DOAC Dosing Advisor for Obesity
Patient Assessment
When someone has obesity-especially severe obesity-their body doesn’t just carry extra weight. It changes how drugs move through their system. This is a big deal when it comes to blood thinners called DOACs (direct oral anticoagulants). These medications-apixaban, rivaroxaban, dabigatran, and edoxaban-are now the go-to choice for preventing strokes in atrial fibrillation or treating blood clots. But for people with a BMI over 40 or weighing more than 120 kg, the old rules don’t always apply. The question isn’t whether to use them. It’s: Which one, and at what dose?
Why Obesity Changes the Game
Obesity isn’t just about weight. It affects how drugs are absorbed, distributed, metabolized, and cleared from the body. In the early 2010s, when DOACs were approved, most clinical trials excluded people with severe obesity. That left doctors guessing. Should they dose the same? Increase the dose? Or stick to what’s on the label? Fast forward to 2026, and we have real-world data from over 15,000 patients. The answer isn’t simple, but it’s clear: standard dosing works for most, but not all DOACs are equal in obese patients.Apixaban: The Most Reliable Choice
Apixaban stands out. Whether someone weighs 100 kg or 180 kg, the standard dose-5 mg twice daily for atrial fibrillation, or 10 mg twice daily for the first week of deep vein thrombosis (DVT) treatment-remains safe and effective. A 2020 study tracking 15,349 patients with atrial fibrillation found no difference in stroke or bleeding rates between those with BMI under 30 and those over 40. In a separate registry of 2,147 obese patients, those on apixaban had the lowest major bleeding rate at 2.1% per year. Even in patients with BMI over 50, no thrombotic events were reported when they stayed on standard apixaban. The International Society on Thrombosis and Haemostasis (ISTH) and the European Heart Rhythm Association both give apixaban a Class I recommendation for all BMI levels. No need to adjust. No need to monitor. Just prescribe the standard dose.Rivaroxaban: Almost as Solid
Rivaroxaban is the second-best option. For atrial fibrillation, 20 mg once daily (or 15 mg if kidney function is low) is effective in obese patients. For treating blood clots, the initial 15 mg twice daily for 21 days, then 20 mg once daily, holds up well. A 2022 meta-analysis showed rivaroxaban’s efficacy in obese patients was nearly identical to non-obese patients, with a hazard ratio of 0.92-meaning it performed slightly better, not worse. The ISTH 2021 update explicitly says rivaroxaban can be used at standard doses regardless of weight or BMI. But here’s the catch: rivaroxaban’s absorption can be affected by food. If a patient has a large meal, the drug’s absorption improves. That’s not a problem in most people, but in those with severe obesity and irregular eating patterns, consistency matters. Stick to taking it with food, every day.Dabigatran: The Risky One
Dabigatran is the outlier. It works well for preventing strokes in obese patients, but it comes with a serious downside: gastrointestinal bleeding. Studies show that in patients with BMI over 40, dabigatran increases the risk of GI bleeding by 37% compared to non-obese patients. One study found a 2.3-fold higher risk of major GI bleeding compared to those with normal BMI. Why? It’s likely because dabigatran concentrates in the stomach lining and may irritate it more in people with higher abdominal fat or altered gastric motility. The European Heart Rhythm Association and the Anticoagulation Forum both warn against using dabigatran in morbidly obese patients. If someone already takes it and gains weight, consider switching. If you’re choosing a DOAC for the first time in someone with BMI >40, avoid dabigatran.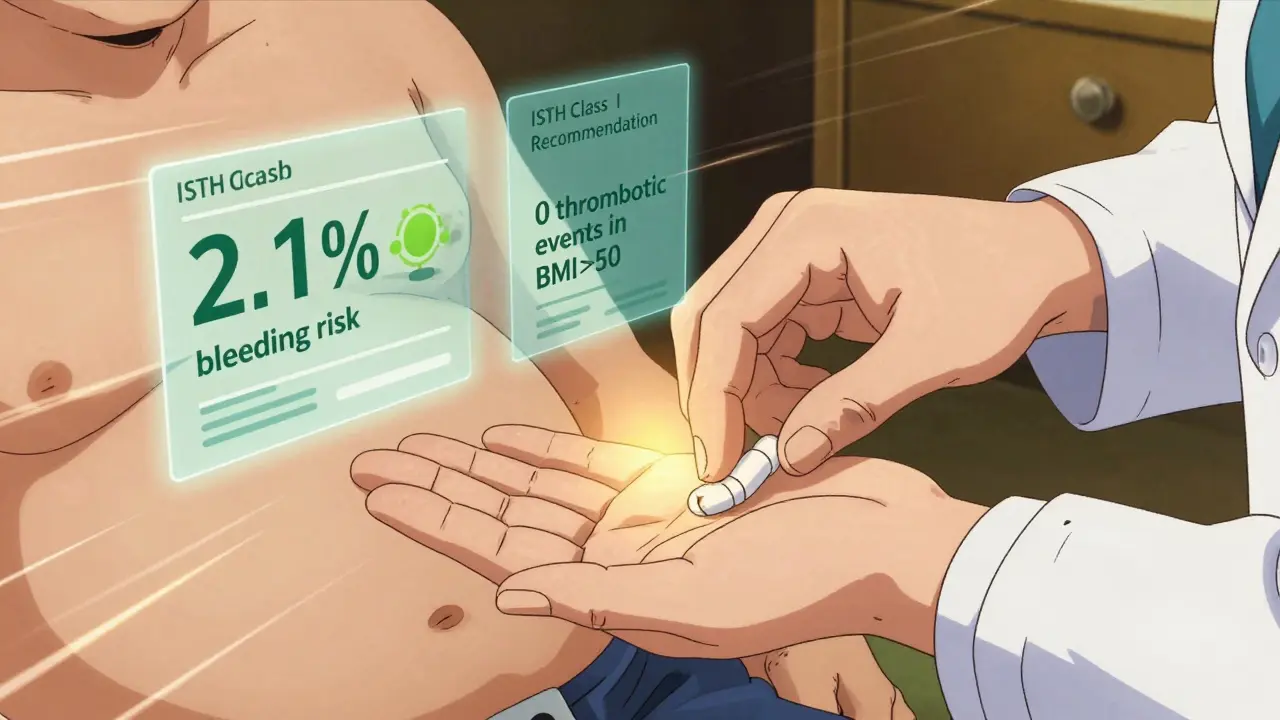
