What Glaucoma Really Is
Glaucoma isn’t just high eye pressure. It’s damage to the optic nerve - the cable that sends visual signals from your eye to your brain. That damage happens slowly, often without warning. By the time you notice vision loss, it’s usually too late to reverse it. This is why glaucoma is the second leading cause of blindness worldwide, affecting 76 million people today - and that number is expected to jump to over 110 million by 2040.
For decades, doctors thought glaucoma was simply about pressure inside the eye. But modern research shows it’s more complex. Yes, high pressure (called intraocular pressure, or IOP) plays a big role. But some people with normal pressure still lose vision. Others with pressure above 30 mmHg never develop damage. So what’s really going on?
How Eye Pressure Damages the Optic Nerve
Your eye makes fluid constantly. That fluid needs to drain out, just like water through a sink. When drainage gets blocked - even slightly - pressure builds up inside the eye. Normal IOP ranges from 10 to 21 mmHg. Anything above that is considered elevated.
That pressure pushes against the back of the eye, specifically the optic nerve head. There’s a mesh-like structure there called the lamina cribrosa. Think of it like a sieve holding the nerve fibers together. When pressure rises, this sieve bends and stretches. Studies using advanced imaging show that in glaucoma patients, this structure moves up to 50% more than in healthy eyes.
That movement crushes the tiny nerve fibers (axons) that carry your vision. Over time, those fibers die. The cells that support them - astrocytes, microglia, blood vessels - also break down. The result? Blind spots in your vision. These start on the edges and creep inward. You won’t feel it. You won’t notice it. That’s why glaucoma is called the "silent thief of sight."
Not All Glaucoma Is the Same
There are different types, and they behave differently.
- Primary Open-Angle Glaucoma (POAG) is the most common - about 90% of cases in the U.S. The drainage angle of the eye looks normal, but fluid drains too slowly. Pressure builds gradually.
- Normal-Tension Glaucoma (NTG) affects people with IOP under 21 mmHg. Yet their optic nerves still get damaged. Why? Research shows these patients often have lower pressure in their brain (intracranial pressure). The difference between eye pressure and brain pressure - called translaminar pressure - may be the real culprit. If that gap is over 20 mmHg, damage risk spikes.
- Angle-Closure Glaucoma is less common globally but causes half of all glaucoma blindness in Asia. Here, the iris blocks the drainage angle suddenly. Pressure rises fast. Symptoms can include eye pain, blurred vision, nausea. This is a medical emergency.
- Secondary Glaucoma comes from other causes: eye injuries, inflammation, steroids, or tumors. It’s aggressive and often harder to treat.
How Doctors Detect It Early
Since symptoms don’t show up until it’s advanced, screening is everything.
Eye doctors use three main tools:
