If you've ever thought about how your birth control choice might affect your vaginal health, you're not alone. Bacterial Vaginosis (BV) can be a bit of a thorn in the side for many women, and the contraceptive method you pick might just tip the balance one way or another. This delicate ecosystem is easily disrupted, and the wrong contraceptive can sometimes make things a bit tricky.
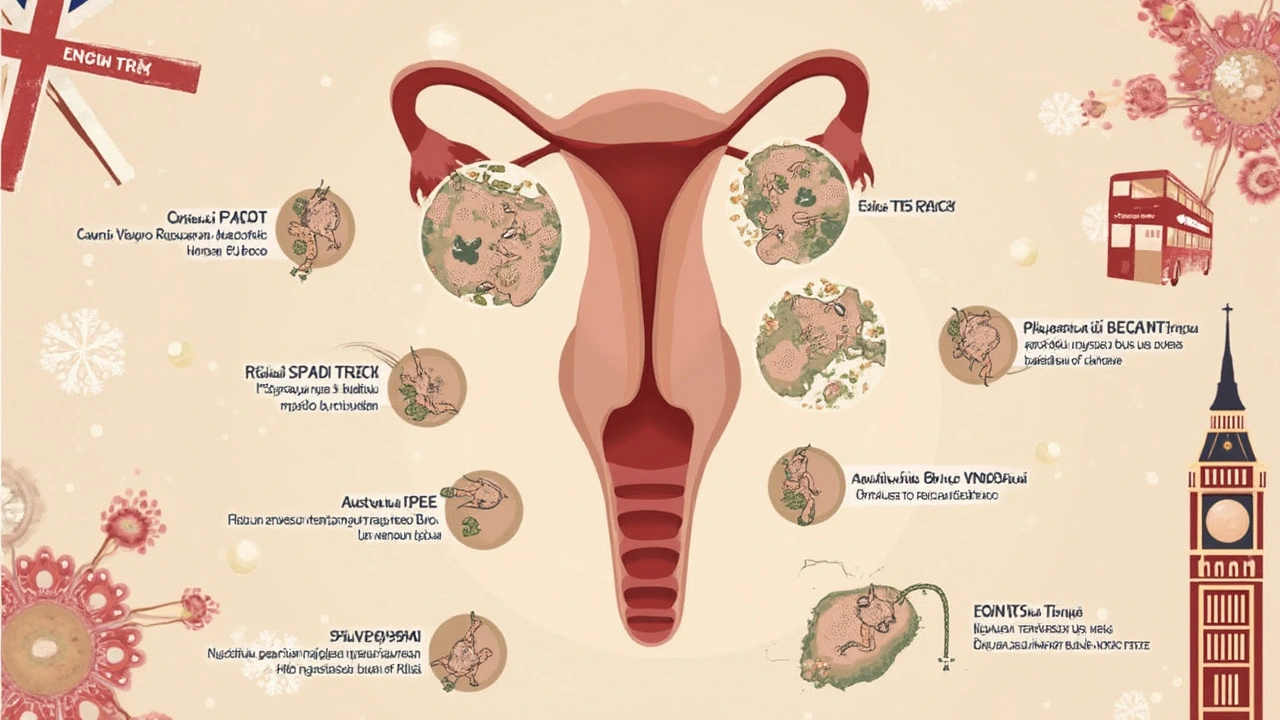
When we're talking about BV, it’s about understanding that fine line between good bacteria doing their thing and harmful bacteria trying to run the show. So, how does your chosen form of birth control come into the mix? It turns out, some methods might have a surprising impact on keeping things balanced down there. Whether it's the hormones in the pill or the physical barrier of a diaphragm, each one plays its own role.
Diving into effective contraceptive methods for those dealing with BV, it's about finding what's just right. You've got options, and knowing which ones help rather than hinder can significantly affect your comfort and health. But don't worry, it's not all about meds and hard choices—sometimes little lifestyle tweaks can make a world of difference. We'll explore those too, so you can have a happy and healthy experience without the BV blues overshadowing everything else.
