Switching to generic immunosuppressants can save transplant patients thousands each year, but for some, it’s a dangerous gamble. When doctors switch patients from brand-name drugs to generics, the risks aren’t just theoretical-they can mean rejection, hospital stays, or even losing a transplanted organ. This isn’t about fear-it’s about understanding the real-world challenges of bioequivalence in life-saving medications.
What are cyclosporine and tacrolimus?
Cyclosporine is a calcineurin inhibitor immunosuppressant discovered in 1971 from the fungus Tolypocladium inflatum. It received FDA approval in 1983 and was the first major drug to prevent organ rejection. Cyclosporine works by blocking T-cell activation, stopping the immune system from attacking transplanted organs.
Tacrolimus (also called FK506) was isolated in 1984 from Streptomyces tsukubaensis. It gained FDA approval in 1994 and has since become the preferred choice for most transplant centers. Tacrolimus suppresses immune responses more effectively than cyclosporine but requires careful monitoring due to its narrow therapeutic window.
Both drugs belong to the calcineurin inhibitors class of drugs that block the calcineurin enzyme to prevent immune system overactivity.. Yet their differences matter greatly. Tacrolimus works at 20 to 100 times lower concentrations than cyclosporine. A typical tacrolimus dose is 5 mg twice daily, while cyclosporine requires about 150 mg twice daily. This affects how doctors monitor patients. Tacrolimus blood levels must stay between 5-15 ng/ml in the first few months after transplant, while cyclosporine levels need to be 100-200 ng/ml. Getting these levels wrong can trigger rejection or toxicity.
Why generics matter-and why they’re tricky
Generic versions of cyclosporine and tacrolimus cut costs significantly. Brand-name tacrolimus (Prograf) costs $1,200-$1,500 monthly, while generics run $300-$500. Cyclosporine brand (Neoral) is $800-$1,000, with generics at $150-$300. For patients without insurance, this savings is life-changing. But bioequivalence the measure of how consistently a generic drug absorbs into the body compared to the brand isn’t always perfect. The FDA requires generics to stay within 80-125% of the brand’s absorption, but real-world data shows some variations exceed this range.
For cyclosporine, formulation differences cause major issues. Older Sandimmune formulations used oil-based delivery, while newer microemulsion versions (like Neoral) use water-soluble technology. Generic manufacturers vary in their methods-some use oil-based, others microemulsion. A 2022 study found switching between generic cyclosporine brands could cause blood levels to drop by 30%, enough to trigger rejection. Tacrolimus generics face similar challenges. Even small changes in absorption can push levels outside the safe range.
Real-world stories: when generics go wrong
On Reddit’s r/transplant community, user u/KidneyWarrior shared: “Switched from brand Prograf to generic tacrolimus. My levels dropped from 8.5 to 5.2 ng/ml in two weeks, leading to a mild rejection episode that required hospitalization.” Another user, u/OrganRecipient99, noted: “My nephrologist refuses to let me switch to generic cyclosporine because my levels were too unstable with the first generic version we tried.”
A 2022 survey by the American Society of Transplantation found 42.7% of 1,247 transplant recipients reported side effect changes after switching to generic tacrolimus. Eighteen percent experienced level instability requiring dose adjustments. The United States Renal Data System shows medication non-adherence rates are 15.3% higher among patients using generics versus brand-name drugs. Yet there are success stories too. One HealthUnlocked user wrote: “My insurance forced me to switch to generic tacrolimus, but my levels have been stable for 18 months with no issues-saved me $900 monthly.”

How to stay safe when switching generics
Transplant centers now follow strict protocols when switching between generic versions. The American College of Clinical Pharmacy recommends weekly blood tests for the first month after any switch. Many centers require 4-6 weeks of intensified monitoring. Patients should:
- Maintain consistent dosing times (within 1-hour windows)
- Avoid grapefruit products, which interfere with drug metabolism
- Use the same generic manufacturer consistently
- Report any new symptoms immediately to their transplant team
Pharmacists also play a key role. A 2023 Pharmacoepidemiology and Drug Safety analysis found only 41.7% of generic manufacturers provide detailed bioequivalence study data to clinicians.. Patients should ask their pharmacist about the specific generic brand they’re receiving and request the manufacturer’s name.
