Why waiting for memory lapses is too late
Most people think cognitive decline means forgetting names or where you left your keys. But by the time those moments become frequent enough to worry about, the brain has already been changing for years - sometimes decades. The real goal today isn’t to wait for confusion. It’s to catch the quiet signals before they turn into problems.
That’s why screening for Mild Cognitive Impairment (MCI) is no longer optional. It’s becoming part of routine care, especially for adults over 65. And the tools we use to find it? They’ve changed completely.
The old tests are falling behind
You’ve probably heard of the MMSE or MoCA - paper-and-pencil tests that ask you to draw a clock, remember three words, or count backward. These were the gold standard for years. But in 2026, doctors are moving away from them. Why? Because they’re too blunt.
Think of it like checking your blood pressure with a manual cuff instead of a digital monitor. Both can give a number, but only one catches subtle shifts over time. The MoCA, for example, might miss someone who’s slowly losing the ability to plan a meal or follow a conversation in a noisy room. These are the early signs - the ones that matter most when new treatments are available.
A 2023 meta-analysis showed traditional screeners only catch 71-90% of MCI cases. That means up to 3 in 10 people with early brain changes slip through. And if you’re one of them, you miss the window to act.
What’s replacing paper tests? Digital tools that see what humans can’t
The new wave of cognitive screening doesn’t ask you to remember words. It watches how you move, how long you pause, how your eyes track a moving object on a screen. These tools don’t just measure outcomes - they measure process.
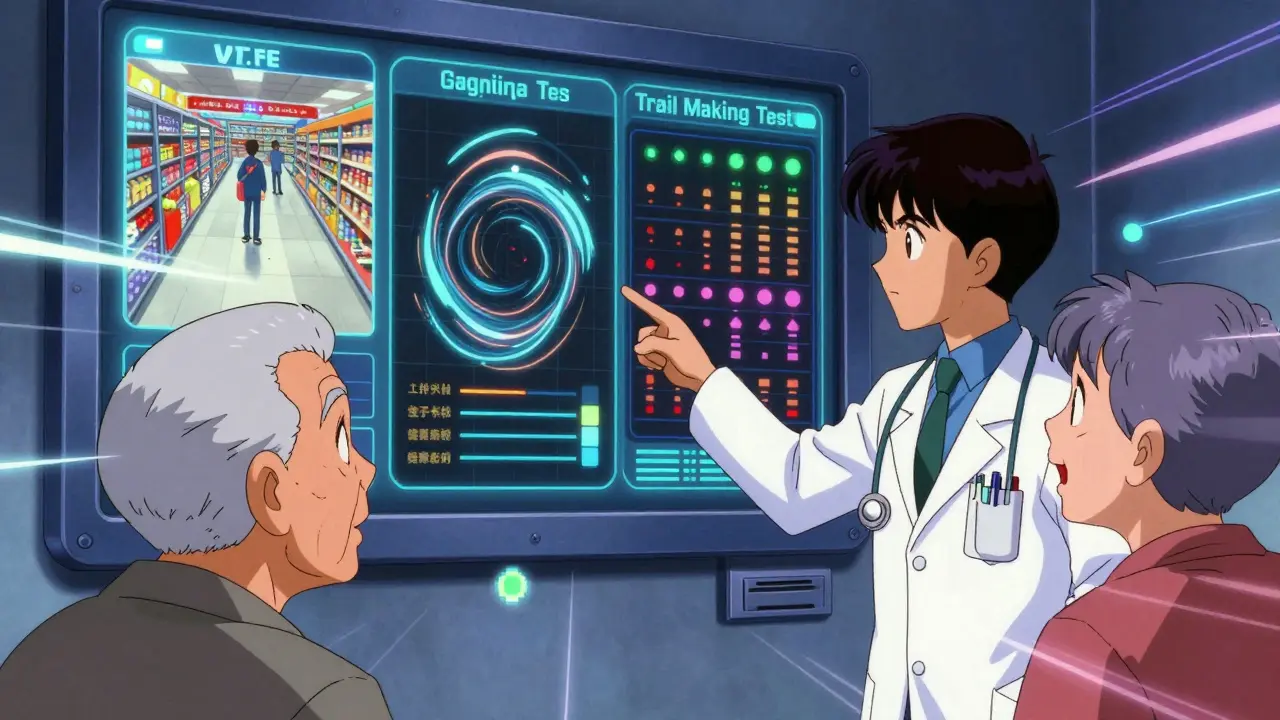
Take the digital Trail Making Test Part B (dTMT-B). Instead of just timing how fast you connect dots, it tracks your pen stroke speed, how often you hesitate, and even the smoothness of your lines. A person with early MCI might draw the same shape as someone healthy - but their movements are slightly slower, less fluid. That’s a clue traditional tests never saw.
