NMS Symptoms: What They Are, How They Happen, and What to Do
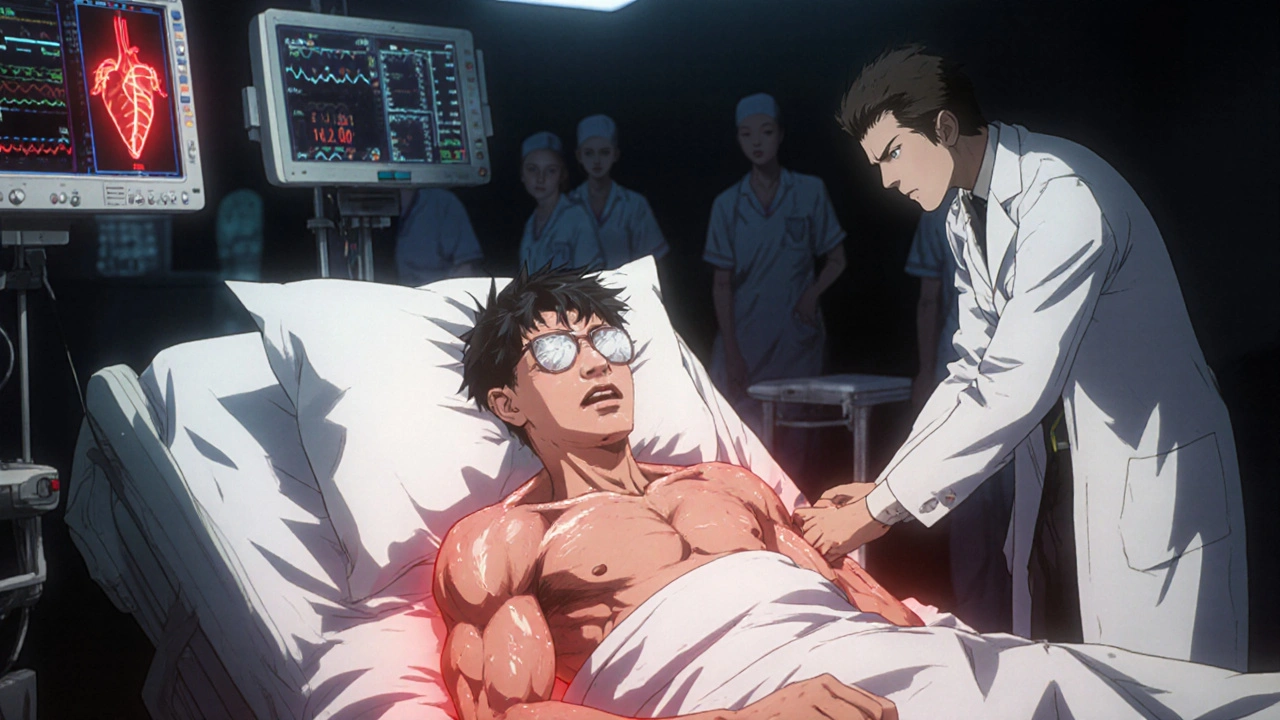
When someone develops neuroleptic malignant syndrome, a rare but deadly reaction to certain psychiatric medications that causes severe muscle rigidity, fever, and organ stress. Also known as NMS, it’s not just side effects—it’s a medical emergency that needs immediate treatment. NMS symptoms usually show up within days to weeks after starting or increasing a drug like risperidone, haloperidol, or even older antipsychotics. You won’t just feel a little off—you’ll have stiff muscles you can’t move, a fever over 102°F, sweating, confusion, and a racing heart. It’s not the same as serotonin syndrome, though they look similar. NMS is tied to dopamine blockage, while serotonin syndrome comes from too much serotonin. Mixing the two can be deadly, and doctors sometimes misdiagnose one for the other.
What raises your risk? Starting a high dose of an antipsychotic, switching meds too fast, or combining them with other drugs like lithium, SSRIs, or even some anti-nausea pills. People with Parkinson’s who take dopamine blockers are also at higher risk. It’s not just about the drug—it’s about how your body handles it. Dehydration, heat, or physical stress can push a slow-burning reaction into full-blown NMS. If you or someone you care for is on an antipsychotic and suddenly can’t move, feels hot, or acts confused, don’t wait. Call 911 or get to an ER. Delaying treatment can lead to kidney failure, seizures, or death.
The good news? If caught early, NMS can be reversed. Stopping the trigger drug, giving fluids, cooling the body, and sometimes using dantrolene or bromocriptine can save lives. But prevention is better than cure. If you’re on these meds, know the signs. Talk to your doctor before changing doses. Keep a list of every drug you take—even over-the-counter ones. And if you’ve had NMS once, you’re at higher risk for it again—so future prescriptions need extra caution.
Below, you’ll find real-world guides from pharmacists and clinicians on how these reactions happen, which drugs are most likely to cause them, how to spot them before it’s too late, and what to ask your provider to stay safe. These aren’t theory pages—they’re practical tools for people who take these meds, care for someone who does, or work in healthcare and need to act fast.