Every pill, injection, or capsule that ends up on a pharmacy shelf didn’t just appear there. It traveled through a complex web of manufacturers, distributors, and wholesalers - and if even one link in that chain is broken, someone could get a fake, contaminated, or expired drug. In 2023, the FDA reported over 2,100 suspicious drug diversion cases, and global losses from counterfeit medicines still hover around $200 billion a year. For pharmacies, especially small independent ones, meeting legitimate drug procurement standards isn’t optional - it’s survival.
What Makes a Drug Supply Chain Legitimate?
A legitimate drug supply chain doesn’t just mean buying from a company that sounds official. It means every step follows strict rules designed to stop counterfeit, stolen, or tampered drugs from entering the system. The backbone of this system in the U.S. is the Drug Supply Chain Security Act (DSCSA), passed in 2013 and fully enforced by November 27, 2023. This law requires every pharmacy, wholesaler, and manufacturer to exchange electronic transaction data - including product details, lot numbers, and expiration dates - at every handoff. No paper records. No gaps. Everything must be traceable.This isn’t just bureaucracy. It’s a firewall. In 2022, a hospital in Ohio had to quarantine $87,000 worth of medication because a distributor’s system failed to send complete DSCSA transaction history. That’s not a rare glitch - 58% of health systems still struggle with incomplete data from suppliers. If you can’t verify the chain of custody, you can’t trust the product.
The Must-Have Supplier Checks
You can’t just pick the cheapest supplier and call it good. Legitimate procurement means vetting every vendor before you even place an order. The American Society of Health-System Pharmacists (ASHP) outlines seven non-negotiable criteria:- Current FDA registration and state pharmacy licenses
- Proof of compliance with current Good Manufacturing Practices (cGMP)
- Documented quality management systems
- No history of recalls or adverse events
- Security measures to prevent theft or diversion
- Financial stability - no fly-by-night operators
- Full DSCSA compliance with electronic tracing
Suppliers must provide documentation proving they’ve met these standards for at least three consecutive years. If they can’t, walk away. One hospital pharmacy director told me they stopped working with a supplier after discovering their FDA registration had expired six months earlier. That’s not negligence - it’s negligence with patients’ lives on the line.
Verification Is Not Optional - It’s Daily Work
Even the best supplier can make a mistake. That’s why every incoming shipment must be checked at the door. Barcode scanning isn’t a nice-to-have - it’s mandatory. ASHP recommends scanning 100% of incoming pharmaceuticals to match the National Drug Code (NDC), lot number, and expiration date against your purchase order. If the system flags a mismatch, quarantine the product immediately. Don’t assume it’s a typo. Don’t rush to use it. Investigate.Temperature control matters too. Vaccines, insulin, and many biologics must stay between 2°C and 8°C. If your refrigerator breaks during a shipment, and you don’t have real-time monitoring logs, you can’t prove the drug was safe. Many pharmacies still use manual thermometers - that’s not enough anymore. Digital loggers with alerts are now standard for any facility handling temperature-sensitive drugs.
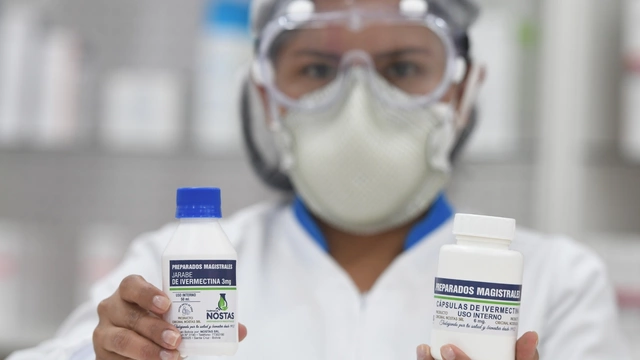
White Bagging vs. Brown Bagging - The Hidden Risks
Some pharmacies try to cut costs or speed things up by using nontraditional methods like “brown bagging” (patients bring drugs from retail pharmacies to clinics) or “white bagging” (specialty pharmacies deliver directly to clinics). These methods sound convenient, but they’re risky. ASHP found that 42% of health systems using these methods had at least one medication error linked to improper handling or lack of verification. Who’s responsible if a patient gets the wrong dose because the drug wasn’t stored right during transport? The pharmacy. The clinic? The patient? No one, until someone gets hurt - and then the lawsuits start.Stick to direct procurement from authorized distributors or manufacturers. If you’re using a specialty pharmacy, make sure they’re DSCSA-compliant and provide full transaction history. Don’t let convenience override compliance.
The Cost of Compliance - And the Cost of Cutting Corners
Yes, following these standards costs money. Independent pharmacies spend over 10% of their budget on compliance. Chain pharmacies? Around 6%. Hospitals with over 200 beds? Nearly all have full DSCSA systems in place. But what’s the alternative? A single counterfeit drug incident can cost millions - in fines, lawsuits, lost trust, and reputational damage.The FDA estimates 1% of the global drug supply is counterfeit. That might sound small, but it’s enough to kill. In 2022, the Health Resources and Services Administration (HRSA) found $1.3 billion in non-compliant purchases under the 340B program alone. That’s not just a number - it’s patients getting the wrong medicine because someone skipped a step.