Linus Health’s Digital Clock and Recall (DCR) and dTMT-B combo has been shown to detect MCI with 93.7% accuracy. Cleveland Clinic’s C3B tool, used during Medicare annual visits, correctly identified MCI 18.3% better than the Mini-Cog. And VR-E, a virtual reality test that uses eye-tracking while you watch a simulated grocery store scene, achieved a 94.15% accuracy rate in distinguishing normal aging from early MCI.
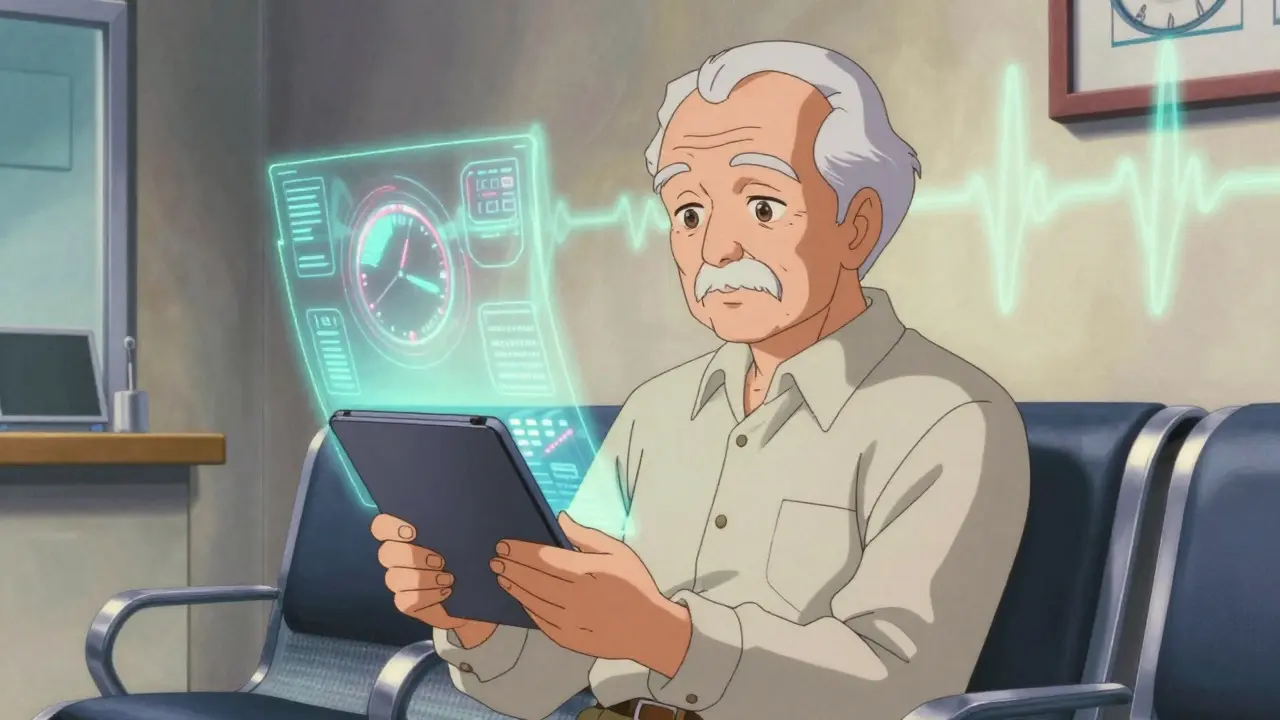
These aren’t science fiction. They’re being used right now in clinics across the U.S. and Europe. And they’re not just accurate - they’re fast. Most take under 10 minutes. Many can be done on a tablet while you wait to see your doctor.
