What Really Happens When You Say You’re Allergic to Penicillin?
Most people who say they’re allergic to penicillin aren’t. Seriously. Around 10% of people in the U.S. report a penicillin allergy, but studies show up to 90% of them can safely take it again after proper testing. That’s not a typo. Nine out of ten people who think they’re allergic aren’t. They might’ve had a rash as a kid, felt nauseous after a dose, or heard a family member say they were allergic-and that label stuck. But a true penicillin allergy? That’s rare.
Penicillin and other beta-lactam antibiotics like amoxicillin and cefazolin are among the safest and most effective drugs for common infections. But if you’re labeled allergic, doctors avoid them. Instead, they give you broader-spectrum antibiotics-drugs that are more expensive, harder on your gut, and sometimes less effective. Each unnecessary switch adds about $500 to your hospital bill. And it’s not just money. Overusing these alternatives fuels antibiotic resistance, making future infections harder to treat.
The real problem? Most people never get tested. Skin tests for penicillin are accurate, quick, and safe. If the test is negative, doctors often give a full dose of amoxicillin right there as a challenge. If you don’t react, you’re not allergic. Done. Yet, most people never get past the old note in their chart. That’s why so many stay labeled-and miss out on better, cheaper care.
NSAID Allergies Are Different-And More Common Than You Think
While penicillin allergies are often misdiagnosed, NSAID allergies (like aspirin, ibuprofen, or naproxen) are real-and often misunderstood. Unlike penicillin, which triggers an IgE-mediated immune response, NSAID reactions are usually pharmacological, not allergic. That means your body isn’t attacking the drug like a virus. Instead, it’s overreacting to how the drug changes your body’s chemistry.
People with asthma, nasal polyps, or chronic sinus issues are especially prone. They might get hives, swelling, or trouble breathing within minutes of taking even a small dose. These aren’t random side effects. They’re a known pattern called aspirin-exacerbated respiratory disease (AERD). It’s not an allergy in the classic sense, but the symptoms can be just as scary.
Here’s the twist: unlike penicillin, you can’t test for NSAID allergy with a skin prick. Diagnosis comes from history and controlled challenges. And here’s where it gets interesting-if you’ve had a reaction, you might still be able to take NSAIDs again. Not by avoiding them, but by slowly, carefully reintroducing them under medical supervision. That’s called desensitization.
How Desensitization Works: Turning Off the Alarm