- Understanding Bacterial Vaginosis
- The Impact of Contraception on Vaginal Health
- Best Contraceptive Methods for BV
- Lifestyle Tips for Managing BV
- When to Seek Professional Help
Understanding Bacterial Vaginosis
Bacterial Vaginosis, or BV, sounds fancy, but it’s really about balance. Think of your vagina as a bustling city of bacteria. Normally, the good bacteria, especially lactobacilli, keep things running smoothly. But sometimes, harmful bacteria start taking over, and that’s when BV shows up. It's one of the most common vaginal infections among women of childbearing age.
So, how can you tell if you’ve got BV? The most obvious sign is a fishy-smelling discharge, especially noticeable after sex. You might also notice a change in color, like a grayish hue, and even some itchiness or burning, though it doesn't always cause these symptoms.
The cause of BV isn’t linked to poor hygiene as people sometimes think. Instead, it's more about things that disrupt the normal bacterial community. This can include everything from washing with harsh soaps, douching, to even having new or multiple sexual partners. It’s also worth knowing that using an IUD has been associated with BV in some cases.
When it comes to numbers, BV affects nearly 30% of women between ages 15 and 44 in the United States. It can sometimes feel like it’s playing hard to get rid of because it tends to come back. But the good news is, it’s treatable and often with simple measures. Still, leaving it unchecked isn't a great plan since it can lead to complications like an increased risk of STIs and issues during pregnancy.
Getting a handle on BV means paying attention to your body and catching changes early. Regular check-ups with your healthcare provider can help in managing it and making sure it doesn’t mess with your life more than it has to.
The Impact of Contraception on Vaginal Health
It's a question that pops into mind more often than you’d think: how does my choice of contraception affect my vaginal health? When we look at Bacterial Vaginosis (BV), the type of contraception you use can play a significant role in either helping or complicating things.
Hormonal methods like the pill, patch, or ring change your hormone levels, which can sometimes mess with the natural balance of bacteria in the vagina. This might not spell trouble for everyone, but if you're someone who deals with BV, it could be worth considering. These hormones can alter the vaginal pH, potentially encouraging the growth of bacteria that lead to BV.
On the flip side, non-hormonal methods might offer a different set of challenges and benefits. For example, using a condom provides a physical barrier that doesn’t affect your hormonal balance but can sometimes lead to irritation or allergies for some folks using latex. You might look into latex-free options if that's the case. Also, diaphragms and cervical caps need to be used with spermicide, which can also affect vaginal bacterial balance.
- Birth Control Pills: Can change vaginal flora due to hormonal shifts.
- Condoms: Provide a barrier, but check for potential latex allergies.
- IUDs: Non-hormonal types like copper might be less disruptive although individual experiences may vary.
- Spermicides: Often used with diaphragms, can alter the natural pH.
While it’s clear that contraception and vaginal health are connected in various ways, there’s no one-size-fits-all answer. Listening to your body and discussing with your healthcare provider will be key in finding what works best for you.
If you've ever wondered which options might make BV better or worse, now you’ve got a bit more insight. Remember, the right choice is about what fits best for your body and lifestyle, so don’t hesitate to experiment and talk to experts until you are happy with your decision.

Best Contraceptive Methods for BV
Picking a birth control method when you're dealing with Bacterial Vaginosis can seem like a maze. The goal here is to choose something that keeps your vaginal health in check without making BV worse. What works well for one person might not be the best for another, so a bit of personalization goes a long way. Let's break down some options.
First up, hormonal contraceptives like the pill, patch, or ring. While these are convenient and effective, they can sometimes alter your hormone balance, potentially impacting your risk of BV. Some women find they do just fine on these, while others notice a flare-up in symptoms. Keeping a health diary might help you spot any patterns related to your BV.
Barrier methods such as condoms or diaphragms are often seen as BV-friendly. They don't mess with your hormones and provide necessary protection. Plus, they help prevent other infections, which is a win-win if you're trying to maintain that delicate balance of flora.