Why this matters: New drugs need early detection
It’s not just about knowing. It’s about acting. In 2023 and 2024, the FDA approved the first disease-modifying drugs for Alzheimer’s - drugs like lecanemab and donanemab. These don’t cure dementia. But they can slow decline… if you start them early.
Studies show these drugs work best when amyloid plaques are just beginning to build up - years before symptoms appear. That’s why screening isn’t just helpful anymore. It’s essential. If you wait until someone is forgetting family members’ names, the damage is too advanced for these treatments to make a meaningful difference.
Dr. James Leverenz from Cleveland Clinic says it plainly: “Linking cognitive screening to the annual Medicare visit allows us to detect early concerning changes. In the new era of disease-modifying therapies… early detection is critically important for treatment success.”
Are these tools easy to use? Real user experiences
One big fear: “Will my parent or grandparent be able to use this?”
The answer? Most can. In Cleveland Clinic’s pilot program, 95% of patients said the digital test added value to their care. On Reddit, a caregiver wrote: “My mom’s 78 and not tech-savvy - she did the Linus Health test in the waiting room with no help.”
But it’s not perfect. Some older adults struggle with small buttons, confusing menus, or unfamiliar interfaces. One user on AgingCare.com shared: “My father failed the online test because he couldn’t figure out how to click - not because he was losing his mind.”
That’s why the best tools are designed with seniors in mind: large buttons, voice prompts, simple navigation, and no timers. Tools like RoCA and TabCAT-BHA were built with input from older users. And the good news? Smartphone use among Americans over 65 is now at 78%. Digital literacy is rising fast.
What’s next? Blood tests and AI
Screening isn’t just getting smarter - it’s getting cheaper. Right now, confirming Alzheimer’s risk often means an expensive PET scan or a spinal tap. But that’s changing.
Researchers are now using simple blood tests to detect proteins linked to Alzheimer’s - amyloid and tau. In early trials, these tests match the accuracy of brain scans. The National Institute on Aging says they’re “finally in reach.”
And the future? Combining digital cognitive tests with blood biomarkers. Linus Health already has a model that uses your clock-drawing pattern, your trail-making speed, and your APOE gene status to predict brain amyloid levels - almost as well as a PET scan. Imagine a single visit: 7 minutes on a tablet, a finger prick for blood, and a clear picture of your brain health.
Getting screened: What to ask your doctor
Don’t wait for your doctor to bring it up. Ask.
- “Do you screen for early cognitive changes during annual checkups?”
- “Are you using digital tools like C3B or Linus Health’s platform?”
- “If I’m concerned about memory, what’s the next step?”
If your doctor says they still use MoCA or MMSE, ask why. The evidence is clear: newer tools are more sensitive, faster, and better at tracking change over time.
Also check if your insurance covers it. Medicare now reimburses up to $45 per digital cognitive screening test. Many private insurers follow suit.
What if the test shows something concerning?
A positive screen doesn’t mean you have dementia. It means your brain is showing early signs of change - and you have time to act.
Next steps often include:
- Further testing: blood work, brain imaging, or genetic screening if appropriate
- Lifestyle changes: more physical activity, better sleep, managing blood pressure and diabetes
- Medications: if you’re eligible, disease-modifying drugs may be an option
- Planning: legal, financial, and care planning for the future
Early detection doesn’t mean panic. It means control. You’re not waiting for the storm - you’re preparing for it.
The big picture: Screening is becoming standard
By 2030, the global market for cognitive screening tools is expected to hit $4.87 billion. Why? Because the system is changing.
Health systems with 500+ beds are adopting these tools at more than double the rate of just two years ago. The American Medical Association now recommends starting with simple digital tools like DCR before moving to complex VR systems.
And the U.S. Preventive Services Task Force is reviewing its stance. They currently say evidence is insufficient - but their 2025 research plan shows they’re preparing to recommend routine screening. That’s coming.
For now, the choice is yours. You can wait for the next missed word or name. Or you can ask for a test today - one that might give you years of better brain health ahead.





14 Comments
owori patrick
Jan 30 2026I really appreciate how this post breaks down the tech in a way that doesn’t make older folks feel left out. My uncle in Lagos just did the Linus test on his tablet last week - no help needed. He said it felt like a game. That’s huge.
