Understanding Graves' Disease and Gluten Sensitivity
Before diving into the connection between Graves' disease and gluten sensitivity, it's essential to understand what these two conditions entail. Graves' disease is an autoimmune disorder that affects the thyroid gland, causing overproduction of the thyroid hormones (hyperthyroidism). This overactivity can lead to various symptoms such as weight loss, anxiety, irritability, and eye problems.
On the other hand, gluten sensitivity, also known as non-celiac gluten sensitivity (NCGS), is a condition where individuals experience symptoms similar to those with celiac disease after consuming gluten-containing foods. However, unlike celiac disease, NCGS does not cause intestinal damage. Symptoms of gluten sensitivity can include gastrointestinal issues, fatigue, and headaches.
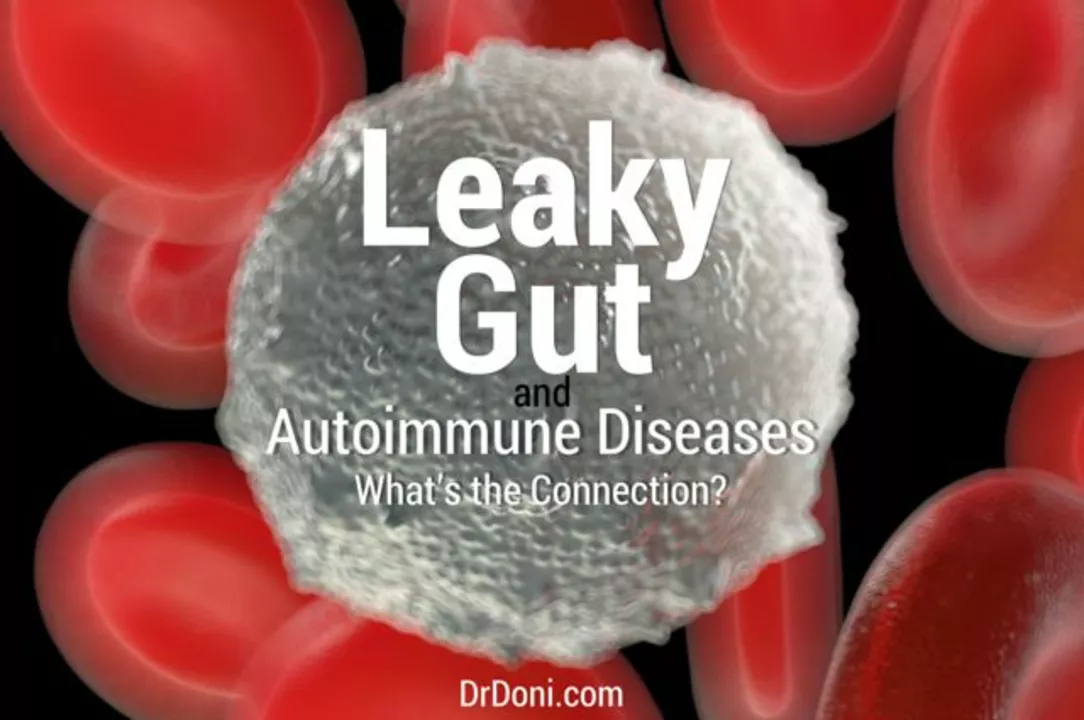
The Link Between Autoimmunity and Gluten
Research has shown that there is a link between autoimmune disorders and gluten sensitivity. This connection is primarily due to the fact that gluten can cause inflammation in the body, which can trigger an autoimmune response. In individuals with a genetic predisposition to autoimmune disorders, consuming gluten can exacerbate their condition and cause symptoms to worsen.
Notably, several studies have found that individuals with autoimmune thyroid disorders, such as Graves' disease, are more likely to have gluten sensitivity than those without such conditions. This suggests that there may be an underlying connection between these two disorders.
Graves' Disease and Gluten: A Closer Look
There is growing evidence to suggest that individuals with Graves' disease may benefit from adopting a gluten-free diet. This is because gluten can exacerbate the autoimmune response, leading to an increase in thyroid hormone production and worsening hyperthyroidism symptoms.
