Porphyria Attack Risk Calculator
This tool estimates your risk of a porphyria attack based on your menstrual cycle phase and related hormonal factors. It helps identify when you might be at increased risk so you can take preventive measures.
Important: This tool provides general guidance only and should not replace professional medical advice. Always consult your healthcare provider for personalized treatment.
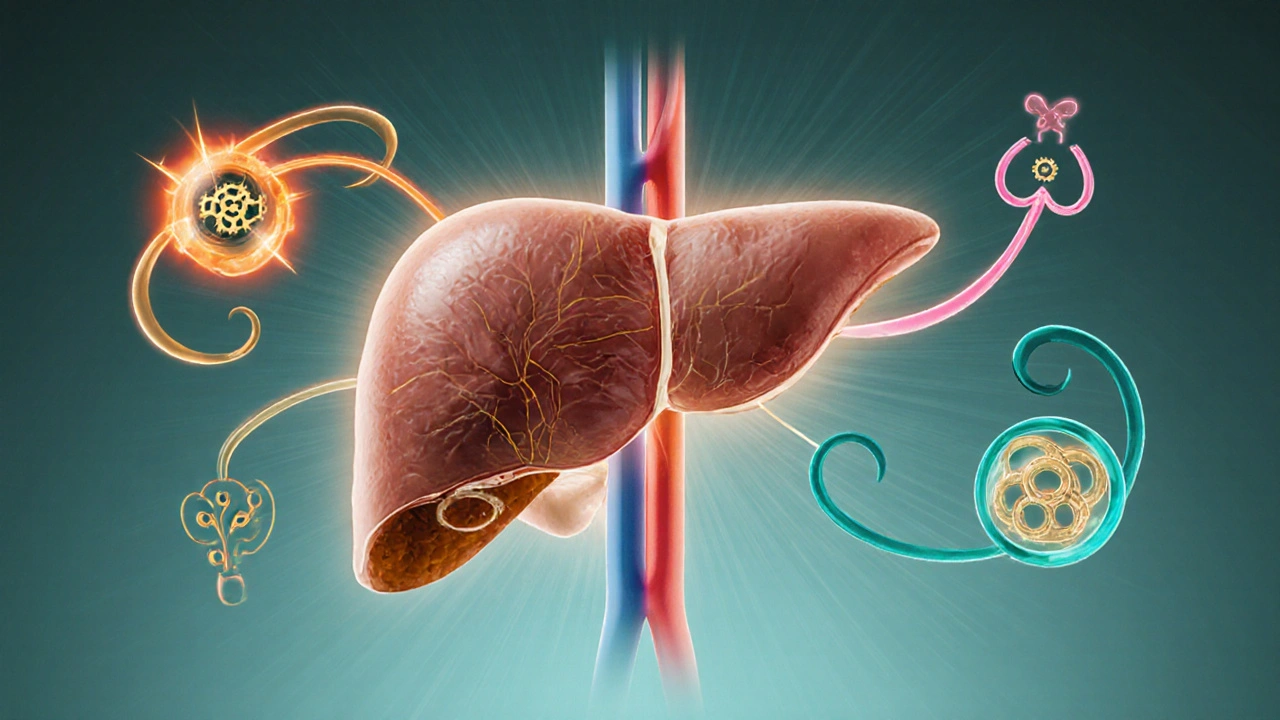
When a rare metabolic disorder like porphyria meets the body’s hormone factory, the results can be baffling. Patients often wonder why a skin rash suddenly flares after a stressful week or why abdominal pain spikes around their menstrual cycle. The answer lies in the tight link between the heme‑making pathway and the endocrine system. This guide untangles that connection, shows which hormones tend to go haywire, and gives practical tips to keep the balance in check.
Key Takeaways
- Porphyria is a group of genetic disorders that disrupt heme biosynthesis, leading to toxic precursors.
- The endocrine system regulates stress, reproductive, and metabolic hormones that can trigger or worsen porphyria attacks.
- Estrogen, cortisol, and thyroid hormones are the most common culprits in hormonal imbalances for porphyria patients.
- Monitoring hormone levels alongside porphyrin tests helps catch flare‑ups early.
- Management includes trigger avoidance, hormone‑modulating therapy, and lifestyle adjustments such as stress reduction and balanced nutrition.
Understanding Porphyria
Porphyria is a cluster of inherited metabolic disorders that impair heme biosynthesis, the process that creates the iron‑containing molecule essential for hemoglobin, cytochromes, and various enzymes. The pathway involves eight enzymes; a deficiency in any one leads to a buildup of porphyrin precursors, which are photo‑reactive and neurotoxic.
Two forms dominate clinical practice:
- Acute intermittent porphyria (AIP) - characterized by neurovisceral attacks, abdominal pain, and psychiatric symptoms.
- Porphyria cutanea tarda (PCT) - presents with blistering skin lesions on sun‑exposed areas.
Both share a common trigger: a rapid rise in the demand for heme or a sudden drop in enzyme activity. Hormones are powerful modulators of that demand.
