Many people take anticholinergic medications without realizing they might be slowly harming their brain. These drugs are common - used for overactive bladder, allergies, depression, and even Parkinson’s - but their hidden costs are serious. If you or someone you know is on one of these medications long-term, especially over age 65, it’s worth asking: is the benefit worth the risk?
What Are Anticholinergics and How Do They Work?
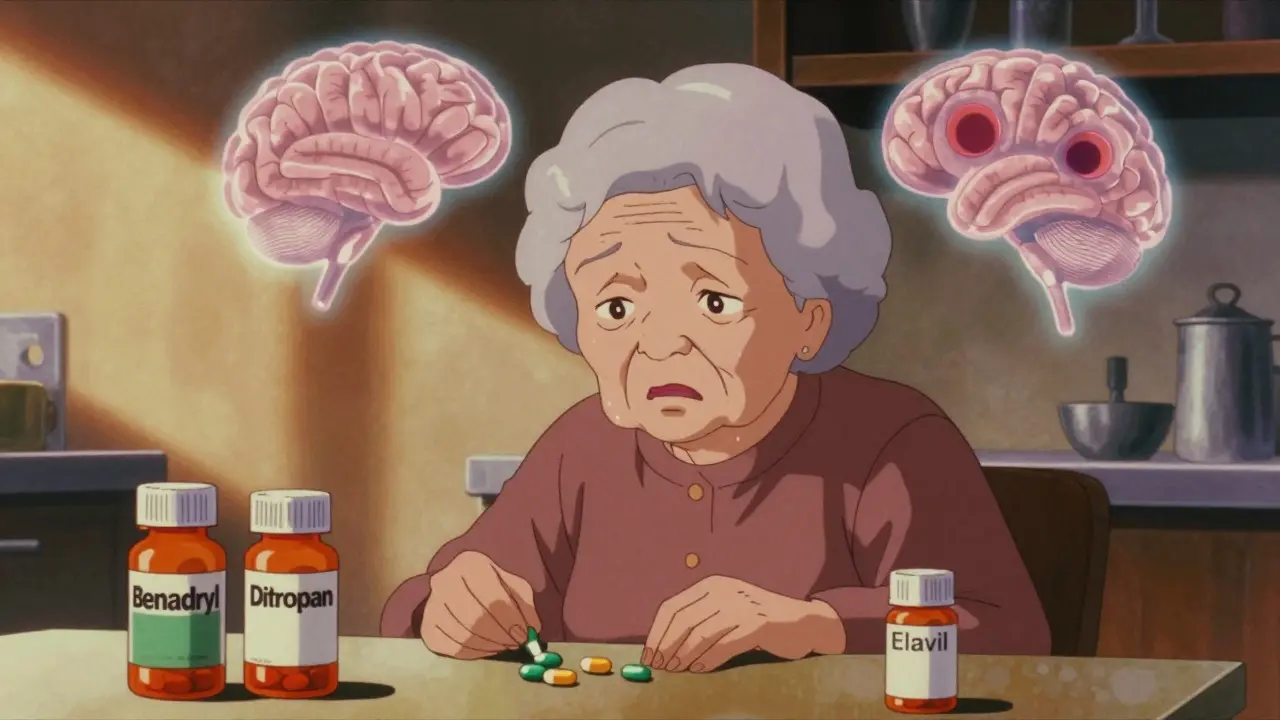
Anticholinergics block acetylcholine, a key brain chemical that helps with memory, attention, and muscle control. They’ve been around since the early 1900s, originally pulled from deadly nightshade plants. Today, they’re in dozens of pills you can buy over the counter or get by prescription.Common ones include diphenhydramine (Benadryl), oxybutynin (Ditropan), amitriptyline (Elavil), and trihexyphenidyl. Each works by attaching to muscarinic receptors in the body - especially M1 receptors in the brain, which are vital for forming memories and staying focused. When these receptors are blocked, the brain struggles to do its job.
That’s why you feel drowsy after taking Benadryl. That’s also why long-term use can lead to real, measurable brain changes.