Claire Wiltshire
Jan 31 2026The shift from MoCA to digital tools is long overdue. As a geriatric nurse practitioner, I’ve seen too many patients miss early intervention windows because paper tests lack sensitivity. The dTMT-B and DCR tools aren’t just more accurate - they’re objectively better at capturing subtle motor-cognitive decoupling. Medicare reimbursement is a step in the right direction, but we need standardized training for clinicians too.
Darren Gormley
Feb 1 2026LMAO 😂 so now we’re diagnosing dementia by how someone draws a clock on a tablet? Next they’ll measure your brain health by how fast you swipe Tinder. This is what happens when tech bros get hold of medicine. Give me a real doctor and a conversation any day.
Mike Rose
Feb 3 2026bro why are we even doing all this? my grandma forgets where she put her dentures and they want to run blood tests and vr games? just give her a pill already.
Sheila Garfield
Feb 4 2026I think the real win here is how these tools normalize the conversation. My mom used to panic every time she mislaid her glasses - now she jokes about her 'digital brain checkup.' That shift from fear to agency? Priceless. And honestly, the fact that 95% of seniors in the Cleveland pilot found it helpful? That says more than any p-value.
Shawn Peck
Feb 5 2026YOU’RE ALL MISSING THE POINT. THESE TOOLS AREN’T FOR SENIORS - THEY’RE FOR THE HEALTHCARE INDUSTRY TO MAKE MONEY. THEY’RE PUSHING THIS BECAUSE PHARMA WANTS YOU TO BELIEVE YOU NEED A DRUG BEFORE YOU EVEN HAVE SYMPTOMS. THIS ISN’T HEALTHCARE - IT’S A SCAM.
Niamh Trihy
Feb 5 2026The blood biomarker research is genuinely exciting - especially the p-tau217 assays. They’re now showing >90% concordance with PET scans in preclinical trials. If this gets rolled out in primary care, we could cut diagnostic delays from 3 years to under 3 months. That’s transformative.
Jason Xin
Feb 7 2026I get the excitement about tech, but let’s not pretend this is magic. My dad did the VR grocery test - failed because he couldn’t tell the difference between milk and yogurt. Turned out he had cataracts. The machine didn’t know. The nurse did. Tech helps. It doesn’t replace human judgment.
KATHRYN JOHNSON
Feb 7 2026This is why America is falling behind. In the UK, we’ve had cognitive screening integrated into NHS annuals since 2022. We don’t need VR goggles or blood tests. We have trained nurses, proper protocols, and no corporate profit motive. This is American over-engineering at its worst.
kate jones
Feb 8 2026The APOE ε4 allele integration with digital phenotyping is the real frontier. Linus Health’s algorithm combining eye-tracking, motor kinetics, and polygenic risk scores achieves AUCs of 0.96 in validation cohorts. This isn’t screening - it’s predictive neurology. We’re entering an era where risk stratification precedes symptom onset.
Kelly Weinhold
Feb 10 2026I just want to say - if you’re reading this and you’re 60+, please don’t wait. My mom waited until she forgot my name. That wasn’t ‘just aging.’ It was MCI. She started on lecanemab last year. She still remembers my wedding day. That’s worth a 10-minute tablet test. Don’t be scared. Be proactive. You’ve got this 💪
Kimberly Reker
Feb 11 2026I work in a senior center. We’ve been using TabCAT-BHA for 6 months now. The staff love it - it’s fast, quiet, and doesn’t stress people out. One guy thought it was a crossword app and asked if he won a prize. We told him he won 20 more years of clarity. He cried. That’s the real win.
Eliana Botelho
Feb 12 2026Okay but why are we letting tech companies design medical tools? Who approved this? Who’s auditing the algorithms? What if the tablet thinks you’re declining because you’re tired? Or because you’re from a different culture? This feels like a beta test on my parents’ brains.
Rob Webber
Feb 12 2026I’ve seen the future of medicine. It’s not in tablets or blood tests. It’s in the silence between the words. The pause before a response. The hesitation when someone tries to recall their daughter’s name. No machine can measure that. Only a family member who’s been there for 40 years. Don’t outsource your love to an app.