Current trends and solutions
In 2023, Astellas Pharma received FDA approval for a new extended-release tacrolimus formulation (LCP-tacrolimus) designed to minimize peak-trough fluctuations. This could reduce substitution issues. The European Medicines Agency issued updated guidelines in February 2024 requiring additional bioequivalence studies using actual transplant patients-not healthy volunteers. This change addresses a major flaw in previous testing.
Transplant centers increasingly use “single generic source” contracts to avoid switching between manufacturers. By 2023, 67.4% of major transplant programs adopted this approach. The International Transplant Society’s 2024 position statement emphasizes: “While generic immunosuppressants provide essential cost savings, their narrow therapeutic index requires individualized management strategies and avoidance of unnecessary interchanging between different generic products.”

Therapeutic Drug Monitoring: Your Safety Net
Therapeutic Drug Monitoring is the process of measuring drug levels in blood to ensure they stay within safe ranges. For tacrolimus, this means checking levels every 1-2 weeks after transplant, then monthly once stable. Cyclosporine requires more frequent checks due to higher variability. Levels outside the target range can cause rejection (too low) or kidney damage (too high). A 2021 study showed patients with consistent monitoring had 63% fewer rejection episodes compared to those without regular checks.
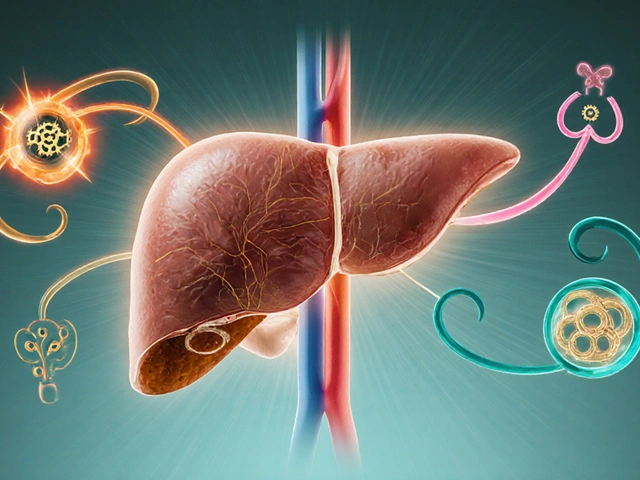
Genetic testing for CYP3A4 Metabolism a liver enzyme that processes these drugs is becoming standard. Variations in this gene affect how quickly the body breaks down tacrolimus. Patients with certain genetic markers need lower doses to avoid toxicity. This personalized approach helps stabilize levels without constant dose adjustments.
Frequently Asked Questions
Can I switch between different generic brands of tacrolimus?
Generally, no. Switching between generic brands without medical supervision can cause dangerous fluctuations in drug levels. The European Medicines Agency warns that “switching between different generic tacrolimus products without appropriate monitoring may result in subtherapeutic or supratherapeutic concentrations, potentially leading to rejection or toxicity.” Always consult your transplant team before changing manufacturers.
How often should I check my drug levels after switching to a generic?
You’ll need weekly blood tests for the first month after switching. After that, if levels stabilize, checks may reduce to biweekly or monthly. Your transplant team will tailor this based on your specific situation. Skipping tests during this period is risky-many rejection episodes occur because patients stopped monitoring too soon.
Are brand-name immunosuppressants safer than generics?
Not necessarily. Both brand-name and generic versions must meet strict FDA standards for safety and efficacy. However, generic versions can vary between manufacturers, and some have shown inconsistent absorption. If your current generic works well and your levels are stable, there’s no need to switch. But if you notice new symptoms or unstable levels, your doctor may recommend switching to a different generic or the brand-name drug.
