufacturer name, and lot number from the bottle.
- Describe the event clearly: ‘Patient switched from Brand-X to Generic-Y on 10/15/2025. Developed severe nausea and dizziness within 24 hours. Symptoms resolved after switching back to Brand-X on 10/18/2025.’
- Submit. Done.
The FDA now has a dedicated online portal with a ‘generic drug’ filter. You can even upload a photo of the pill if it looks different. And if you’re unsure? Call the FDA’s MedWatch hotline at 1-800-FDA-1088. They’ll walk you through it.
What Happens After You Report?
Every report goes into the FDA’s FAERS database-over 25 million reports as of December 2023. When enough reports point to the same generic product, the FDA’s Office of Generic Drugs triggers a review. In 2022, 147 generic drugs were flagged for extra review because of pharmacist reports. Twelve of those led to direct warnings to prescribers and patients.
One example: in 2021, multiple pharmacists reported that a generic version of levothyroxine caused heart palpitations and weight loss in elderly patients. The FDA tested the product and found inconsistent dissolution rates. The manufacturer was asked to change the formulation. That change was made in 2023. Patients got safer meds because pharmacists spoke up.
These aren’t hypotheticals. They’re real outcomes.
What You Can Do Today
You don’t need to wait for a crisis. Start small:
- Ask patients: ‘How’s the new generic working for you?’
- Document every change in response after a switch-even if it’s minor.
- Keep a log of recurring complaints about the same generic product.
- Share patterns with your pharmacy’s clinical team.
- Use the FDA’s free MedWatch training module (Module 4, updated January 2023). It takes 20 minutes.
And if you’re in a state with mandatory reporting? Make sure your pharmacy has a written policy. Train your staff. Track your reports. You’re not just following rules-you’re protecting lives.
Why This Matters More Than Ever
Generic drugs save the U.S. healthcare system over $300 billion a year. They’re essential. But safety can’t be an afterthought.
Between 2015 and 2022, reports of generic drug problems jumped 131%. That’s not because more drugs are faulty-it’s because more people are paying attention. Pharmacists are on the front lines. You see the real-world impact. Your reports help the FDA spot problems before they become national crises.
It’s not about blaming manufacturers. It’s about fixing what’s broken. And if you’re not reporting, you’re letting the system rely on luck-not data.
The next patient who switches to a generic and gets sick? They might be your neighbor. Your friend. Your family. Your report could be the one that stops it from happening again.







9 Comments
Chris Park
Dec 5 2025The FDA’s whole system is a rigged game. They let generic manufacturers use the same label as brand names, even when the pills are chemically different - and then they wonder why people get sick? It’s not about reporting, it’s about accountability. The brand companies own the patent, the generic companies copy it, and the FDA lets them off the hook. Meanwhile, pharmacists get blamed for not reporting the symptoms of a system designed to fail. This isn’t safety - it’s corporate liability laundering.
Akash Takyar
Dec 7 2025While the systemic challenges are undeniable, I believe that each pharmacist’s report, however small, contributes to a cumulative force for change. The FDA’s MedWatch system, though imperfect, remains one of the few structured channels through which frontline professionals can influence national drug safety policy. Even if only one patient is spared harm because of a single report, the effort is morally and ethically justified. Let us not underestimate the power of consistent, documented vigilance.
Geraldine Trainer-Cooper
Dec 8 2025so like... we’re supposed to risk our jobs over a pill that tastes weird?
Kenny Pakade
Dec 9 2025Why are we even talking about this? The FDA’s a joke. We don’t need more paperwork - we need to stop letting foreign factories make our meds. If you want real safety, ban cheap generics. Let’s make pharma pay for American-made pills. This whole ‘report it’ thing is just virtue signaling for overworked pharmacists while China and India keep printing pills that shouldn’t even be in a medicine cabinet.
brenda olvera
Dec 10 2025I’ve seen this firsthand. A grandma in my community switched to a generic and started having panic attacks - she thought she was dying. We switched her back and she cried saying ‘I feel like myself again.’ No one else noticed because no one asks. But we do. And I’m not sorry for caring. We’re not just filling scripts - we’re holding people together. Even if the system doesn’t care, we should.
Myles White
Dec 10 2025It’s important to recognize that the burden of reporting falls disproportionately on pharmacists who are already stretched thin, and while the FDA’s guidelines are technically clear, the reality is that many pharmacists don’t have the time, training, or institutional support to document and submit detailed reports. The process is not user-friendly, the forms are outdated, and there’s no feedback loop - you submit a report and never hear back. Without systemic changes - like integrating reporting into pharmacy management software, offering incentives, or creating regional pharmacovigilance hubs - we’re asking people to do more with less, which is not sustainable. We need infrastructure, not just moral appeals.
Brooke Evers
Dec 12 2025I work in a community pharmacy and I’ve kept a little notebook for over a year now - just notes on patients who say ‘this new pill doesn’t feel right.’ I’ve had five cases where the same generic caused dizziness or nausea across different patients. I didn’t report them right away because I didn’t want to be ‘that pharmacist.’ But after reading this, I filed my first MedWatch form last week. It took 12 minutes. And you know what? I felt like I actually did something. Not because I expected change - but because I stopped pretending I wasn’t part of the solution. If you’re seeing patterns, write them down. You don’t have to fix everything. Just start.
Nigel ntini
Dec 12 2025The real tragedy isn’t the lack of reporting - it’s the silence between professions. Pharmacists see the effects, physicians prescribe the switches, patients suffer, and no one talks. We need interdisciplinary huddles in every pharmacy - pharmacists, nurses, even medical students - to review recurring complaints weekly. This isn’t about bureaucracy; it’s about culture. If we treated drug safety like infection control - with checklists, debriefs, and shared responsibility - we’d stop waiting for someone else to act. The data is in the waiting room. We just need to listen together.
pallavi khushwani
Dec 13 2025It’s funny how we blame the system while ignoring the human part. I’ve seen patients cry because their generic pill made them feel ‘empty’ - not sick, not dizzy - just… gone. No label says that. No lab test measures it. But it’s real. And maybe reporting isn’t about changing policy. Maybe it’s about saying: ‘I saw you. I didn’t ignore you.’ That’s the quiet revolution here. Not the form. Not the NDC. Just someone who noticed - and didn’t look away.