Technology Is Changing the Game - But It’s Not a Fix-All
Blockchain, AI, and automated traceability platforms are coming fast. By 2025, 73% of health systems plan to use blockchain for drug verification. AI tools can now flag suspicious patterns in supply chain data - like a sudden spike in orders from an unknown distributor - before a single pill is received. These tools help, but they’re only as good as the data feeding them. If your supplier still sends paper forms or doesn’t scan barcodes, your AI won’t save you.And here’s the hard truth: technology doesn’t replace human judgment. You still need trained staff who know what to look for. One pharmacy in Wisconsin saved $120,000 in a year by catching a supplier falsifying expiration dates - not because their system flagged it, but because their pharmacist noticed the lot numbers didn’t match the manufacturer’s format.
Who’s Responsible? The CPO and the Frontline Pharmacist
In large hospitals, a Chief Pharmacy Officer (CPO) oversees procurement. By 2023, 92% of academic medical centers had one. But in small pharmacies? The owner or lead pharmacist is it. That means you’re responsible for knowing the rules, training your staff, auditing suppliers, and making the tough calls when something doesn’t add up.There’s no shortcut. Training takes about 120 hours to cover DSCSA, cGMP, state laws, and verification protocols. Certification through the Healthcare Supply Chain Association (CHCSCP) isn’t required - but it’s the gold standard. If you’re not investing in training, you’re gambling with patient safety.
What Happens When You Fail?
Fines? Yes. But worse - loss of license. The FDA can shut down a pharmacy for repeated violations. State boards can revoke your registration. Insurance companies may drop you. Patients will leave. And if someone is harmed? You could face criminal charges.In 2022, a small pharmacy in Florida was fined $500,000 and lost its license after distributing counterfeit blood pressure medication. The supplier claimed they were “authorized.” They weren’t. The pharmacist didn’t check. The patient died.
That’s the real cost of cutting corners.
Where to Start - A Practical Checklist
If you’re overwhelmed, start here:- Verify every supplier’s FDA registration and state license - on the official FDA and state board websites.
- Require written proof of DSCSA compliance - no verbal assurances.
- Implement barcode scanning for every incoming shipment.
- Use digital temperature monitors for refrigerated drugs.
- Keep transaction records for at least six years.
- Train your team on the seven ASHP supplier criteria.
- Never accept drugs from patients, unknown online sellers, or foreign sources without full documentation.
One pharmacy in New Zealand, following similar standards, reduced procurement errors by 80% in 18 months by doing just these seven things. You don’t need fancy software. You need discipline.
Final Thought: It’s Not About Rules - It’s About Trust
Patients trust you with their lives. That trust isn’t built on low prices or fast service. It’s built on knowing their medicine is safe. Every time you verify a lot number, every time you reject a suspicious shipment, every time you ask for documentation - you’re not just following a rule. You’re protecting someone’s life.The system isn’t perfect. Counterfeiters adapt. Regulations change. But the standard hasn’t: if you can’t trace it, you can’t trust it. And if you can’t trust it - don’t dispense it.
What happens if a pharmacy can’t prove DSCSA compliance?
If a pharmacy can’t prove DSCSA compliance, regulators can issue fines, suspend or revoke the pharmacy’s license, and require mandatory audits. In severe cases, the FDA can initiate criminal investigations. Pharmacies that fail to trace prescription drugs through the supply chain risk being shut down, especially if counterfeit or unsafe drugs are found on their shelves.
Can a pharmacy buy drugs from international suppliers?
Technically, yes - but only if the supplier is FDA-registered, complies with U.S. cGMP standards, and provides full DSCSA transaction data. Most international suppliers, especially those outside the U.S., EU, Canada, or Australia, don’t meet these requirements. Buying from them increases the risk of counterfeit drugs and violates federal law. The FDA actively blocks and seizes drugs imported without proper documentation.
How often should pharmacies audit their suppliers?
Pharmacies should conduct full supplier audits at least once a year, with spot checks every quarter. This includes verifying licenses, reviewing recall history, confirming DSCSA data flow, and checking financial stability. Suppliers with a history of issues should be audited twice a year. Waiting longer than a year is a major compliance risk.
Is it safe to use group purchasing organizations (GPOs) for drug sourcing?
Yes - and it’s strongly recommended. GPOs with dedicated pharmaceutical compliance teams pre-vet suppliers and handle DSCSA documentation, reducing the burden on individual pharmacies. Hospitals using GPOs reported 89% fewer supply chain security incidents in 2022 compared to those managing procurement independently. For small pharmacies, using a reputable GPO is one of the most effective ways to ensure compliance.
What’s the difference between 503A and 503B compounding pharmacies?
503A pharmacies are traditional compounding pharmacies that make custom medications for individual patients under a prescription. 503B outsourcing facilities produce larger batches of sterile drugs for hospitals and clinics, and must follow stricter FDA cGMP standards. Legitimate procurement requires knowing which type you’re buying from - 503B facilities must be registered with the FDA and are subject to inspections, while 503A facilities are regulated by states and have different rules.