Why do some doctors refuse to let patients switch to generics?
Doctors often avoid switching patients to generics if the patient has a history of unstable drug levels or prior rejection episodes. Cyclosporine, in particular, has higher variability between generic formulations. A 2023 study found 32% of transplant patients experienced level fluctuations when switching cyclosporine generics. If your doctor says no, it’s based on your specific medical history-not a blanket policy.
What should I do if I experience side effects after switching to a generic?
Contact your transplant team immediately. Symptoms like fever, unusual fatigue, swelling, or changes in urine output could signal rejection or toxicity. Do not stop taking your medication without medical advice. Your doctor will likely order blood tests to check drug levels and may adjust your dose or switch back to a different brand. Reporting side effects to the FDA’s MedWatch program also helps improve drug safety data.





10 Comments
Carol Woulfe
Feb 5 2026For years now, I've been watching the FDA and Big Pharma push these generic immunosuppressants on transplant patients.
The bioequivalence standards are a joke-they allow up to 25% variation in absorption.
For drugs like tacrolimus, which have a narrow therapeutic window, that's a death sentence.
The real reason they're pushing generics is to save money for insurance companies and hospitals.
Patients are being used as guinea pigs.
It's not just about cost-cutting; it's a deliberate strategy to harm vulnerable populations.
They know the risks, but they don't care because the profits are too high.
The FDA's approval process is completely broken.
They don't test these generics on actual transplant patients-they use healthy volunteers, which is irrelevant.
This is why so many people end up with rejection episodes.
It's all about corporate greed, and the government is in on it.
I've been saying this for years, but no one listens.
The system is rigged against patients.
We need to demand real change, not just more dangerous generics.
Every single transplant patient I know has had issues with generics.
It's not coincidence-it's a systematic failure.
The FDA's guidelines are written by people who have ties to pharmaceutical companies.
They're not looking out for patients; they're protecting the bottom line.
This has to stop.
Kieran Griffiths
Feb 7 2026Switching to generics can be safe if done carefully. Always work closely with your transplant team and get regular blood tests. Consistency is key-stick to the same generic brand and avoid switching between manufacturers. If you notice any new symptoms, contact your doctor immediately. Many patients have successfully transitioned to generics without issues when monitored properly. It's important to stay informed but not panic. Your medical team is there to help you navigate this safely.
Lisa Scott
Feb 7 2026Bioequivalence is a myth and FDA is complicit in patient harm.
Brendan Ferguson
Feb 7 2026While generics do save money, the key is proper management. Transplant centers now have strict protocols for switching-weekly blood tests for the first month, consistent dosing times, avoiding grapefruit. Many studies show that with careful monitoring, generics work just fine. The real issue is inconsistent switching between different generic brands. If you're stable on a particular generic, don't switch unless necessary. Always communicate with your pharmacist and doctor about which brand you're getting. It's not about brand vs generic-it's about consistency and monitoring.
Phoebe Norman
Feb 8 2026Consistency is paramount for narrow therapeutic index drugs like tacrolimus Variability in absorption can lead to subtherapeutic or supratherapeutic levels Without rigorous monitoring adverse events are inevitable The system is flawed
anjar maike
Feb 8 2026Switching to generics saves money but requires careful monitoring 😊 Regular blood tests are crucial Consistency in brand helps avoid issues Stay informed and work with your doctor 💡
Bella Cullen
Feb 9 2026Generics are dangerous for transplant patients.
Cullen Bausman
Feb 10 2026American generics are the safest-FDA oversight is unmatched.
Tehya Wilson
Feb 11 2026Generic immunosuppressants present significant risks due to bioequivalence inconsistencies The regulatory framework is inadequate Patient safety is compromised More rigorous testing is required
Albert Lua
Feb 13 2026In Europe the EMA has updated guidelines requiring testing on actual transplant patients This is a step forward Different countries have different approaches but collaboration is key Global standards need to improve for patient safety