How the Endocrine System Interacts with Porphyria
Endocrine system is a network of glands that release hormones directly into the bloodstream, governing growth, metabolism, reproduction, and stress response. When hormones surge or dip, the liver - the primary site of heme production - receives signals to adjust enzyme activity. In porphyria, these adjustments can backfire.
Key pathways:
- Stress axis (hypothalamic‑pituitary‑adrenal) - cortisol spikes increase the liver’s need for cytochrome P450 enzymes, which consume heme.
- Reproductive axis (hypothalamic‑pituitary‑gonadal) - estrogen and progesterone modulate the expression of porphobilinogen deaminase, the enzyme deficient in AIP.
- Thyroid axis - thyroid hormones accelerate basal metabolic rate, indirectly lifting heme turnover.
When any of these axes go out of sync, the already‑strained heme pathway may overload, releasing porphyrin precursors that provoke attacks.

Common Hormonal Imbalances in Porphyria Patients
Studies from European porphyria centers (2023) show a clear pattern: estrogen‑dominant women and patients with chronic stress‑induced cortisol elevation experience the highest attack frequency.
| Hormone | Typical Effect on Porphyria | Associated Symptoms |
|---|---|---|
| Estrogen | Up‑regulates ALA synthase, raising porphyrin precursor production | Abdominal pain, anxiety, worsening of skin lesions during menstrual peaks |
| Cortisol | Stimulates hepatic cytochrome P450, increasing heme consumption | Sudden neuropathy, fatigue, heightened sensitivity to medication triggers |
| Thyroid hormones (T3/T4) | Accelerate metabolic rate, indirectly pushing heme demand | Heat intolerance, tremor, overlapping with porphyria‑induced tachycardia |
| Insulin | Fluctuations can modify hepatic enzyme activity | Post‑prandial nausea, occasional hypoglycemia during attacks |
Men with AIP sometimes report low testosterone, but the data are less consistent. The key takeaway is that any hormone that pushes the liver to produce more heme‑dependent enzymes can tip a stable porphyria patient into crisis.
Clinical Manifestations Linked to Hormone Fluctuations
Because hormonal cycles are predictable, many patients learn to anticipate their own symptom patterns.
- Menstrual‑related attacks: Roughly 60% of women with AIP note that cramps and neuro‑psychiatric symptoms worsen a few days before or during menses, coinciding with estrogen peaks.
- Stress‑induced neurology: High‑stress weeks often precede peripheral neuropathy or seizures, reflecting cortisol‑driven enzyme up‑regulation.
- Thyroid‑linked skin changes: Hyperthyroid patients may see PCT lesions become more extensive due to increased skin blood flow and oxidative stress.
Recognizing these patterns allows clinicians to time preventive measures - such as short‑term hormone blockers - around the most vulnerable windows.
Diagnostic Approach for Hormonal Imbalance in Porphyria
Accurate diagnosis hinges on two parallel tracks: porphyrin profiling and hormone assessment.
- Porphyrin tests: Spot urine for porphobilinogen (PBG) and delta‑aminolevulinic acid (ALA); plasma fluorescence for PCT; fecal coproporphyrin for liver‑type porphyrias.
- Hormone panels: Serum estradiol and progesterone in women, cortisol (AM and PM), TSH/T4 for thyroid status, and fasting insulin/glucose if metabolic issues are suspected.
- Genetic confirmation: Sequencing of the HMBS gene (for AIP) or UROD gene (for PCT) solidifies the diagnosis and informs family screening.
Timing matters - hormone levels fluctuate, so draw blood at consistent points in the menstrual cycle or cortisol rhythm to avoid false negatives.

Management Strategies: Balancing Hormones and Heme
Effective care blends trigger avoidance, hormonal modulation, and symptomatic treatment.
- Trigger avoidance: Limit alcohol, smoking, high‑dose vitaminA, and porphyrin‑inducing drugs (e.g., barbiturates, certain antibiotics).
- Hormone modulation:
- For estrogen‑related attacks, low‑dose oral contraceptives with progestin‑only or GnRH agonists can blunt the surge.
- Cortisol spikes are best managed with stress‑reduction techniques - mindfulness, regular sleep, and, when needed, low‑dose glucocorticoid replacement only under specialist supervision.
- Thyroid dysfunction should be corrected to euthyroid levels; beta‑blockers may help if hyperthyroidism aggravates symptoms.
- Heme‑targeted therapy: Intravenous hemin (Panhematin) for acute attacks, replenishing hepatic heme stores and down‑regulating ALA synthase.
- Nutritional support: Adequate carbohydrate intake (≥ 70% of calories) reduces ALA production; avoid fasting.
- Regular monitoring: Quarterly porphyrin panels and hormone checks, especially during life stages with hormonal upheaval (puberty, pregnancy, menopause).
Patient stories reinforce these points. One 32‑year‑old teacher with AIP reduced attack frequency from monthly to twice a year after switching to a progestin‑only pill and adopting a daily 30‑minute meditation routine. Another man with PCT saw his skin lesions clear after treating an undiagnosed subclinical hyperthyroid state.
When to Seek Immediate Care
Acute neurovisceral attacks can become life‑threatening. Call emergency services if you experience:
- Severe, unrelenting abdominal pain not relieved by typical analgesics.