Moreover, some studies have shown that patients with Graves' disease who adopt a gluten-free diet experience a decrease in their symptoms and an improvement in their overall quality of life. This further supports the idea that there may be a connection between Graves' disease and gluten sensitivity.
How a Gluten-Free Diet Can Help
Adopting a gluten-free diet can help individuals with Graves' disease in several ways. First, removing gluten from the diet can reduce inflammation in the body, which may help to alleviate some of the symptoms associated with hyperthyroidism.
Second, a gluten-free diet can help to support a healthy immune system. Since Graves' disease is an autoimmune disorder, maintaining a healthy immune system is crucial in managing the condition. By eliminating gluten, individuals with Graves' disease can reduce the risk of triggering an autoimmune response and potentially improve their overall health.
Challenges of Adopting a Gluten-Free Diet
While a gluten-free diet may be beneficial for individuals with Graves' disease, adopting this way of eating can be challenging. Gluten is found in many common foods, including bread, pasta, and cereal, making it difficult to avoid completely.
Additionally, gluten-free products can be more expensive and less accessible than their gluten-containing counterparts. This can make adhering to a gluten-free diet more difficult, particularly for those on a tight budget or living in an area with limited gluten-free options.
Gluten-Free Diet Tips for Graves' Disease
For individuals with Graves' disease who are considering a gluten-free diet, there are several tips that can help make the transition more manageable. First, focus on consuming whole, unprocessed foods such as fruits, vegetables, lean proteins, and healthy fats. These foods are naturally gluten-free and can help to reduce inflammation in the body.
Additionally, be sure to read food labels carefully to identify any hidden sources of gluten. Many processed foods contain gluten, even if it is not immediately apparent from the ingredient list. By becoming familiar with common sources of gluten, individuals with Graves' disease can more effectively navigate a gluten-free diet.
Consulting a Healthcare Professional
It's essential to consult with a healthcare professional before making any significant dietary changes, particularly for individuals with Graves' disease. A healthcare provider can help to determine if a gluten-free diet is appropriate and provide guidance on how to safely and effectively implement this way of eating.
Ultimately, the connection between Graves' disease and gluten sensitivity is still being explored, and further research is needed to fully understand this relationship. However, for individuals with Graves' disease who are struggling with their symptoms, a gluten-free diet may be worth considering as part of their overall treatment plan.






16 Comments
Corey Jost
Apr 30 2023Look, I've been reading the same kind of “autoimmune‑gluten” hype for years, and honestly it feels like a trendy buzzword slapped onto a very complex set of disorders, so let’s unpack this carefully. First, Graves' disease is fundamentally a thyroid issue driven by autoantibodies that stimulate the TSH receptor, not a simple dietary consequence. Second, gluten sensitivity, while real for many, still lacks the concrete, reproducible biomarkers that celiac disease has, which means its impact on the immune system is far more ambiguous. Third, the notion that eliminating gluten will magically dial down thyroid hormone production oversimplifies the endocrine feedback loops that have been studied for decades. Fourth, the studies that claim improvement are often small, open‑label, and lack proper controls, making it hard to separate placebo from true effect. Fifth, we know that any restrictive diet can lead to nutrient deficiencies, and a gluten‑free regimen often cuts out fortified breads that supply B vitamins and iron, which are already at risk in hyperthyroid patients. Sixth, inflammation is a hallmark of many autoimmune processes, yet the link between dietary gluten and systemic inflammation in Graves' disease hasn’t been definitively proven. Seventh, some patients do report feeling better on a gluten‑free diet, but that could be due to reduced processed food intake rather than gluten per se. Eighth, clinicians should always prioritize evidence‑based treatments like antithyroid meds, radioactive iodine, or surgery before recommending broad dietary overhauls. Ninth, if a patient chooses to try a gluten‑free diet, it should be done under the guidance of an endocrinologist and a dietitian to monitor thyroid labs and nutritional status. Tenth, the gut‑thyroid axis is an emerging field, but we are still piecing together how gut permeability, microbiota, and thyroid autoimmunity interact. Eleventh, anecdotal reports do not equal clinical consensus, and the medical community remains divided. Twelfth, we have to be cautious about commercial interests pushing gluten‑free products as a cure‑all for everything from IBS to thyroid disease. Thirteenth, the key takeaway is that while a gluten‑free diet might benefit some individuals, it is not a universally proven therapy for Graves' disease. Fourteenth, patients should focus on a balanced diet rich in whole foods, adequate protein, and essential micronutrients. Fifteenth, regular monitoring of thyroid function tests remains essential regardless of dietary changes. Finally, keep an eye on emerging research, but don’t jump on the gluten‑free bandwagon solely based on a few preliminary studies.