Edoxaban: Mixed Signals
Edoxaban’s behavior is less predictable. Most studies show that standard dosing (60 mg once daily) works fine for patients with BMI up to 40. But at the extreme end-BMI over 50-there are red flags. In a study of 347 patients with BMI over 50, 18.2% had subtherapeutic anti-Xa levels on standard-dose edoxaban. That means their blood wasn’t adequately thinned. The 2023 ACC/AHA/ACCP/HRS guideline now recommends considering the reduced dose (30 mg) for patients with BMI >50. This is one of the few cases where dose adjustment might be needed. But here’s the problem: we don’t have enough data to say for sure. No large trials exist for people over 160 kg. So if you’re treating someone with extreme obesity, and edoxaban is the only DOAC available, consider checking anti-Xa levels or switching to apixaban.What About Dose Increases?
Some doctors think, “If standard dose doesn’t seem enough, give more.” But that’s dangerous. The ISTH 2021 guidance is clear: there is no evidence to support higher-than-standard dosing in obese patients. Increasing the dose doesn’t improve protection against clots. Instead, it raises bleeding risk without benefit. One study tried doubling apixaban to 10 mg twice daily in patients with BMI >40. The result? No reduction in clots-but bleeding rates jumped. Don’t overcorrect. Stick to the label.Real-World Numbers You Should Know
- 42.4% of U.S. adults have BMI ≥30 (obesity). - 9.2% have BMI ≥40 (morbid obesity). - DOACs now make up 78% of new anticoagulant prescriptions for obese patients with atrial fibrillation (up from 32% in 2014). - Apixaban is used in over 50% of obese patients on DOACs. - Major bleeding rates: apixaban (2.1%), rivaroxaban (2.4%), dabigatran (3.8%). These numbers aren’t abstract. They’re from real clinics, hospitals, and registries. This is what’s working.
What to Do in Practice
Here’s a simple guide:- For atrial fibrillation: Use apixaban 5 mg twice daily. If the patient is 80+, weighs ≤60 kg, or has kidney issues, drop to 2.5 mg twice daily. Avoid dabigatran.
- For blood clots (VTE): Use apixaban 10 mg twice daily for 7 days, then 5 mg twice daily. Rivaroxaban 15 mg twice daily for 21 days, then 20 mg once daily is also fine.
- For BMI >50 or weight >160 kg: Stick with apixaban or rivaroxaban. Avoid dabigatran. Consider edoxaban only if others aren’t available, and monitor anti-Xa levels if possible.
- Never increase the dose beyond what’s approved, even if you’re worried.
What’s Coming Next?
A major trial called DOAC-Obesity (NCT04588071) is currently enrolling 500 patients with BMI ≥40. It’s testing whether standard dosing truly works across all weight ranges. Results are expected in late 2024. Meanwhile, researchers are working on point-of-care tests to measure DOAC levels quickly in the clinic-something that could help tailor doses in extreme cases. But for now, we have enough data to make smart choices.Bottom Line
You don’t need to overthink DOAC dosing in obesity. For most people-even those with severe obesity-standard doses of apixaban and rivaroxaban are safe and effective. Dabigatran should be avoided. Edoxaban is okay for most, but tread carefully at the extremes. And never increase the dose. The data is clear. The guidelines are solid. The right choice isn’t complicated. It’s just apixaban.Can I use DOACs if I weigh over 120 kg?
