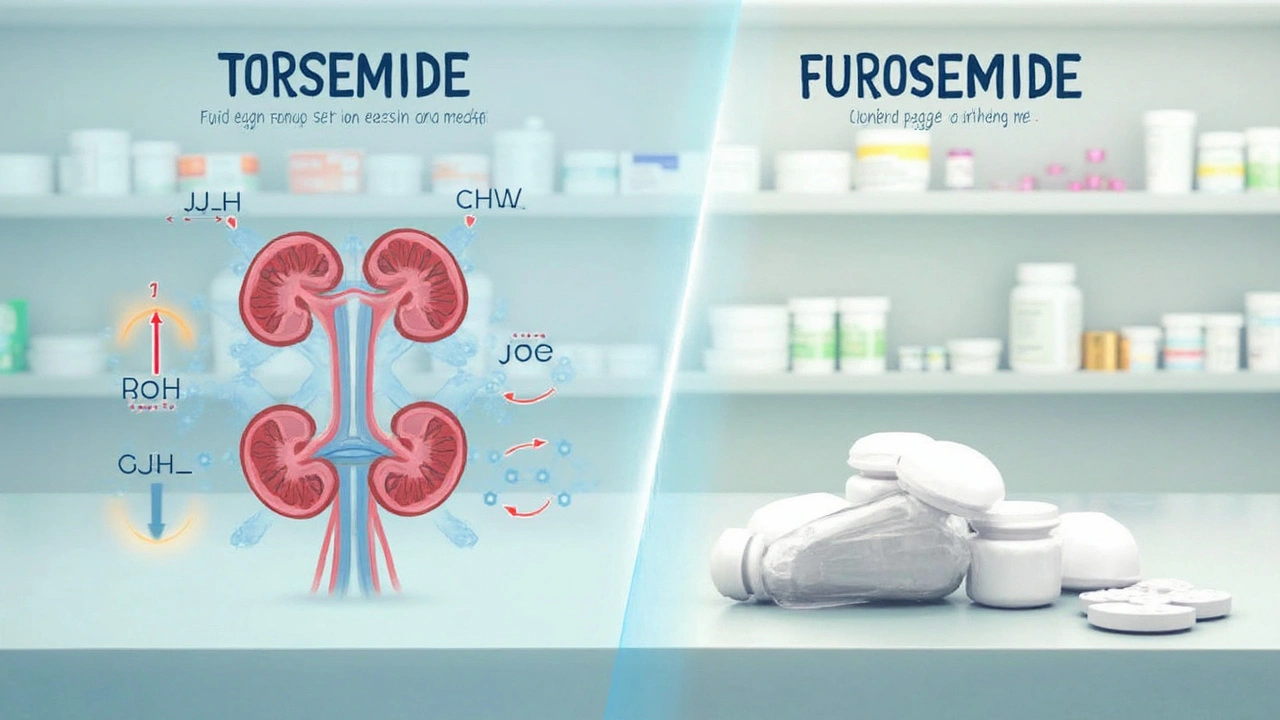
Dosing Dilemmas: Why Torsemide and Furosemide Aren’t Twins
It’s tempting to believe all diuretics are just water pills. Toss them in, flush it out, and call it a day. But life would be way too simple. Furosemide (Lasix) and torsemide both belong to the loop diuretic family, but once you get down to dosing and how the body absorbs them, the differences start stacking up. Let’s start straight away with how each drug works inside you.
Furosemide is legendary in hospitals—it’s the classic IV rescue for flooded lungs and overfilled legs. Trouble is, its oral absorption is wildly inconsistent. Pop a 40 mg Lasix and your body might only grab onto 10 mg one day, then twice that amount the next. This happens because furosemide is at the mercy of shifting stomach acidity, gut motility, and interactions with food. This unpredictability creates a kind of "pharmacologic roulette" where success, side effects, and duration can change meal to meal.
Torsemide, on the other hand, is much smoother. With a bioavailability exceeding 80%—some say as high as 90%—it’s absorbed almost the same way each time you take it, food or not. That reliable absorption means the prescribed dose matches the amount actually doing the job. Torsemide also sticks around longer: its plasma half-life averages about 3.5 hours, versus just 1.5 hours for furosemide. Steadier levels in the blood can lead to longer, more predictable relief from symptoms like swelling or breathlessness.
The magic doesn’t end there. Torsemide is about twice as potent, milligram-for-milligram, compared to furosemide. This means 20 mg of torsemide works like 40 mg of furosemide—not just for getting rid of fluid, but for dropping sodium and easing strain on the heart. For anyone juggling different doses, this conversion matters. You can switch, but you have to use the right math. Doctors sometimes underestimate this, making the swap trickier than it looks.
Still, Lasix is branded into medical culture. Emergency teams and older clinicians lean on it because it’s reliable intravenously—no waiting on the gut, no absorption wildcards. But in everyday oral use, especially in home settings, torsemide’s steady absorption and longer half-life can provide more consistent responses, meaning less guesswork for both doctors and patients.