Desensitization isn’t a cure. It’s a temporary reset. Think of it like reprogramming your body’s alarm system. You’re not removing the allergy. You’re teaching your immune system to ignore the drug-for now.
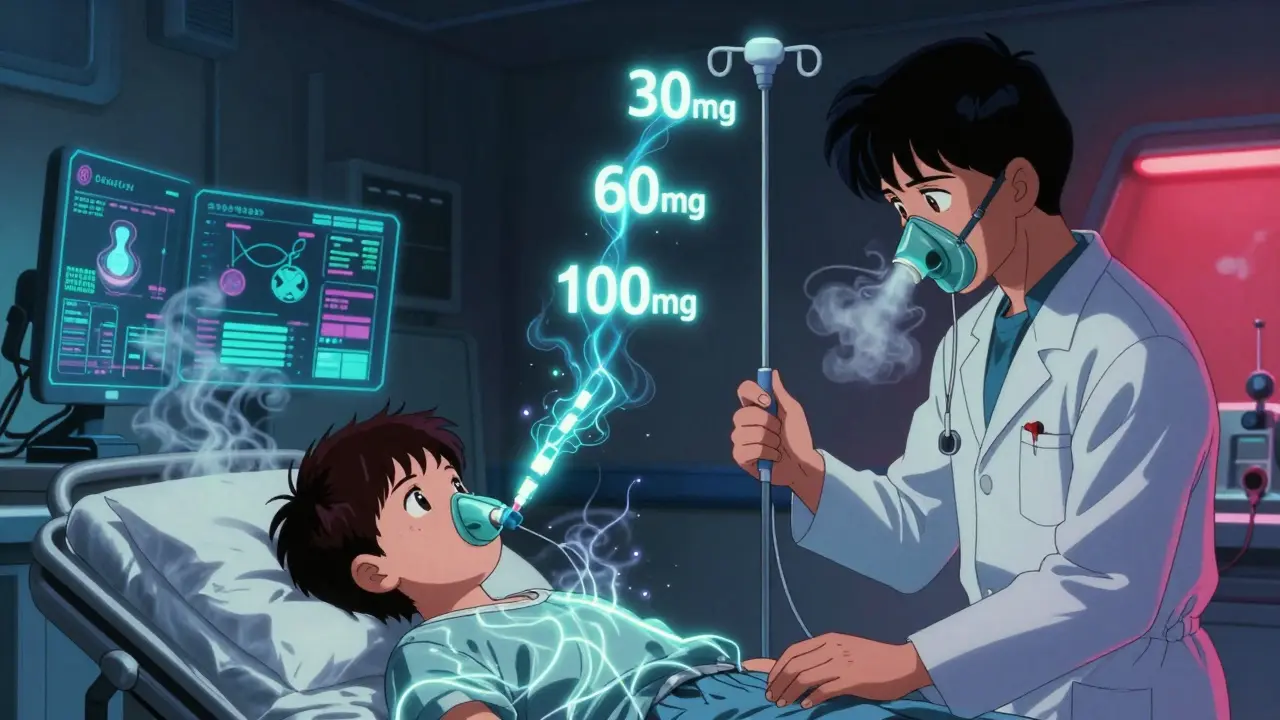
The process starts with a tiny, almost undetectable dose-sometimes as little as one ten-thousandth of a full pill or IV dose. You wait 15 to 20 minutes. If nothing happens, you get a slightly bigger dose. Then another. And another. Over 4 to 8 hours, you’re slowly climbed up to your full therapeutic dose. For penicillin, this might mean starting with 0.001 mg and ending with 500 mg. For aspirin, it might start at 30 mg and build to 325 mg.
It’s done in a hospital or clinic, with emergency meds like epinephrine, oxygen, and IV fluids ready. Nurses and allergists watch you like hawks. If you get hives, wheezing, or a drop in blood pressure, they stop and treat it. But if you make it through? You’re good-for that one course of treatment.
Here’s the catch: once you stop taking the drug, the tolerance fades. If you need it again next month? You go through the whole process again. That’s why it’s not for everyday use. It’s for when you have no other choice-like if you have a life-threatening infection and every other antibiotic has failed.
Protocols for Penicillin vs. NSAIDs: Why They’re Not the Same
Not all desensitization is created equal. Penicillin and NSAIDs need different approaches because they trigger different reactions.
For penicillin, the most common protocol is the 12-step method. It uses three solutions: one with the full drug concentration, one diluted tenfold, and one diluted 100-fold. Doses double every 15-20 minutes. Some centers use faster versions-like a 2-hour and 15-minute schedule for cephalosporins. These work because the reactions are IgE-driven and predictable.
For NSAIDs, especially aspirin, the protocol is longer and more gradual. It’s often done daily over weeks, not hours. You might start with 30 mg of aspirin, then 60 mg the next day, then 100 mg, and so on. This isn’t just about getting you to a full dose. It’s about training your body to tolerate the drug long-term. Once you hit the target dose, you keep taking it every day-even if you don’t need it for an infection. That’s how you maintain tolerance. It’s a maintenance routine, not a one-time fix.
And then there are the exceptions. Some patients with non-IgE reactions-like delayed rashes or organ inflammation-can still be desensitized. But those cases are rarer, more complex, and require even more expertise. That’s why this isn’t something your local pharmacy can do. It’s hospital-based, specialist-only work.