How do I know if a drug is counterfeit?
Signs include mismatched packaging, spelling errors, unusual color or smell, missing lot numbers, or inconsistent tablet markings. But many counterfeits look perfect. The only reliable way is to verify the National Drug Code (NDC), lot number, and expiration date against the manufacturer’s database and confirm the transaction history through DSCSA-compliant systems. If anything doesn’t match, quarantine the product and report it to the FDA.
Are generic drugs more likely to be counterfeit?
No - counterfeit drugs target high-demand, high-margin products, regardless of whether they’re brand-name or generic. However, because generics are often sourced from multiple suppliers, especially overseas, the risk of encountering a fraudulent vendor increases if procurement isn’t tightly controlled. The key isn’t the drug type - it’s whether the supplier is verified and the supply chain is traceable.
What should I do if I suspect a drug is counterfeit?
Immediately quarantine the product. Do not dispense it. Contact your supplier for an explanation and request full documentation. If they can’t provide it, report the incident to the FDA’s MedWatch program and your state pharmacy board. Keep all packaging and records. The FDA uses these reports to track counterfeit trends and take enforcement action.
Next Steps for Pharmacies
If you’re a small pharmacy owner: start with the seven ASHP supplier criteria. Call your top three suppliers and ask for their FDA registration number and DSCSA compliance statement. Verify them yourself online. If they hesitate - that’s your answer.If you’re part of a hospital system: ensure your ERP and traceability systems are talking to each other. Only 35% of health systems have seamless integration - fix that before the next audit.
If you’re a regulator or policy maker: push for standardized data formats across all suppliers. The current patchwork of systems is what counterfeiters exploit.
Legitimate drug procurement isn’t about perfection. It’s about consistency. One step. One check. One verified lot number at a time. That’s how you stop counterfeit drugs - not with technology alone, but with people who refuse to cut corners.








15 Comments
Erin Nemo
Nov 30 2025This is so real. I work at a small pharmacy and we just got audited. We passed because we scan everything. No excuses.
ariel nicholas
Dec 1 2025The FDA? The DSCSA? Who even are these people? We used to just order from whoever had the best price-and we didn’t die! People are dying from iPhones, not pills! Why are we letting bureaucrats dictate medicine??
Kelly Essenpreis
Dec 1 2025All this paperwork and no one cares if the drug works. I’ve seen generics from India that cured my aunt’s diabetes better than the $500 brand name. Stop pretending compliance equals safety
Alexander Williams
Dec 3 2025The operationalization of DSCSA-compliant traceability infrastructure remains under-optimized across SMBs due to legacy ERP fragmentation and non-standardized API ontologies. The regulatory burden is non-trivial without interoperable data layering.
Suzanne Mollaneda Padin
Dec 3 2025I’ve trained pharmacy staff in 12 states. The biggest win? When a tech catches a mismatched lot number because they were trained to look. It’s not tech-it’s culture. Start there.
Rachel Stanton
Dec 3 2025For anyone overwhelmed: pick one thing. Just one. Maybe start with verifying FDA registration on the website. Do it for your top supplier this week. Then next week, do another. Progress > perfection.
Amber-Lynn Quinata
Dec 4 2025I’m so mad. I found a pill bottle with a typo on the label and no one cared. 🤬 Patients are dying because we’re too lazy to check. This isn’t just policy-it’s moral failure. 😔
amit kuamr
Dec 6 2025In India we get drugs from local manufacturers without any of this paper. No one dies. You Americans overthink everything. Just trust the doctor and move on
James Allen
Dec 7 2025I used to work at a chain. One time we got a shipment of insulin that was 2 degrees too warm. The manager said, 'eh, it’s fine, it’s just one batch.' I quit that day. This isn’t about rules-it’s about who you are when no one’s watching.
Kenny Leow
Dec 8 2025The global supply chain is complex. While U.S. regulations are rigorous, they are not universally applicable. International pharmacies operate under different frameworks. Respect for local systems is essential.
Lauryn Smith
Dec 8 2025I know a pharmacist who caught a fake blood pressure med because the bottle felt too light. She didn’t have fancy tech. Just sharp eyes and courage. You don’t need a degree to do the right thing.
Bonnie Youn
Dec 9 2025YES YES YES. This is the stuff we need to hear. Stop being scared of the work. Start doing the work. One scan. One call. One verification. You’re saving lives. I believe in you 💪
Edward Hyde
Dec 9 2025Let’s be real-this whole system is a cash grab for consultants and software vendors. You think the guy who wrote the DSCSA rules actually ever worked a pharmacy shift? Nah. He’s sipping margaritas in D.C.
Charlotte Collins
Dec 10 2025The irony? The same pharmacies that scream about 'regulation' are the ones that skip temperature logs and accept expired stock. You don't want rules-you want to be lazy and not get caught.
Margaret Stearns
Dec 11 2025i just started my first pharmacy job and this post helped me so much. i was scared to ask questions but now i know to always check the lot number. thank you