The Cognitive Risks: More Than Just Forgetfulness
It’s not just about forgetting where you put your keys. Studies show that long-term anticholinergic use causes structural damage to the brain. People taking high-burden drugs (ACB score of 2 or 3) lose brain volume faster - up to 1.2% more per year than non-users. That’s like aging your brain an extra decade in just five years.Brain scans reveal smaller hippocampi, the area responsible for memory. Ventricles - fluid-filled spaces in the brain - become noticeably larger. Glucose metabolism drops by 8-14% in memory centers, meaning the brain isn’t getting the fuel it needs.
On cognitive tests, users perform 23-32% worse on memory recall and 18-27% worse on problem-solving tasks. These aren’t small dips. They’re the kind of changes doctors see in early dementia.
A 2015 study tracking over 48,000 people found that using anticholinergics for three or more years nearly doubles the risk of developing dementia. The American Geriatrics Society says this isn’t speculation - it’s fact. They’ve listed 56 anticholinergic drugs as potentially inappropriate for older adults.
Dry Mouth: The Most Common - and Misunderstood - Side Effect
Almost everyone on these drugs gets dry mouth. It’s not just uncomfortable - it’s a warning sign. Dry mouth happens because anticholinergics shut down saliva production. You’re not just thirsty; your mouth feels like cotton. Chewing, swallowing, even speaking becomes hard.On Drugs.com, 82% of users report severe dry mouth. One person wrote: "I drink three liters of water a day and still feel parched." Another said: "I can’t talk without clearing my throat every few seconds."
But dry mouth isn’t just a nuisance. It leads to dental decay, gum disease, and infections. Saliva protects your teeth and kills bacteria. Without it, your mouth becomes a breeding ground for problems that cost time, money, and pain.
Some people accept it as "just part of the pill." But that’s dangerous thinking. Dry mouth is your body screaming that something’s wrong - and it’s not just your mouth that’s affected.
Not All Anticholinergics Are Created Equal
Here’s the good news: you don’t have to take the worst ones. The Anticholinergic Cognitive Burden (ACB) scale rates drugs from 0 (no effect) to 3 (high risk). Many drugs with the same purpose have much lower scores.For example:
- High risk (ACB 3): Diphenhydramine, scopolamine, oxybutynin
- Moderate risk (ACB 2): Amitriptyline, tolterodine
- Low risk (ACB 1): Glycopyrrolate, trospium, darifenacin, tiotropium
Oxybutynin, a top choice for overactive bladder, has one of the highest ACB scores. Studies show it causes 28% more cognitive decline than tolterodine - a similar drug with half the brain impact.
And here’s the kicker: you don’t need anticholinergics at all for overactive bladder. Mirabegron, a beta-3 agonist, works just as well without touching your brain. It’s more expensive - $350 a month vs. $15 for generic oxybutynin - but it doesn’t fog your mind or dry out your mouth.
Who’s Most at Risk?
Older adults are the most vulnerable. About 25% of Americans over 65 take at least one anticholinergic. Many don’t realize it’s in their allergy pill, sleep aid, or stomach medicine. They’re taking multiple drugs with low ACB scores - and adding up to a dangerous total.One person might take Benadryl for allergies (ACB 3), amitriptyline for nerve pain (ACB 3), and oxybutynin for bladder control (ACB 3). That’s a total burden of 9 - the equivalent of taking a high-dose anticholinergic every day for years.
Even younger people aren’t safe. Long-term use of diphenhydramine for sleep can cause memory issues in people as young as 40. The damage builds slowly. By the time symptoms show up, the brain changes may already be permanent.
What Can You Do?
If you’re on an anticholinergic, don’t stop cold turkey. Talk to your doctor. Ask these questions:- What’s the ACB score of this drug?
- Is there a safer alternative - even if it costs more?
- Can I try non-drug options first? Like bladder training, pelvic floor therapy, or sleep hygiene?
- How long have I been on this? Is it still necessary?
For overactive bladder, behavioral therapy works as well as drugs for many people. For depression, SSRIs have far fewer brain effects than amitriptyline. For allergies, second-generation antihistamines like loratadine or cetirizine have almost no anticholinergic activity.