- Rapidly progressing weakness or numbness in limbs.
- Seizures, extreme confusion, or hallucinations.
- Dark urine that appears reddish‑brown (a sign of porphyrin excretion).
Prompt IV hemin administration, fluid resuscitation, and removal of provoking drugs are the standard emergency protocol.
Frequently Asked Questions
Can pregnancy worsen porphyria attacks?
Yes. Pregnancy raises estrogen and progesterone dramatically, which can trigger AIP attacks in up to 30% of women. Close monitoring, low‑dose hemin prophylaxis, and hormone‑adjusted therapy are usually required.
Is it safe to take hormone replacement therapy (HRT) after menopause?
It depends on the porphyria type. For AIP, standard estrogen‑based HRT can provoke attacks, so a transdermal low‑dose estradiol combined with a progestin patch is sometimes used under specialist guidance. Non‑hormonal options for vasomotor symptoms are also viable.
Do dietary changes affect hormonal balance in porphyria?
A diet rich in complex carbs stabilizes blood sugar, which can blunt cortisol spikes. Avoiding excessive caffeine and processed sugars also helps keep insulin levels steady, indirectly supporting hormone equilibrium.
What tests confirm a hormonal trigger for an attack?
Combine a quantitative urine PBG/ALA test with a targeted hormone panel performed within 24‑48hours of the attack. A noticeable rise in estradiol, cortisol, or thyroid hormones alongside elevated porphyrins suggests a hormonal trigger.





15 Comments
Lawrence D. Law
Oct 14 2025The presented correlation between menstrual cycle phases and porphyria attack propensity is noteworthy; however, the omission of peer‑reviewed endocrinological references undermines the argument's credibility, and the reliance on anecdotal risk thresholds detracts from scientific rigor.
Odin Zifer
Oct 21 2025They want you to trust a cheap online calculator while the pharma giants hide the real data on hormonal triggers and keep the cure under lock‑and‑key.
Marisa Leighton
Oct 28 2025Understanding how estrogen and progesterone fluctuations interact with the heme synthesis pathway can empower patients to anticipate attacks.
When you track your cycle diligently, you gain insight into the windows of heightened vulnerability.
Integrating stress‑management techniques during the luteal phase can further reduce the likelihood of a flare‑up.
Nutritional support, such as maintaining adequate carbohydrate intake, complements hormonal monitoring.
Many individuals report noticeable improvements after aligning medication schedules with their ovulation peaks.
The calculator, while simple, serves as a visual cue that encourages proactive self‑care.
Collaborative discussions with endocrinologists can refine the risk model to your personal physiology.
Remember that each body responds uniquely; the tool is a guide, not a guarantee.
Embracing a holistic approach that includes sleep hygiene amplifies the benefits of hormonal awareness.
Research indicates that cortisol spikes can exacerbate porphyria, making stress level inputs highly relevant.
By lowering stress through mindfulness or gentle exercise, you may blunt the hormonal surge that precipitates attacks.
It's also wise to keep a symptom diary to correlate calculated risk scores with actual episodes.
Over time, patterns emerge that can inform both you and your healthcare team.
Stay hopeful, because knowledge truly is a powerful preventive weapon.
Keep sharing your experiences with the community, as collective data will drive better tools in the future.
Chelsea Hackbarth
Nov 4 2025Great start! This tool could be a game‑changer for many; 🚀 just make sure to double‑check the inputs! 😄
Adam Shooter
Nov 11 2025The algorithmic stratification of porphyria risk via endocrine phase mapping lacks a robust multivariate regression framework, thereby limiting its predictive validity.
Shanmughasundhar Sengeni
Nov 18 2025Looks kinda useful but honestly seems like a quick hack rather than a deep medical analysis.
Christina Burkhardt
Nov 25 2025When you’re navigating hormonal triggers, it helps to keep a supportive network; sharing your cycle data with a trusted friend can add an extra layer of accountability and encouragement.
liam martin
Dec 2 2025Ah, the cold equations of risk scores! Yet amidst the numbers, we must ask: does the soul of a patient bow to statistics, or does it rebel?
Ria Ayu
Dec 9 2025Your breakdown is truly uplifting; I’ve found that pairing such tools with gentle yoga sessions during the luteal phase brings a noticeable calm.
maya steele
Dec 16 2025Indeed, fostering a collaborative environment is essential; coordinated care involving both clinicians and close confidants enhances adherence to preventive strategies.
Sharon Lax
Dec 23 2025The presented risk matrix suffers from oversimplification, neglecting the intricate feedback loops inherent in the hypothalamic‑pituitary‑adrenal axis.
paulette pyla
Dec 30 2025Wow, groundbreaking insight-never thought of that before.
Benjamin Cook
Jan 6 2026Hey guys!! This tool is super helpful!! Just remember to update your stress level daily!!! 😅
Breanne McNitt
Jan 12 2026Totally agree!! Consistency is key, and sharing progress can keep the whole community motivated!!
Christopher Ellis
Jan 19 2026If you rely on a calculator you might miss the bigger picture of diet and genetics.