If you’re leaning towards an intrauterine device (IUD), the copper IUD might be a good pick. Unlike hormonal IUDs, the copper one won't alter hormone levels. It's a popular choice for those who want long-term protection without the hormonal side effects. However, it's always good to chat with a healthcare provider about your specific situation, as some women report an increase in discharge when using certain types of IUDs.
For people considering long-term methods like implants or hormonal shots, bear in mind the potential hormonal impact. While they’re highly effective, if you notice any BV flaring up, it might be worth discussing alternatives with your doctor.
Ultimately, finding the best contraceptive method for BV involves a bit of trial and error. Partnering with a healthcare provider to monitor any changes can make all the difference in keeping both your birth control needs and BV management on track.
Lifestyle Tips for Managing BV
Dealing with Bacterial Vaginosis? It’s not the most fun thing, but thankfully, there are some lifestyle tweaks you can make that might help manage it. Let’s talk about some practical stuff you can do to keep your vaginal health in check.
First up, let’s chat about the basics of hygiene. Keeping the vaginal area clean and dry is key, but don't go overboard. You might think douching is doing good, but it can actually disrupt the natural balance of good bacteria in your vagina. Stick to mild, unscented soap and warm water, and you're golden. Here’s a tip: wear breathable cotton underwear. It helps keep things airy, reducing moisture buildup that can invite bad bacteria.
Diet plays a surprising role too. Have you heard of probiotics? These friendly bacteria can support your gut health and might help maintain the balance down there. Yogurt with live cultures or a probiotic supplement can be a great addition to your daily routine. You might want to limit sugar and refined carbs as well—they can sometimes trigger those unwanted changes.
Let’s look at some points more closely:
- Avoid Scented Products: Scented tampons, sprays, or pads might seem like a fresh idea, but they're a big no-no for vaginal health.
- Wear Loose-Fitting Clothing: Think about those skinny jeans. Every day might not be the best idea; give your body room to breathe.
- Regular Check-Ups: Even if you’re not feeling any symptoms, regular visits to your healthcare provider can catch potential issues early.
If you're constantly struggling with BV, it might be a hint to check in with what you're eating or using down there. Don’t hesitate to seek professional help when things don’t seem to improve. A healthcare provider can offer personalized advice, ensuring you're not guessing in the dark.
With these simple changes, you might find that managing BV becomes a bit more manageable. Remember, it’s about feeling good and comfortable in your own skin, rather than letting BV spoil the party.
When to Seek Professional Help
Dealing with Bacterial Vaginosis can sometimes feel like walking a tightrope. Most of the time, you might manage just fine on your own with a bit of vigilance and good habits. But there are moments when getting a professional on board is the smart move. Here’s how you can know when it’s the right time to drop in at the doctor’s office.
If you're noticing persistent or severe symptoms—like a strong, fishy odor or unusual discharge—it’s definitely time to chat with someone who knows the ropes. BV shares symptoms with other infections, like yeast infections or even STIs, so it’s crucial to get the correct diagnosis. A professional will be able to pinpoint exactly what's going on, ensuring you don’t start any unnecessary or ineffective treatments.
Also, if you’ve tried treating Bacterial Vaginosis on your own but it keeps coming back, it’s another clear signal to see a doctor. Recurring BV could suggest an underlying issue, or it might be a sign that your current birth control method isn’t doing you any favors. A healthcare professional can work with you to find a contraception option that’s in harmony with your body.
And if you’re pregnant, experiencing BV symptoms is a definite red flag. Untreated BV during pregnancy can increase the risk of complications, including preterm birth or low birth weight. In such cases, professional intervention is not just advisable, it's essential for both you and your baby’s well-being.
All in all, keeping an open line of communication with your healthcare provider when dealing with BV isn't about alarmism; it's about staying informed and healthy.