Yes. Standard doses of apixaban and rivaroxaban are safe and effective for people weighing over 120 kg. Large studies and real-world data confirm this. Dabigatran should be avoided, and edoxaban may need monitoring if weight exceeds 160 kg.
Is dabigatran dangerous for obese patients?
Yes, dabigatran carries a 37% higher risk of gastrointestinal bleeding in obese patients with BMI over 40. While it still prevents strokes, the bleeding risk outweighs the benefit for most in this group. It’s not recommended as a first choice.
Should I increase the DOAC dose for someone with obesity?
No. Increasing the dose beyond the standard regimen does not improve protection against clots and increases bleeding risk. There is no evidence supporting higher doses in obese patients. Stick to the approved dose.
What’s the best DOAC for someone with BMI over 50?
Apixaban is the best option. It has the strongest safety and efficacy data in this group. Rivaroxaban is a good alternative. Edoxaban may have subtherapeutic levels in some patients, so it’s not ideal. Avoid dabigatran entirely.
Do I need to monitor DOAC levels in obese patients?
Generally, no. DOACs don’t require routine monitoring. But for patients with BMI over 50 on edoxaban, or if there’s concern about effectiveness or bleeding, anti-Xa levels can be checked. This isn’t standard practice, but it’s an option when uncertainty exists.




10 Comments
Robert Petersen
Feb 12 2026This is exactly the kind of practical, evidence-based guide we need in clinical practice. Apixaban as the go-to for obesity? Absolutely. I've been pushing this in my clinic for years, and the data just keeps confirming it. No more guessing. No more overcomplicating. Just prescribe the right drug and let it work.
Also, props for calling out dabigatran - so many still default to it out of habit. Time to update our mental algorithms.
Ernie Simsek
Feb 13 2026bro. apixaban is the GOAT. 🥇
weird how we used to overthink this so much. now it's just: if they're obese? apixaban. 5mg BID. done. no labs. no adjustments. just give it and walk away. rivaroxaban's fine too, but apixaban's the chill uncle who never messes up.
Reggie McIntyre
Feb 14 2026I love how this post distills chaos into clarity. It's like someone took all the confusing guidelines, threw them in a blender, and then served up a cold beer with a napkin that says 'just use apixaban'.
Also, the fact that we now have 15k+ real-world patients confirming this? That’s not data - that’s a revolution. We’ve moved from guesswork to gospel.
Rachidi Toupé GAGNON
Feb 16 2026Apixaban for the win. 🙌
Simple. Safe. Effective. No drama. No monitoring. Just give it and trust the science. Rivaroxaban’s a solid second. Dabigatran? Nah. Edoxaban? Only if you’re desperate. And never, ever increase the dose. That’s how you end up in the ER with a bleeding ulcer.
Joanne Tan
Feb 16 2026OMG YES THIS. I’ve been telling my residents for months: stop overthinking the weight. Apixaban is the MVP. I had a patient at 190kg last week - standard dose. No issues. No bleeds. No drama. Just happy patient, happy docs. Why do we make things harder than they are? 🤦♀️
Brad Ralph
Feb 18 2026So... we spent 10 years overcomplicating this, and the answer was always apixaban? 🤨
Classic. Like spending millions on a rocket to Mars when the answer was 'just use a ladder'.
christian jon
Feb 18 2026THIS IS WHY WE CAN’T HAVE NICE THINGS! The pharmaceutical industry has been pushing DOACs like candy, and now we’re blindly following guidelines without questioning who funded the studies! Who benefits from apixaban being the 'gold standard'? Who wrote the ISTH guidelines? Did they get paid by BMS? Did you even check the conflict of interest disclosures?!?!?!?!
Autumn Frankart
Feb 20 2026You know what’s really happening? They’re using obesity as an excuse to push cheaper drugs. Apixaban? It’s cheaper than warfarin. That’s why they’re all pushing it. They don’t care about bleeding risk - they care about profit margins. And dabigatran? They’re just scared of the GI bleed data because it’s too messy for their marketing team. This isn’t medicine - it’s corporate theater.
athmaja biju
Feb 21 2026In India, we rarely see patients above 120kg, but when we do, we stick to apixaban. The data is clear. Also, we don’t have the luxury of checking anti-Xa levels. So we go with what works. Apixaban. Always. No debate. The rest? Just noise.
Sophia Nelson
Feb 22 2026I’ve been using apixaban for obese patients for 3 years now. No issues. No bleeding. No clots. Just works. Why is this even a conversation?