Who Gets Desensitized? And Why It’s Life-Saving
Desensitization isn’t for everyone. It’s reserved for people who truly need the drug and have no alternatives.
Think cancer patients needing paclitaxel (a chemo drug) who broke out in hives during their first infusion. Or someone with a severe bacterial infection who’s allergic to every other antibiotic. Or a person with AERD who needs daily aspirin to control their asthma and sinus polyps. These aren’t hypotheticals. Hospitals like Brigham and Women’s have done over 170 desensitizations for just paclitaxel and docetaxel alone.
Children are another group. Most protocols were designed for adults. But kids with allergies to antibiotics or chemo drugs are being helped too. Allergists now work with pediatric oncologists and infectious disease specialists to make it happen. It’s not easy. It takes planning, patience, and a team. But for a child with a life-threatening infection and no safe antibiotic options? Desensitization isn’t optional. It’s their only shot.
And here’s the kicker: even if you’ve had a severe reaction before-like anaphylaxis-you can still be desensitized. That’s right. The protocol doesn’t care how bad your last reaction was. It only cares that you need the drug now. That’s why it’s so powerful. It turns a dead end into a path forward.

The Risks and Why It’s Not Done Lightly
Desensitization is safe when done right. But it’s not risk-free. About 1 in 10 patients will have a mild reaction during the process-like itching or a slight drop in blood pressure. These are manageable. But in about 1-2% of cases, reactions are severe enough to stop the procedure. That’s why you can’t do this at home. Or in a clinic without an ICU nearby.
And then there’s the issue of resensitization. A small number of people-around 2%-who were successfully desensitized to penicillin and then stopped taking it for months or years, can develop a new allergy when they’re exposed again. It’s rare, but it happens. That’s why doctors sometimes recommend retesting with a skin test before trying it again.
Another problem? Mislabeling. Many people get labeled allergic because they had a side effect-like diarrhea or a headache. But those aren’t allergies. They’re side effects. And if you’re wrongly labeled, you might miss out on the best treatment. That’s why testing comes first. Desensitization is the last resort, not the first step.
There’s also a knowledge gap. Not all doctors know how to do this. Not all hospitals have the protocols. That’s why patients often travel to big medical centers. But that’s changing. More institutions are training teams. More guidelines are being published. The field is growing.
What Comes Next? The Future of Drug Allergy Management
The future is clearer testing, better protocols, and more collaboration.
Right now, penicillin skin testing is the gold standard. But we’re starting to see new tools-like blood tests that detect specific antibodies. They’re not perfect yet, but they’re getting closer. And for NSAIDs? We need better ways to predict who’s at risk before they even take a pill.
Internationally, there’s a push to standardize protocols. Right now, every hospital does it a little differently. That’s dangerous. If you move cities or change hospitals, you might get a different treatment plan. That’s why organizations like the AAAAI and ICALL are pushing for global guidelines.
And the biggest shift? We’re moving away from fear and toward facts. Instead of saying “penicillin allergy” and avoiding it, we’re asking: “Did you get tested?” “Was it a true reaction?” “Can we try a challenge?” That mindset change is saving lives-and money.
For patients, the message is simple: don’t assume you’re allergic. Ask for testing. If you’ve been told you can’t take penicillin or NSAIDs, ask if desensitization is an option. It might be the difference between a long hospital stay and going home with a cure.
Can you outgrow a penicillin allergy?
Yes, many people do. Studies show that 8 out of 10 people who had a penicillin allergy as a child lose it within 10 years. But without testing, you won’t know for sure. Just because you reacted once doesn’t mean you always will. Skin testing or a supervised drug challenge is the only way to confirm you’re no longer allergic.
Is NSAID desensitization permanent?
No. For NSAIDs like aspirin, tolerance lasts only as long as you take the drug daily. If you stop for more than a few days, your body forgets. You’ll need to restart the desensitization process from the beginning. That’s why people with AERD often take low-dose aspirin every day-even when they don’t need it for pain.