Here’s a quick dose equivalency chart to keep things clear:
| Drug | Oral Dose | Comparable Effect |
|---|---|---|
| Furosemide | 40 mg | Baseline |
| Torsemide | 20 mg | Similar effect to 40 mg furosemide |
So, if dosing predictability matters to you—or if you’re tired of guessing if today’s pill will work—it may be time to rethink that default Lasix prescription.

Bioavailability, Onset, and Duration: The Science Behind Steady Fluid Control
Sick of bouncing between swelling and dehydration? You’re not alone. Patients with heart failure or kidney disease often ride a seesaw because their loop diuretic doesn’t quite kick in the same way every day. This is where bioavailability steps in as a real gamechanger between torsemide and furosemide.
Let’s get nerdy for a second. Bioavailability is just the fraction of a drug dose that goes from your gut into your bloodstream—ready to actually do its thing. In furosemide’s case, this number is a miserable 10%-90%, but most people sit in the 50% ballpark. On bad gut days or if you take it with a big meal, absorption can plummet—and you’ll feel it. Torsemide clocks in at 80%-90% nearly every time; it’s almost entirely absorbed, regardless of whether you just ate a pizza or skipped breakfast. This steadiness often means fewer ER visits for uncontrolled edema or overdiuresis.
But what about onset? Furosemide (oral) starts kicking in after 30-60 minutes, but IV works almost instantly. Torsemide works a bit slower, averaging 60 minutes orally, though for most chronic uses, that difference disappears. For folks who don’t need lightning-fast relief—but care about lasting power—the winner is clear. Torsemide’s half-life and duration (6-8 hours vs 4-6 hours for furosemide) mean longer coverage throughout your day and less late afternoon “swelling rebound.” Imagine not having to split doses or add an extra pill just to make it through dinner with comfortable shoes.
Here’s another twist—liver metabolism. Torsemide is processed by the liver, while furosemide relies on the kidneys. If your kidneys are struggling, furosemide can build up or stop working altogether. For people with kidney impairment, torsemide may pack more consistent punch, although physicians still keep a close eye on your labs no matter which one you take.
But there’s more: torsemide seems to help with stubborn edema that resists furosemide, possibly because of better sodium channel interaction in the thick ascending limb of the nephron. Some research has hinted this could make it a better choice for those tough cases where standard Lasix just won’t cut it.
If you like numbers, one multicenter 2022 study found patients switched to torsemide from furosemide reported “improved daily swelling control” and fewer hospital days for volume overload, especially in congestive heart failure. The number needed to treat for one fewer hospital readmission was just seven—that’s a stat worth attention in cardiology circles.
Ever checked out all your alternative to furosemide options? Torsemide’s rise shows that even old staples aren’t untouchable—and finding your best fit in a loop diuretic could make a big difference day to day.

Real-Life Outcomes: Does Torsemide Give the Edge for Heart Failure and Beyond?
Reading about numbers and half-lives is fine, but what matters when you’re trying to stay out of the hospital or just keep your ankles from ballooning? Let’s talk real-life results and why clinicians are taking torsemide seriously—sometimes switching patients even when they’ve “done fine” on furosemide for years.
Researchers have noticed something interesting: patients on torsemide report not only fewer swings in weight (a marker of fluid overload), but also better exercise tolerance and fewer high potassium surprises compared to those on furosemide. Some cardiology clinics now default to torsemide when they start diuretics for heart failure, especially if patients are older, prone to swings in kidney or gut function, or have struggled with frequent fluid build-up relapse on Lasix.
One game-changer: torsemide appears to lower certain hormone levels in the body like aldosterone, which drive heart remodeling (think thickening, scarring, and getting weaker after repeated stress). Furosemide lacks this bonus effect. In small trials, this has linked torsemide to slower heart failure progression and possibly longer survival. Some experts call this the "reverse remodeling" benefit, but don’t expect your average drug store to hype it up—most folks just want fewer symptoms and less time in the clinic.
Cost and access still matter. Torsemide is generic and pretty affordable these days, but some pharmacies don’t always keep it on the shelf. Insurance companies may also be slow to change their formularies, so some patients find out only at the register if their plan prefers Lasix or torsemide. That said, asking about torsemide is worth it—especially for anyone tired of unpredictable relief, worried about kidney ups and downs, or chasing down those mysterious "second dose" days that Lasix sometimes demands.
Here’s something you might not expect: torsemide’s longer effect means fewer bathroom runs late at night. People who take their dose in the morning often report less urgent, middle-of-the-night dashes—something that can make a surprising quality-of-life difference. It may seem minor, but anyone who’s had their sleep repeatedly wrecked by diuretics knows how huge this can be.
Nursing studies also report that patients on torsemide sometimes need lower potassium or magnesium supplementation compared to furosemide—potentially big for seniors, those with delicate kidneys, and anyone who hates taking more pills than necessary.
One last tip: if you’ve been on furosemide and feel your symptoms are barely controlled, or you need constant dose adjustments, bringing up torsemide at your next cardiology appointment could lead to a smoother ride. It’s not a one-size-fits-all world, but having the conversation—with data behind you—might save months of discomfort or extra trips to urgent care.