6 Comments
Jennifer Ferrara
Apr 4 2025When one reflects upon the delicate symbiosis that governs the vaginal microbiome, it becomes evident that any perturbation, be it hormonal or mechanical, may precipitate an imbalance. The intricate dance between lactobacilli and opportunistic organisms is mediated by pH, nutrient availability, and immune modulation, each of which can be subtly altered by contraceptive choices. Hormonal contraceptives, such as oral tablets, patches, or vaginal rings, introduce exogenous estrogen and progestin, which may shift the vaginal environment towards a more alkaline state, thereby fostering the proliferation of Gardnerella vaginalis. Conversely, non‑hormonal barriers, including condoms and diaphragms, typically preserve the endogenous hormonal milieu but may introduce irritants or allergens that disrupt the epithelial barrier. Empirical studies have demonstrated a modest increase in BV recurrence among users of certain combined oral contraceptives, though the evidence remains heterogeneous. It follows that an individualized assessment, taking into account personal history of recurrent BV, sensitivity to latex, and lifestyle factors, is paramount in selecting an optimal method. Maintaining meticulous hygiene, avoiding douching, and employing probiotic‑rich diets are ancillary strategies that complement the primary contraceptive decision. In clinical practice, a thorough dialogue between patient and provider, wherein the potential ramifications on vaginal flora are explored, can mitigate unintended consequences. The copper IUD, devoid of hormonal influence, presents a viable long‑term alternative for those seeking to minimize microbial disturbance, yet its mechanical presence may still alter discharge patterns. Ultimately, the guiding principle should be to align contraceptive efficacy with the preservation of microbial equilibrium, thereby reducing the incidence of BV flares. By conscientiously documenting symptom trajectories in relation to contraceptive switches, patients empower themselves with data that can inform future choices. The integration of probiotic supplementation, particularly strains of Lactobacillus crispatus, has shown promise in restoring a protective lactobacilli dominance. Moreover, awareness of the potential for spermicide to disrupt pH underscores the importance of selecting spermicide‑free barrier methods when appropriate. While no single method guarantees immunity from BV, a judicious combination of medical insight, personal observation, and lifestyle modulation yields the most favorable outcome. In sum, the convergence of hormonal influence, mechanical factors, and individual susceptibility dictates the nuanced relationship between contraception and bacterial vaginosis. Recognizing this complexity equips both clinicians and patients to navigate toward a harmonious balance.
Terry Moreland
Apr 12 2025I totally get how frustrating BV can be, especially when you’re trying to pick a birth control method that works for you. It helps to keep a simple log of any changes you notice after switching methods, like more discharge or a different smell. If you see a pattern, bring it up at your next appointment – your doc can suggest alternatives that might be gentler on your flora. Also, make sure you’re using fragrance‑free products and breathable cotton underwear to give your body the best environment possible. Small steps like these often make a big difference in how you feel day‑to‑day.
Abdul Adeeb
Apr 21 2025It is essential to acknowledge that the interplay between contraceptive hormones and vaginal pH constitutes a scientifically documented phenomenon. Studies indicate that estrogen‑dominant formulations can elevate vaginal alkalinity, thereby encouraging the growth of anaerobic bacteria associated with bacterial vaginosis. Conversely, copper intrauterine devices maintain hormonal homeostasis, reducing the likelihood of such dysbiosis. Nevertheless, individual variability mandates personalized clinical assessment before prescribing any specific method. In practice, a thorough anamnesis combined with microbiological testing yields the most reliable guidance.
Abhishek Vernekar
Apr 29 2025Hey there! Just wanted to add that staying hydrated and eating plenty of fermented foods can give your good bacteria a real boost. Yogurt with live cultures or kefir are tasty ways to support the lactobacilli down there. If you decide to go with condoms, try the non‑latex options if latex irritation has ever been an issue for you. And don’t forget to change your pads frequently during heavy flow days – moisture can be a breeding ground for unwelcome microbes. Keep an eye on any recurring symptoms and let your healthcare provider know early on. A proactive approach really pays off in the long run.
Val Vaden
May 7 2025Seriously, the copper IUD is the way to go 😒
lalitha vadlamani
May 15 2025One must not be deceived by the allure of convenience when it veils a potential disruption of the body's natural order. The moral imperative lies in choosing a contraceptive that upholds, rather than undermines, the delicate microbial equilibrium. To champion this cause, we must demand rigorous research and transparent discourse from the medical community. Only then can we safeguard women's health against the insidious advance of bacterial vaginosis.