- Eye pressure test (tonometry) - The gold standard is Goldmann applanation tonometry. It gently flattens part of the cornea to measure pressure. Normal is 10-21 mmHg. But pressure changes during the day. Peak levels often happen between 6 and 8 a.m.
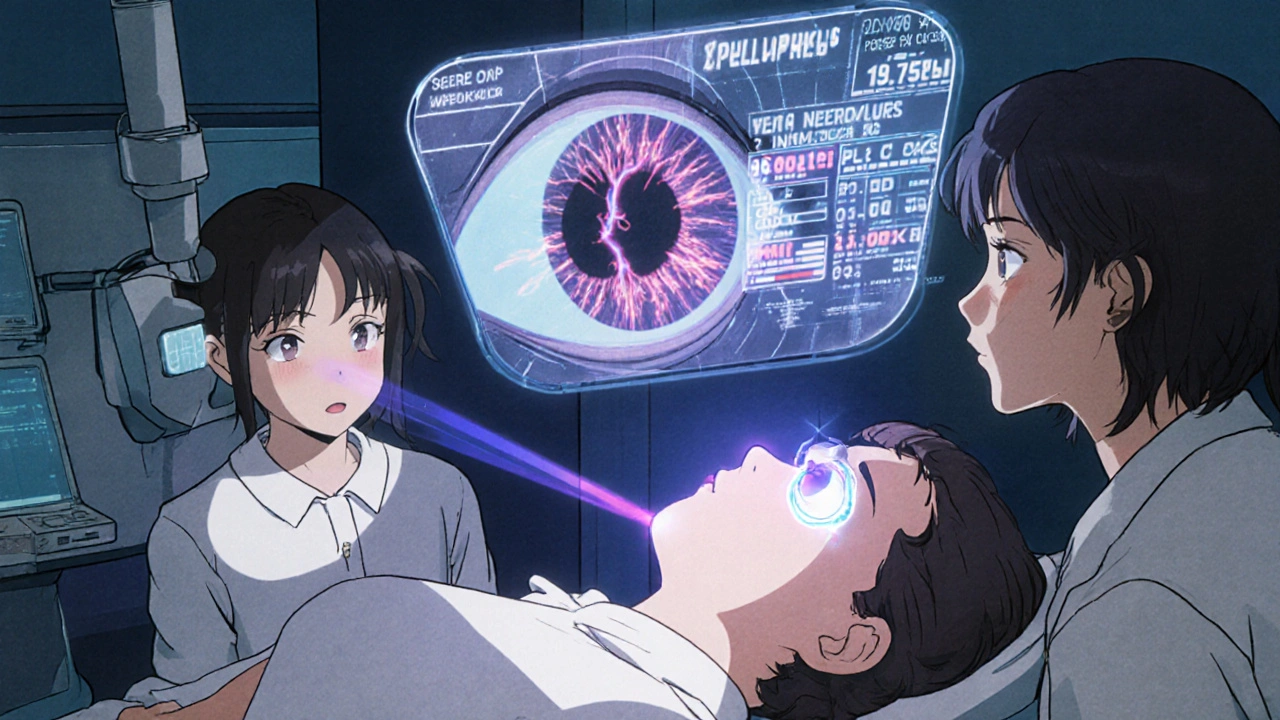
- Optic nerve imaging (OCT) - Optical coherence tomography takes a 3D scan of the retina. It can detect thinning of the nerve fiber layer as small as 5 microns - way before you lose vision. This is the most sensitive early warning tool.
- Visual field test - You sit in front of a machine and press a button when you see flashes of light. It maps out blind spots. Losses as small as 1 dB can signal early damage.
These tests are done regularly. For someone diagnosed with glaucoma, doctors typically check pressure every 3-6 months, do an OCT scan every 6-12 months, and repeat visual field tests once a year.
Treatment: Lowering Pressure, Saving Vision
The goal isn’t to cure glaucoma. It’s to stop it from getting worse. And the best way to do that? Lower eye pressure.
Studies show reducing IOP by 20-30% cuts progression risk by about half. The Early Manifest Glaucoma Trial proved this. So does the Collaborative Normal Tension Glaucoma Study - even when pressure was already normal, cutting it by 30% slowed damage.
First-line treatment? Eye drops. Prostaglandin analogs like latanoprost are the most effective. They lower pressure by 25-33% with just one drop a day. But they come with side effects: longer eyelashes, darker eyelids, and sometimes sunken eyes from fat loss around the orbit. About 1 in 5 people stop using them because of this.
If drops don’t work enough, doctors turn to laser treatment. Selective laser trabeculoplasty (SLT) opens up drainage channels. It works in 75% of people, but its effect fades over time - about 10% per year.
Surgery is next. Trabeculectomy creates a new drainage path. It’s successful in 85-90% of cases after one year. But it’s invasive. Minimally Invasive Glaucoma Surgery (MIGS), like iStent, is becoming popular. It’s safer, with fewer complications, and reduces pressure by 20-25%. Success lasts at least two years in 70-80% of cases.
Why People Stop Taking Their Meds
Here’s the hard truth: half of glaucoma patients stop their eye drops within a year. Only one in four still uses them after two years.
Why? Side effects. Forgetting. Cost. And denial. Many patients don’t feel sick, so they think they’re fine. A 2022 survey of 1,200 patients found 68% lived in fear of going blind - yet still skipped doses.
One Reddit user wrote: "My IOP is always under 15. Why is my vision still getting worse?" That’s NTG. Pressure isn’t the whole story. That’s why some patients need more than drops - they need regular imaging to track nerve thinning, even if pressure looks good.
On the flip side, others find relief. One patient on Glaucoma.org shared: "After surgery, my pressure dropped from 32 to 14. My vision hasn’t changed in 10 years."
The Future: Beyond Pressure
Researchers are no longer just focused on lowering pressure. They’re trying to protect the nerve itself.