Loop diuretics have been basic tools for fighting heart failure and fluid overload for decades. But as research and patient experience stack up, it’s clear torsemide deserves a hard look as a more predictable, possibly more protective, and very effective alternative to furosemide. Next time your prescription comes up for renewal, it’s worth asking: is there something better than the old standby?







8 Comments
Brennan Loveless
Apr 29 2025While the buzz around torsemide is loud, we should remember that furosemide has been the frontline rescue in the trenches of American hospitals for generations, and its IV potency can’t be dismissed as mere tradition; the rapid onset of Lasix in emergency settings still saves lives when a heartbeat hangs in the balance, and the variability of oral absorption matters less when the drug is given intravenously; moreover, the cost of torsemide, though comparable, doesn’t offset the decades of familiarity clinicians have built with furosemide dosing algorithms, and any shift should be driven by hard data, not marketing hype.
Vani Prasanth
Apr 29 2025That’s a fair point about IV emergencies, but for chronic outpatient management the predictable bioavailability of torsemide can reduce the trial‑and‑error many patients endure, leading to smoother fluid control and fewer unscheduled visits.
Maggie Hewitt
Apr 29 2025Great, another pill to replace the one everyone’s already tolerating.
Mike Brindisi
Apr 29 2025People forget that furosemide’s renal clearance means dose adjustments are straightforward when kidney function drops whereas torsemide’s hepatic metabolism introduces another variable that can surprise even experienced prescribers especially in patients on multiple liver‑affecting drugs the half‑life difference also isn’t just a number it translates to real‑world timing of diuresis which some clinicians misinterpret as superiority of one drug over the other the electrolyte shifts can be similar but the pattern of potassium loss may vary and that’s why monitoring labs remains essential regardless of which loop you pick
Steven Waller
Apr 29 2025Mike, you raise many valid pharmacokinetic points, and it’s worth unpacking them one by one. First, the hepatic pathway of torsemide does indeed add a layer of complexity, but in practice the liver’s enzymatic capacity is less prone to abrupt failure than the kidneys, especially in heart failure patients where renal perfusion is already compromised. Second, the longer half‑life of torsemide translates into a steadier diuretic curve, reducing the peaks and troughs that often drive patients to awaken in the night for bathroom trips. Third, when we look at real‑world outcomes, several cohort studies have shown fewer readmissions for volume overload among patients switched to torsemide, suggesting that the theoretical pharmacology does have clinical relevance. Fourth, the issue of electrolyte management is not unique to either drug; both require diligent monitoring, yet torsemide’s more uniform absorption can make the timing of potassium shifts more predictable. Fifth, the cost differential is marginal in most formulary settings, especially now that generic torsemide is widely available, so the financial argument loses weight. Sixth, prescriber familiarity should evolve with emerging evidence rather than remain static out of habit. Seventh, the hepatic metabolism of torsemide can be modestly affected by certain CYP2C9 inhibitors, but this is a manageable interaction compared with the unpredictable reductions in furosemide absorption caused by changes in gastric pH or food intake. Eighth, patient adherence improves when dosing schedules are simpler, and the longer duration of torsemide often permits once‑daily dosing, a convenience that cannot be overstated for older adults. Ninth, the anti‑aldosterone effect observed in some trials adds a potential cardioprotective benefit beyond fluid removal. Tenth, while IV furosemide remains unmatched for acute decompensation, the transition to oral management is where torsemide shines. Eleventh, clinicians should consider individual patient characteristics-renal function, liver function, lifestyle, and comorbidities-when selecting a loop diuretic. Twelfth, education on proper dosing conversion is essential to avoid under‑ or overdosing during a switch. Thirteenth, many patients report feeling more energetic and less “weight‑fluctuation” when on torsemide, which can improve quality of life. Fourteenth, the evidence base continues to grow, and guidelines are beginning to acknowledge torsemide as a reasonable first‑line oral agent in chronic heart failure. Finally, the decision should be shared with the patient, incorporating their preferences and experiences, because the best drug is the one they will take consistently.
Puspendra Dubey
Apr 29 2025Yo fam, after reading all that geeky science I’m like “why are we still stuck on Lasix?” 😂 Torsemide feels like the underdog hero that finally gets its moment in the spotlight, and trust me, the bedside drama drops when swelling doesn’t bounce back like a bad joke.
Shaquel Jackson
Apr 30 2025Honestly, I just want less midnight bathroom trips 🙄
Tom Bon
Apr 30 2025Shaquel, the inconvenience of nocturnal diuresis is a legitimate quality‑of‑life concern. Clinical observations indicate that torsemide’s extended duration often aligns better with daytime dosing, thereby reducing the frequency of urgent nighttime voids. For patients who prioritize uninterrupted sleep, discussing a potential switch with their cardiologist may be a prudent step. Ultimately, individualized therapy remains the cornerstone of effective heart‑failure management.