For dry mouth, try sugar-free gum or lozenges - they boost saliva by 30-40%. Prescription options like pilocarpine (5mg three times a day) can increase saliva by 50-70%. Don’t just suffer - ask for help.
The Bigger Picture: A System That Still Overprescribes
Only 32% of primary care doctors can correctly identify high-risk anticholinergics during patient visits. That’s not because they’re careless - it’s because the system doesn’t train them to look for it. Pharmacists often don’t flag these drugs either.But change is coming. The FDA now requires stronger warning labels on 12 high-risk drugs. NICE in the UK recommends deprescribing anticholinergics in 68% of older patients. Medicare prescriptions for oxybutynin dropped 32% between 2015 and 2022 as safer alternatives like mirabegron grew.
New drugs are being developed too. Trospium chloride XR has 70% less brain penetration than oxybutynin. Xanomeline, a new M1-selective drug, reduces dry mouth by 40% compared to older antipsychotics.
AI tools like MedAware are now scanning prescriptions in real time and alerting doctors when a patient is on too many anticholinergics. In five years, these tools could prevent hundreds of thousands of dementia cases.
Final Thoughts: Knowledge Is Power
Anticholinergics aren’t evil drugs. They help people with severe symptoms. But they’re not harmless. For millions, the trade-off is brain fog, dry mouth, and a higher chance of dementia - all for a condition that might be managed another way.If you’re on one of these medications, ask your doctor to review your list. Bring a copy of your pills. Ask for the ACB score. Ask about alternatives. Don’t assume the side effects are normal. They’re not.
Your memory matters. Your mouth matters. And you deserve to live without unnecessary risk.
Can anticholinergics cause dementia?
Yes. Long-term use - especially three or more years - doubles the risk of dementia, according to a major study of 48,000 people published in The BMJ. Brain scans show structural changes like shrinking hippocampi and larger ventricles in users. The American Geriatrics Society warns that these drugs should be avoided in older adults whenever possible.
Is dry mouth from anticholinergics dangerous?
Yes. Dry mouth isn’t just uncomfortable - it leads to tooth decay, gum disease, oral infections, and difficulty swallowing. Saliva protects your mouth from bacteria and helps digest food. Without it, your dental health declines fast. Use sugar-free gum, saliva substitutes like Xerolube, or prescription pilocarpine to manage it.
Are there anticholinergics that don’t affect the brain?
Yes. Drugs like glycopyrrolate, trospium, darifenacin, tiotropium, and ipratropium have low ACB scores (1) and show no significant cognitive decline in studies. For overactive bladder, mirabegron is a non-anticholinergic option with equal effectiveness and no brain side effects.
Can I stop taking anticholinergics on my own?
No. Stopping suddenly can cause dangerous rebound symptoms - especially for Parkinson’s or severe depression. Always talk to your doctor. They can help you taper off safely or switch to a lower-risk alternative.
How do I know if my medication has anticholinergic effects?
Check the ACB scale. Common high-risk drugs include diphenhydramine (Benadryl), oxybutynin, amitriptyline, and scopolamine. You can also ask your pharmacist or use free online tools like the Anticholinergic Cognitive Burden Calculator from the University of Michigan. Look for terms like "anticholinergic," "antimuscarinic," or "blocks acetylcholine" on the label.
What’s the best alternative to oxybutynin for overactive bladder?
Mirabegron (Myrbetriq) is the top alternative. It works differently - by relaxing the bladder muscle - and has no anticholinergic effects. Clinical trials show it’s just as effective as oxybutynin at reducing incontinence, but without memory loss or dry mouth. Behavioral therapies like bladder training and pelvic floor exercises are also highly effective and risk-free.








14 Comments
Josh Potter
Dec 17 2025Bro, I’ve been taking Benadryl to sleep for 10 years and my brain feels like mush-but I just thought I was getting old. This post hit me like a brick. Time to ditch the pills and try melatonin.
Kent Peterson
Dec 19 2025Oh please. Another fear-mongering article from the ‘everything-is-toxic’ crowd. People have been taking anticholinergics since the 1920s-and we’re still here. If you’re worried about dementia, maybe stop binge-watching TikTok and start lifting weights instead. Also, ‘ACB score’? Sounds like a pharmaceutical marketing scam.