Nick Ward
May 1 2023Totally get how overwhelming all the diet advice can be ☺️. If you’re thinking about cutting gluten, just start by swapping out the obvious stuff like bread and pasta for veggies and GF grains, and keep an eye on how you feel.
felix rochas
May 1 2023Whoa!!! This is exactly what the shadow‑farmers want you to believe!!! Gluten is the hidden puppet‑master pulling the strings of every autoimmune condition-yes, even Graves'!!! They hide the truth behind "scientific studies" that are just smoke screens!!! Don't be fooled-read between the lines, the truth is out there!!!
inder kahlon
May 2 2023From a clinical perspective, the first step is to confirm true gluten sensitivity with a proper challenge test. If confirmed, a gradual gluten‑free transition while monitoring thyroid levels is advisable.
Dheeraj Mehta
May 3 2023Hey there! 😊 Switching to gluten‑free can be a good experiment-just stay positive and listen to your body. You got this!
Oliver Behr
May 4 2023Interesting read-it's always fascinating to see how dietary trends intersect with endocrine health.
Tiffany W
May 5 2023From a pathophysiological standpoint, the purported "gluten‑Graves nexus" lacks robust mechanistic elucidation, rendering the discourse riddled with methodological opacity and speculative extrapolation.
Rajeshwar N.
May 6 2023Honestly, the whole gluten‑free hype for Graves' feels like another band‑wagon trend. People love quick fixes, but the evidence just isn’t there, so why chase a fad?
Louis Antonio
May 7 2023Yo, I tried cutting gluten once and felt fine, but then I missed pizza. So yeah, if it works for you, do it, but don’t act like it’s the holy grail.
Kyle Salisbury
May 8 2023Not sure how much gluten matters, but a balanced diet never hurts.
Angie Robinson
May 9 2023People love to blame gluten for everything, even when the data says otherwise. Stop scapegoating food and focus on actual treatment protocols.
Emmons Kimery
May 9 2023Great discussion! 🌟 If you decide to try a gluten‑free plan, make sure you get enough fiber from fruits and veggies, and keep those thyroid labs checked. 👍😊
Mimi Saki
May 10 2023Sending positive vibes your way! 🌈 Remember, any diet change should be paired with good medical advice. 💪
Subramaniam Sankaranarayanan
May 11 2023Let me set the record straight: gluten sensitivity is a real entity, but conflating it with Graves' disease without rigorous double‑blind studies is scientifically unsound. The immunological pathways differ-autoantibodies against the TSH receptor drive Graves', whereas gluten triggers innate immune activation via gliadin peptides. Until we see reproducible evidence showing that gluten elimination lowers thyroid‑stimulating immunoglobulins, any claim remains speculative. Moreover, the nutritional ramifications of a gluten‑free diet can inadvertently exacerbate deficiencies in selenium or iodine, which are crucial for thyroid health. In practice, a personalized approach-testing for celiac markers, assessing gut permeability, and monitoring thyroid function-offers the most rational path forward.
Kylie Holmes
May 12 2023Hey everyone! 🎉 If you’re feeling stuck, give the gluten‑free experiment a shot for a few weeks and track your symptoms. You might be surprised by the results! 🚀
Jennifer Wees-Schkade
May 13 2023From a therapeutic perspective, dietary changes should complement, not replace, standard Graves' disease management. Always coordinate with your endocrinologist before making major diet shifts.