One promising area: neuroprotection. The drug brimonidine, already used for pressure control, appears to have a second effect - it may directly protect nerve cells. In the LIBERTI study, NTG patients on brimonidine had 30% slower vision loss than those on timolol - even though both lowered pressure equally.
Other experiments are even more exciting. Oncomodulin, a natural growth factor, triggered 40% regeneration of damaged nerve fibers in animal models. CNTF implants showed 2.5 dB better visual field preservation after two years. Gene therapy targeting the eye’s drainage system has already reduced pressure by 25% in early human trials.
Stem cell therapies are being tested to rebuild the optic nerve. Home monitoring devices, like the Triggerfish contact lens, track pressure 24/7. AI tools can now spot early glaucoma in OCT scans with 94% accuracy - better than many human graders.
What You Can Do
If you’re over 40, get your eyes checked - even if you see fine. Glaucoma doesn’t care if you’re healthy, active, or young. It doesn’t cause pain. It doesn’t ask permission.
Know your family history. Glaucoma runs in families. If a parent or sibling has it, your risk doubles.
Stick to your treatment. Even if your pressure seems normal, don’t skip drops. Don’t skip follow-ups. Your vision is being monitored at a microscopic level. Tiny changes matter.
And if you’ve been told you have "elevated pressure" but no damage yet - don’t panic. That’s ocular hypertension. Not everyone with high pressure develops glaucoma. But you need regular checkups. Your doctor will watch your optic nerve closely.
Final Thought
Glaucoma isn’t a death sentence. But it’s not something you can ignore. With early detection and consistent treatment, most people keep their vision for life. The key isn’t perfection - it’s persistence. Keep your appointments. Take your drops. Trust the process. Your eyes are watching you - even when you think they’re not.
Can glaucoma be cured?
No, glaucoma cannot be cured. Once nerve cells are lost, they don’t regenerate. But with early detection and consistent treatment - usually lowering eye pressure - progression can be stopped or dramatically slowed. Most people maintain useful vision for life if they follow their treatment plan.
Can you have glaucoma with normal eye pressure?
Yes. This is called normal-tension glaucoma (NTG). It accounts for 20-30% of cases in Western countries and up to 70% in parts of Asia. Damage occurs even when eye pressure is within the normal range (10-21 mmHg). The cause may be related to low pressure in the brain (intracranial pressure), making the pressure difference across the optic nerve too high. Regular imaging and visual field tests are critical for managing NTG.
How often should I get tested for glaucoma?
If you’re over 40 with no risk factors, get a comprehensive eye exam every 2-4 years. If you’re over 60, every 1-2 years. If you have a family history of glaucoma, diabetes, or high blood pressure, start screenings at 35 and get checked every 1-2 years. If you’ve been diagnosed, follow your doctor’s schedule - usually every 3-6 months for pressure checks, annual visual field tests, and OCT scans every 6-12 months.
Are eye drops for glaucoma safe long-term?
Yes, most glaucoma eye drops are safe for long-term use. Prostaglandin analogs like latanoprost are the most commonly prescribed and well-tolerated. Side effects - like darker eyelashes, eyelid skin darkening, or eye redness - are usually mild and cosmetic. Serious side effects are rare. The bigger risk is not using them. Skipping doses is the leading cause of vision loss in glaucoma patients.
Does lifestyle affect glaucoma?
Lifestyle doesn’t cause glaucoma, but it can influence its progression. Regular aerobic exercise (like brisk walking) can lower eye pressure by 10-20%. Avoid inverted yoga poses, which can raise pressure. Smoking increases oxidative stress and may worsen damage. A diet rich in leafy greens and omega-3s may support eye health, though no specific supplement prevents glaucoma. The most important thing? Stick to your prescribed treatment - not diet or vitamins.
Is glaucoma testing painful?
No. Eye pressure testing is quick and painless. A puff of air or a gentle touch with a probe (after numbing drops) is all that’s needed. Visual field tests take 15-30 minutes per eye and require focus, but there’s no discomfort. OCT scans are non-invasive - just sit and look at a light. There’s no radiation or needles involved.
Can glaucoma affect both eyes equally?
Usually, but not always. In most cases, glaucoma affects both eyes, but often one eye is worse than the other. This is why doctors test each eye separately. Even if one eye looks fine, the other may already be damaged. That’s why regular monitoring of both eyes is essential - even if symptoms seem to be in just one.