Can you be desensitized to multiple drugs at once?
No. Desensitization is done one drug at a time. Trying to desensitize to two drugs together is too risky and not supported by evidence. If you’re allergic to both penicillin and an NSAID, you’ll need two separate procedures, spaced weeks apart. Each requires its own protocol, monitoring, and recovery time.
What if I have a reaction during desensitization?
The procedure is paused immediately. Medications like antihistamines, steroids, or epinephrine are given to stop the reaction. Once you’re stable, the team may try again later with slower dosing-or decide it’s too risky. Severe reactions like laryngeal edema or uncontrolled low blood pressure mean the procedure is stopped for good.
Is desensitization safe for kids?
Yes, but it’s more complex. Most protocols were designed for adults, so pediatric doses and timing need careful adjustment. It’s done in specialized centers with pediatric allergists, oncologists, or infectious disease specialists working together. It’s been successfully used for antibiotics, chemotherapy, and even monoclonal antibodies in children with life-threatening conditions.
Do I need to stop all other medications before desensitization?
Usually, yes. Beta-blockers and ACE inhibitors can interfere with how your body responds to epinephrine during a reaction. Your doctor will likely ask you to pause these for a few days before the procedure. Other meds like antihistamines may also be stopped to avoid masking symptoms. Always follow your allergy team’s instructions exactly.
Next Steps: What to Do If You Think You’re Allergic
If you’ve been told you’re allergic to penicillin or NSAIDs, here’s what to do next:
- Check your medical records. Do you have documentation of a true allergic reaction-like anaphylaxis, hives, or swelling-or just a side effect like nausea or headache?
- Ask your doctor if you’ve ever had a skin test or drug challenge. If not, request a referral to an allergist.
- If you need a specific drug (like an antibiotic for an infection or aspirin for heart health), ask if desensitization is an option.
- Don’t assume you’re allergic forever. Allergies can fade. Testing can free you from unnecessary restrictions.
Drug allergies don’t have to be life sentences. With the right testing and care, you can get the treatment you need-safely and effectively.







13 Comments
Eliana Botelho
Jan 30 2026I mean, I got labeled penicillin-allergic when I was 7 because I got a rash after amoxicillin - turns out it was just heat rash from running around in a fever. No one ever bothered to retest me. Now I’m 34, got pneumonia last winter, and my doctor gave me some weird expensive antibiotic that gave me diarrhea for a week. Like, why are we still doing this? The system is broken. My chart still says ‘penicillin allergy’ even though I’ve taken it twice since then with no issue. No one checks. No one cares. It’s just a checkbox. And now I’m stuck with this label like it’s a tattoo.
Diksha Srivastava
Feb 1 2026This is so important!! 🙌 I’m so glad someone finally explained desensitization in a way that makes sense. So many people live in fear of meds they don’t even need to avoid. If you’ve been told you’re allergic, please, please ask for a test - it could change your life. You deserve better care. And yes, you can outgrow it. Your body isn’t your enemy. 💪
Sidhanth SY
Feb 2 2026Yeah, this is spot on. I work in a rural clinic in India, and we see this all the time - patients avoid penicillin because grandma said it gave her a rash in 1962. Meanwhile, we’re giving them azithromycin for every sinus infection. It’s cheaper to test than to keep wasting antibiotics. And honestly? The desensitization protocol for aspirin in AERD patients? Game changer. We’ve had patients go from constant sinus surgeries to living normally just by taking a daily low-dose aspirin. It’s not magic - it’s science.
Adarsh Uttral
Feb 3 2026so like… i had a reaction to ibuprofen once. got hives. big deal. but i read this and now i think maybe it wasnt even an allergy? like… my asthma got worse that day too. maybe it was just the asthma flaring? so now im scared to take anything. should i just avoid all nsaid forever? or is there a test?