Evelyn Vélez Mejía
Dec 20 2025There is a profound ethical dissonance in our medical infrastructure: we prescribe medications that erode the very architecture of human cognition-memory, attention, identity-while simultaneously celebrating longevity as a triumph. The dry mouth is not a side effect; it is a sacrament of neglect. We have turned pharmacology into a blunt instrument, and the brain, the most exquisite organ of consciousness, into an afterthought. This is not medicine. It is quiet violence, sanctioned by inertia and obscured by insurance formularies.
Jane Wei
Dec 22 2025I’m 68 and on oxybutynin. My mouth feels like the Sahara, but my bladder’s fine. I didn’t know it could hurt my brain. I’ll talk to my doc next week. Thanks for the nudge.
Nishant Desae
Dec 22 2025This is such an important topic, and I’m glad someone brought it up. I’ve seen so many elderly relatives in India take diphenhydramine for sleep or allergies, and no one ever questions it. We just say, 'It’s just a pill.' But the brain doesn’t lie-it remembers everything, even when we forget. I think we need more awareness in communities where doctors are scarce and pharmacists aren’t involved. Maybe local clinics can start simple handouts with the ACB scores? A little education goes a long way. And yes, mirabegron is expensive, but maybe governments can negotiate bulk prices. Our elders deserve better than foggy minds and cracked lips.
Philippa Skiadopoulou
Dec 23 2025Empirical evidence supports the association between long-term anticholinergic burden and cognitive decline. The American Geriatrics Society Beers Criteria is unequivocal. Clinicians must prioritize deprescribing. Alternatives exist. The burden of proof lies with continued use, not discontinuation.
Pawan Chaudhary
Dec 24 2025Hey, I’m from India and I’ve seen so many people use Benadryl for colds and sleep. This post opened my eyes. I’m gonna tell my auntie to switch to cetirizine. Small change, big difference!
Linda Caldwell
Dec 26 2025I switched from amitriptyline to sertraline for nerve pain and my brain fog lifted within weeks. I didn’t even realize how bad it was until it was gone. Don’t suffer in silence-ask your doctor about alternatives. You’re worth more than dry lips and forgotten names.
Anna Giakoumakatou
Dec 27 2025Oh wow. So now we’re blaming the drugs for our collective failure to learn how to sleep, pee normally, or feel emotions without chemical assistance? How quaint. Next you’ll tell me caffeine causes existential dread. Please. The real problem is a culture that outsources wellness to a pill bottle.
Sam Clark
Dec 27 2025Thank you for presenting this information with both scientific rigor and human empathy. The ACB scale is underutilized in clinical practice, and patient education remains fragmented. I encourage all clinicians to integrate ACB scoring into routine medication reviews, particularly for polypharmacy patients over 65. Shared decision-making is not optional-it is foundational to ethical care.
Jigar shah
Dec 29 2025Interesting. I’m a pharmacist’s assistant in Delhi and we don’t have ACB guidelines here. But I’ve noticed patients on oxybutynin often complain of confusion. Maybe we should start tracking this locally. Is there an open database for ACB scores I can reference?
Sachin Bhorde
Dec 31 2025Yo, this is fire. I work in a clinic and we get like 3 people a week on diphenhydramine for insomnia. I always tell em ‘try sleep hygiene’ but they’re like ‘nah bro, I need the pill’. This post? I’m printing it out and laminating it. Also, mirabegron is like $400? Damn. Maybe we can push for generics soon. #DeprescribeMore
Salome Perez
Jan 1 2026As someone who grew up in a household where every ailment was treated with a pill from the cabinet, I’m deeply moved by this. My grandmother took Benadryl for years-she forgot my name once during Christmas. We thought it was just aging. Now I know better. I’ve started sharing this with my family. Knowledge is love in action.
Meghan O'Shaughnessy
Jan 1 2026My mom’s on oxybutynin. I just called her doctor. We’re switching to mirabegron next month. Fingers crossed.