13 Comments
steve o'connor
Nov 23 2025I had no idea glaucoma could sneak up like this. My dad had it and we just thought he was getting old. Turns out he was losing vision for years before anyone noticed. Got my first OCT scan last month - thank god I went. Still have my full field of vision.
Don't wait until you 'feel' something. Just get checked.
ann smith
Nov 24 2025This is such an important post. 🙏 I work in primary care and see so many patients who skip eye exams because 'they see fine.' Glaucoma doesn't announce itself - it steals quietly. Please, if you're over 40, don't ignore this. Your future self will thank you.
Julie Pulvino
Nov 26 2025I'm on latanoprost and honestly? The eyelash thing is kinda cool. Like, I got free mascara. 😅 But the dark eyelids? Yeah, that’s a bummer. Still, I’d rather have dark lids than blind spots. My doc says my IOP’s down to 12 now - after 3 years of drops. Worth it.
Danny Nicholls
Nov 28 2025bro i had angle closure and it was scary as hell. one minute i’m fine, next minute my eye feels like it’s gonna explode, vision all blurry, nausea. rushed to ER, got laser iridotomy same day. now i’m fine but i tell everyone: if you’re asian and over 50, get checked. this isn’t a myth. it’s real. 🙏
Robin Johnson
Nov 30 2025Let’s cut the fluff. If you have glaucoma, you don’t get to choose whether to take drops. You either do it or you lose your vision. No exceptions. No 'I’ll do it tomorrow.' Your optic nerve doesn’t care how busy you are. Stop pretending this is optional.
Latonya Elarms-Radford
Nov 30 2025The tragedy of modern medicine is that we treat symptoms while ignoring the existential void between perception and reality. Glaucoma isn’t just a disease of pressure - it’s a metaphor for how we disconnect from the fragility of our own being. We live in a world that values productivity over presence, and so we ignore the silent erosion of our inner sight until the light is gone. And then? We blame the eye drops. But the real failure? We stopped listening to ourselves long before the pressure rose.
Mark Williams
Dec 2 2025The translaminar pressure gradient hypothesis is underappreciated in clinical practice. NTG patients with low ICP show significant axonal transport disruption due to differential stress across the lamina cribrosa. OCT metrics like RNFL thinning and GCC loss are more predictive than IOP alone. We need to shift from pressure-centric to neuro-structural monitoring protocols.
Ravi Kumar Gupta
Dec 2 2025In India, most people think eye problems = need for glasses. Glaucoma? They say 'it's just aging.' My uncle lost vision in one eye before anyone took him to a specialist. We need more awareness - especially in villages. I started sharing this post in my WhatsApp groups. If one person gets checked because of it, it’s worth it.
Rahul Kanakarajan
Dec 3 2025So you’re telling me I need to spend $200 on eye drops every month just because I have 'elevated pressure'? What if I’m just one of those people who naturally has high IOP but zero damage? Why not wait and see? You guys are just scared of losing patients. This whole thing feels like a money grab.
james lucas
Dec 5 2025i just found out i have ocular hypertension and honestly i was freaking out. but reading this made me feel way better. my doc said i dont need drops yet, just checkups every 6 months. i started using my phone reminder to get my eyes checked. also i walk 30 min a day now. small stuff but feels good. thanks for the info!
Jessica Correa
Dec 7 2025I think the real issue is how disconnected we are from our bodies until something breaks. I used to skip eye exams because I didn't feel sick. Now I know it's not about feeling it. It's about seeing it before it's gone. I got my OCT last week. Still normal. I'm so grateful
manish chaturvedi
Dec 7 2025In my village in Uttar Pradesh, we used to believe that eye diseases were caused by bad karma. My cousin went blind from glaucoma because no one took her to a doctor. Now I teach my nieces and nephews: your eyes are not a gift you can ignore. Get checked. Even if you see fine. Even if you think you’re too young.
Nikhil Chaurasia
Dec 7 2025I appreciate this post. I’ve been managing NTG for 5 years. My pressure is always normal, but my nerve keeps thinning. I’ve learned to trust the scans more than my eyes. Sometimes, I feel like I’m living in a ghost town - my vision is still 'fine,' but I know the damage is happening. I just wish more doctors understood that.