Sarah Blevins
Feb 3 2026The data presented here is statistically misleading. The 90% figure is derived from self-reported allergy cohorts without rigorous confirmation bias controls. Additionally, the economic argument of $500 per unnecessary antibiotic switch ignores regional pricing variances, insurance reimbursement structures, and the downstream costs of managing adverse drug reactions from second-line agents. The piece lacks methodological transparency and overgeneralizes complex immunological phenomena into a simplistic narrative.
Holly Robin
Feb 4 2026THIS IS A PHARMA SCAM. 🚨 They want you to believe you’re not allergic so they can keep selling you penicillin. Why do you think they don’t want you to get tested? Because if you find out you’re NOT allergic, you’ll stop buying their expensive alternatives! And what about the people who actually died from penicillin? Are their families just supposed to say ‘oops, my bad, you weren’t allergic’? I’ve seen it happen. They push these protocols because they’re cheaper than developing new drugs. Don’t be fooled. Your body knows. Trust your instincts.
Shubham Dixit
Feb 4 2026India has been doing this right for decades. We don’t waste money on fancy skin tests. If you had a reaction, you avoid it. Period. Why risk it? In the West, you people treat medicine like a video game - ‘oh I’ll just desensitize myself like a boss’. We have 1.4 billion people. We can’t afford your experimental nonsense. We use what works. Simple. Safe. Proven. Don’t bring your American overcomplicated healthcare nonsense here.
KATHRYN JOHNSON
Feb 5 2026Desensitization is not a cure. It is a temporary, high-risk, hospital-bound procedure that should only be considered in terminal cases. The normalization of this practice reflects a dangerous erosion of medical caution. We are replacing evidence-based caution with convenience-driven experimentation. The fact that children are being subjected to this is alarming. The FDA should issue a warning.
Sazzy De
Feb 6 2026My mom was told she was allergic to penicillin in the 80s. She never got tested. Last year she got a UTI and they gave her cipro. She got really sick. I found this article, convinced her to see an allergist. Turned out she wasn’t allergic. They gave her amoxicillin the next day. She felt better in 12 hours. I’m so glad we finally did this. Just… ask. Seriously. It’s not that hard.
Blair Kelly
Feb 7 2026Let me get this straight - you’re telling me if I had anaphylaxis to penicillin at age 5, I can just go back to it now like nothing happened? That’s not bravery. That’s insanity. This isn’t a superhero origin story. This is a one-way ticket to the ICU. And you’re telling people to just ‘ask for testing’? What if the allergist is busy? What if your insurance denies it? What if you’re in a rural town? This article reads like a corporate ad for big pharma’s new ‘allergy eraser’ product. Wake up.
Gaurav Meena
Feb 7 2026Man, this gave me chills 😊 I work with cancer kids in Mumbai - one of them had a reaction to paclitaxel. We did desensitization over 8 hours. She made it. Now she’s back in school. Her mom cried. I cried. This isn’t just medicine - it’s hope. And yes, it’s hard. But when you see a child walk out of the hospital after being told ‘no treatment possible’? That’s why we do it. You’re not alone. We’re in this together. 💙
Carolyn Whitehead
Feb 8 2026I never thought about how a label from childhood can follow you forever. My sister was allergic to aspirin as a kid. Now she’s 40 and has heart disease. She can’t take baby aspirin to protect her heart because of that old note. She’s scared to even ask. I’m printing this out for her tomorrow. Maybe this is the push she needs. Thank you for writing this.
Katie and Nathan Milburn
Feb 8 2026While the clinical utility of desensitization protocols is well-documented in peer-reviewed literature, the ethical implications of encouraging patients to undergo high-risk, time-intensive procedures - particularly in resource-constrained settings - warrant serious consideration. The presumption that all patients possess equal access to specialized care, emergency infrastructure, and follow-up monitoring is, in practice, untenable. A more equitable approach would prioritize widespread, low-cost, validated diagnostic screening prior to intervention.